Abstract
Accurate prognostication is challenging in the setting of SARS-CoV-2, the virus responsible for COVID-19, due to rapidly changing data, studies that are not generalizable, and lack of morbidity and functional outcomes in survivors. To provide meaningful guidance to patients, existing mortality data must be considered and appropriately applied. Although most people infected with SARS-CoV-2 will recover, mortality increases with age and comorbidity in those who develop severe illness.
Key Words: Prognosis, SARS-CoV-2, COVID-19, palliative care, prognostication, proactive planning
Introduction
Palliative care clinicians aim to equip patients and families with accurate prognostic information to align medical interventions with patient priorities. Accurate prognostication is particularly challenging in the case of SARS-CoV-2, the virus responsible for COVID-19, due to several factors including incomplete and rapidly changing data, challenges in generalizing data between regions, and lack of morbidity and functional outcomes in survivors. The high transmission rate of this virus has led to a worldwide pandemic. This has increased lay discussion about the risk of mortality the virus carries, particularly for older adults and people with comorbid conditions such as diabetes, coronary artery disease, chronic respiratory disease, cancer, or hypertension.1 As we work to provide accurate and personalized recommendations to our patients, we must closely examine available data and apply to our patient populations.
Severity of Illness
Despite a large number of people being infected, over 3.1 million people worldwide as of April 29, 2020, most of those infected are asymptomatic or have mild symptoms. On April 1, the World Health Organization reported 25% of SARS-CoV-2+ patients in Wuhan, China, were asymptomatic and never developed symptoms.2 Many patients who have increased risk of severe disease, including those >65 years old and those with comorbidities of heart disease, diabetes, lung disease, asthma, or obesity, recover. Initial data suggest that only 20% of those with confirmed COVID-19–positive test go onto have severe symptoms.3 However, for those who develop severe illness, mortality increases with age and comorbidity.
Overall Mortality
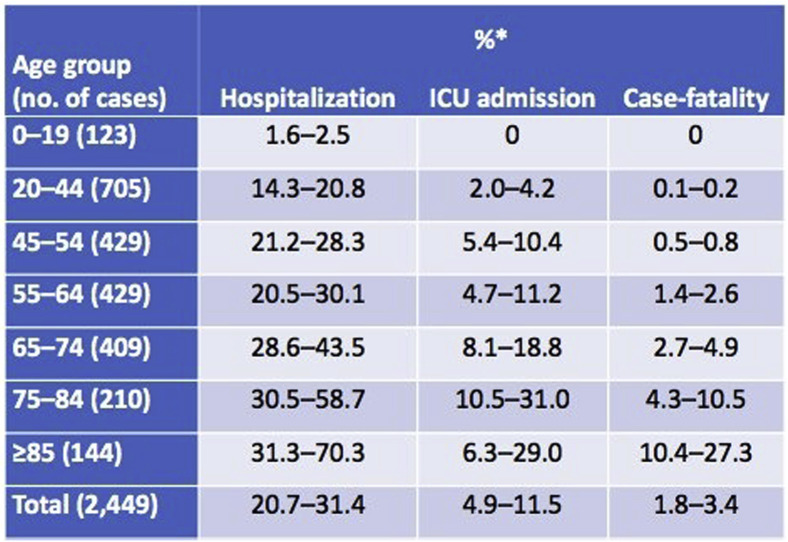
The case fatality rate (CFR), the number of people who die divided by the number of people known to be infected with the virus, is widely variable around the world. With numbers as low as 0.7% in Germany, where testing is prevalent, up to 10.7% in Italy for a global fatality rate of 4.7% as of April 6, 2020.4 Older adults are disproportionally affected by COVID-19. Data from the Washington Department of Health show that while one in 10 confirmed cases were in adults greater than 80 years of age, this age group accounted for 54% of all deaths.5 This aligns with nationwide CFR that increases with older age, with rates up to 27.3% in those >85 years as reported by the Centers for Disease Control.6 (Figure 1 ). When widespread testing is more available worldwide, it is expected a more accurate CFR will be lower than currently reported.
Fig. 1.
United States case fatality rate February 12 to March 16, 2020
Hospitalized Patients
National data on frequency of hospitalization of infected patients are lacking as of this publication due to inconsistent reporting methods. Individual states, however, report similar hospitalization rates via The COVID Tracking Project, revealing rates ranging from 8% to 24% with higher hospitalization frequency correlating directly with age.7 Of those who were sick enough to require hospitalization in one hospital in Wuhan, China, 28% (54/191) died.8 Older age, higher Sequential Organ Failure Assessment score, and elevated d-dimer at admission were risk factors associated with death. Northwell Health in the New York City area demonstrated similar mortality in their hospital system, with 553 deaths out of 2634 (20.9%) patients hospitalized March 1 through April 4, 2020.9 However, these data only include those who were discharged alive or died. Given that most patients (3066 of the 5700 patients) remained hospitalized, the actual mortality rate may be higher or lower than this one-time snapshot.
Intensive Care
Of patients who were sick enough to require intensive care in a Wuhan, China hospital, 61.5% (32/52) died in hospital with a median duration of seven days from admission to ICU until death.10 Patients with acute respiratory distress syndrome and older adults were more likely to die, with a median age of 64.6 years of those who died and a median age of 51.9 years for survivors. Similarly, 67% (14/21) of patients in a Washington state hospital, the majority of which came from a nursing home, died after intensive care admission, and 24% remained critically ill at the time of reporting.11 An Italian cohort study demonstrated lower mortality, at 26% (405/1581).12 However, the true mortality is likely significantly higher given that 58% (920/1581) of patients remained in the intensive care unit at the time of the publication. As noted with previous studies, mortality significantly worsened with increasing age (Figure 1).
Intubated Patients
Patients who require mechanical ventilation demonstrate very high mortality rates, ranging from 81% to 97%.10 , 13 It is not yet clear whether mortality in the New York system Northwell Health may be different. In their data set of 1151 patients who were mechanically ventilated, 3% were discharged alive, 25% had died, and 72% were still in the ICU.9 Therefore, we can estimate the mortality is somewhere between 25% and 97%. The Intensive Care National Audit and Research Center in the U.K. documented a lower mortality rate when including noninvasive positive pressure ventilation. In their population, for patients who required advanced respiratory support, inclusive of BIPAP, CPAP, and mechanical ventilation and extracorporeal respiratory support, 67% were dead at the end of their critical care stay.14 Caution is warranted when looking at these data as they are biased toward reporting patient outcomes of those who died or recovered quickly and may underreport those with a long duration of mechanical ventilation.
Survival After Cardiac Resuscitation
A single study has demonstrated poor outcomes for COVID-19+ patients who require in-hospital cardiac resuscitation. Overall 30-day survival for the 136 patients who underwent in-hospital resuscitation in the setting of COVID-19 was only 2.9%.15 Only one of the 136 patients survived with a favorable neurologic status (Cerebral Performance Category [CPC] score of 1 or 2. As a comparison, previous data before the COVID-19 pandemic showed that the overall survival to discharge after treated in-hospital cardiac arrest in those without is approximately 18%, with about half of those patients neurologically intact or with only mild neurologic deficits at discharge (CPC of 1).16
Pediatric Patients
In a U.S. study of COVID-19 cases from 50 states and four territories reported on April 2, 2020, 1.7% were persons aged <18 years despite this age group accounting for 22% of the U.S. population.17 , 18 A portion of this population required hospitalization, estimated at 5.7%–20% while 0.58%–2.0% required ICU admission. This is consistent with previous reports that COVID-19 illness often has a mild course among younger patients.19 Although symptoms of COVID-19 were typically less severe than those of adult patients, young children, particularly infants, were vulnerable to infection in this study, consistent with data from the Chinese Center for Disease Control.19 Patients aged 15–17 years were the most common age group to be infected, accounting for one of three cases, but hospitalization was most common in patients aged less than one year. One out of 728 children confirmed to have COVID-19 died in the China study, a 14-year-old boy.19 Three out of 2572 children died in the U.S. study.17
Proactive Planning
In this dynamic medical environment, it is incumbent on palliative care, primary care, emergency and critical care clinicians to incorporate existing data with prior knowledge to inform accurate prognostication and alignment of care with patient goals. The aforementioned studies, in combination with existing knowledge about the impact of performance status, pneumonia severity, comorbidities, and age, can be utilized to develop a prediction of the odds of morbidity and mortality for patients seeking guidance. As in non-COVID times, our aim is to understand the priorities of our patients, including their minimal acceptable state of being. Only then can we utilize current and past findings to help them understand the likelihood they will maintain an acceptable state should they get infected with SARS-CoV-2 and require hospitalization or intensive care.
Conclusion
While most patients infected with SARS-CoV-2 will recover, those who get severe illness and require hospitalization, intensive care, intubation, and cardiac resuscitation have escalating levels of mortality. Evolving data should be viewed as preliminary and used to supplement existing constructs.
Disclosures and Acknowledgments
The authors report no conflicts of interest.
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Ashour H.M., Elkhatib W.F., Rahman M.M., Elshabrawy H.A. Insights into the recent 2019 novel coronavirus (SARS-CoV-2) in light of past human coronavirus outbreaks. Pathogens. 2020;9:186. doi: 10.3390/pathogens9030186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Orgnization Press Conference. https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-01apr2020-final.pdf?sfvrsn=573dc140_2 Available from. Accessed April 18, 2020.
- 3.Xu Z., Li S., Tian S., Li H., Kong L.-Q. Full spectrum of COVID-19 severity still being depicted. Lancet. 2020;395:947–948. doi: 10.1016/S0140-6736(20)30308-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Omer S.B., Malani P., Del Rio C. The COVID-19 pandemic in the US: a clinical update. JAMA. 2020 doi: 10.1001/jama.2020.5788. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health, state of Washington website. https://www.doh.wa.gov/Emergencies/Coronavirus Available from.
- 6.Centers for Disease Control Morbidity & Mortality Weekly Report March 27th 2020. https://www.cdc.gov/mmwr/index.html Available from.
- 7.The COVID Tracking Project. https://covidtracking.com/data Available from.
- 8.Zhou F., Yu T., R Du Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richardson S., Hirsch J.S., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323:2052-2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arentz M., Yim E., Klaff L. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grasselli G., Zangrillo A., Zanella A. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiss P., Murdoch D.R. Clinical course and mortality risk of severe COVID-19. Lancet. 2020;395:1014–1015. doi: 10.1016/S0140-6736(20)30633-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Intensive care national Audit & Research Center April 24th report. https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports Available from. Accessed April 18, 2020.
- 15.Shao F., Xu S., Ma X. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18–23. doi: 10.1016/j.resuscitation.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ebell M.H., Jang W., Shen Y., Geocadin R.G., Get With the Guidelines–Resuscitation Investigators Development and validation of the Good Outcome Following Attempted Resuscitation (GO-FAR) score to predict neurologically intact survival after in-hospital cardiopulmonary resuscitation. JAMA Intern Med. 2013;173:1872–1878. doi: 10.1001/jamainternmed.2013.10037. [DOI] [PubMed] [Google Scholar]
- 17.CDC COVID-19 Response Team Coronavirus disease 2019 in children- United States, February 12-April 2, 2020. Morbmortal Wkly Rep. 2020;69:422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bridged race population estimates. US Department of Health and Human Services, CDC; Atlanta, GA: 2020. https://wonder.cdc.gov/bridged-race-population.html Availble from. Accessed April 18, 2020. [Google Scholar]
- 19.Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 Among Children in China. Pediatrics April 2020:e20200702. [DOI] [PubMed]