Sir,
Coronavirus disease 2019 (COVID−19) is a highly contagious disease that has the potential to spread rapidly among healthcare workers (HCWs) and in the hospital setting [1]. A critical epidemiological measure that modulates the early stage of a viral outbreak is access to adequate equipment, which is crucial for the protection of HCWs [2]. However, the present pandemic is distinguished by a huge shortage of personal protective equipment [3], especially in Italy where the rate of COVID−19 among HCWs is high. The Italian Government strengthened prevention and restraint strategies, including self-quarantine, and restricted the movements of residents, first in Lombardy and subsequently across the entire country [4]. During the early phase of the pandemic, routine screening for COVID−19 was easily accessible for politicians and football players, even in the absence of overt symptoms, yet by the end of March 2020, no specific serial testing strategy had been implemented for early recognition of potentially infected HCWs [5]. It was expected that initial reports from China during the early epidemic phase might have increased global awareness among healthcare providers of the high risk of infection in the hospital setting. Unfortunately, in Lombardy, the epicentre of the Italian outbreak, COVID−19 had caused 42 deaths among physicians by 1st April 2020 [6]. International media and Italian politicians are now raising the question: are we doing enough to protect HCWs during this pandemic?
Currently, no published studies have focused specifically on the prevalence of COVID−19 among HCWs. Hence, we investigated the proportion of HCWs among consecutive patients with COVID−19 admitted to a tertiary care hospital in Lombardy in the early stage of the European outbreak.
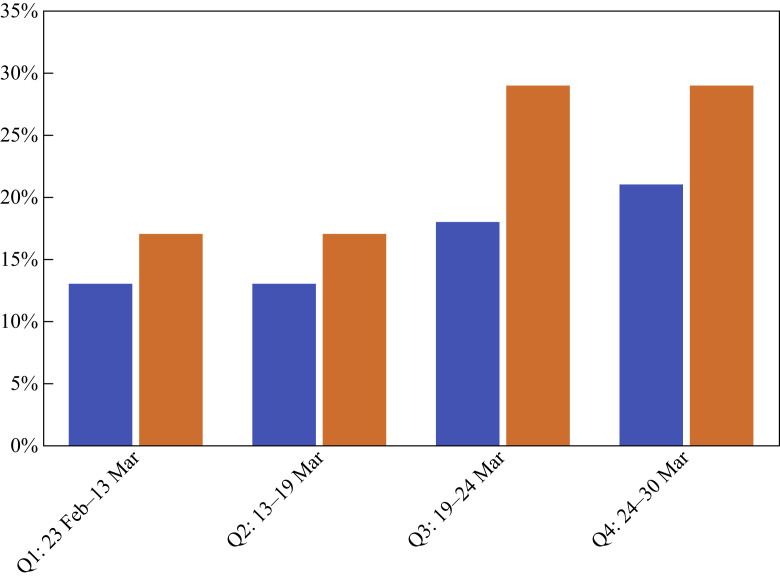
Our analysis included 400 consecutive adults admitted to the study hospital with confirmed COVID−19 by 30th March 2020. We grouped our population into quartiles, each made up of 100 patients, in order to evaluate the variation in infection rate over time (Quartile 1: 23rd February−13th March 2020; Quartile 2: 13th March−19th March 2020; Quartile 3: 19th March−24th March 2020; Quartile 4: 24th March−30th March 2020). We evaluated the percentage of infected HCWs in the total population and among active workers, excluding retired patients. Sixty-five patients were HCWs, representing 16.3% of the total study population. All HCW cases had been exposed in Lombardy. According to the latest report of the Italian Statistical Institute, the overall proportion of HCWs is estimated to be 1.87% of the adult population; therefore, the proportion of HCWs in our series is approximately nine-fold higher than expected. Our sample included 120 retired patients; if we consider active workers alone, 65 of 280 cases were HCWs (23.2%). As the behaviours and control measures of HCWs were in constant flux, we estimated the proportion of HCWs infected over time until the end of March 2020, 40 days after the first Italian patient was registered. Figure 1 shows that the transmission rate in HCWs has increased persistently, affecting up to 29% of HCWs in the active worker population.
Figure 1.
Healthcare workers (HCWs) with coronavirus disease 2019 (COVID-19). The transmission rate in HCWs increased persistently over time, with up to 22.7% and 33.3% of HCWs affected among the total study population and active workers, respectively. Blue bars, HCWs with COVID-19 from total study population; orange bars, HCWs with COVID-19 from active workers population.
Up to 30th March 2020, general data provided from the Italian Istituto Superiore di Sanità showed that among 94,312 confirmed cases of COVID−19, 8956 were HCWs (9.49%; compared with 16.3% in the study population). Up to 24th February, 2020, China reported that 2055 of 77,262 cases of COVID−19 were HCWs (2.66%) [7]. Despite increased awareness of the risk of infection, the prevalence of COVID−19 seems to be three-fold higher in Italian HCWs than in Chinese HCWs, who were the first to face the outbreak.
This analysis indicates that the current Italian outbreak of COVID−19 is having a considerable impact on local HCWs. Despite government efforts to limit the spread of severe acute respiratory syndrome coronavirus−2, the lack of standardized protocols to screen HCWs across Italy, even during this later phase of the pandemic, may induce the resumption of new outbreaks in the hospital setting, especially as routine activities will be restored soon. Although this study was limited to a single nation, the data highlight the urgent need to implement serial testing and appropriate control measures among HCWs, and may also provide some valuable guidance for other countries facing COVID−19.
Conflict of interest statement
None declared.
Funding sources
None
References
- 1.McMichael T.M., Currie D.W., Clark S., Pogosjans S., Kay M., Schwartz N.G. Epidemiology of COVID-19 in a long-term care facility in King County, Washington. N Engl. J Med. 2020 doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020 doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 3.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages – the need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med. 2020 doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 4.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020 doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chow E.J., Schwartz N.G., Tobolowsky F.A., Zacks R.L.T., Huntington-Frazier M., Reddy S.C. Symptom screening at illness onset of health care personnel with SARS-CoV-2 infection in King County, Washington. JAMA. 2020 doi: 10.1001/jama.2020.6637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.In memoriam: healthcare workers who have died of COVID-19. Medscape. 2020 https://www.medscape.com/viewarticle/927976#vp_1 [Google Scholar]
- 7.Wang J., Zhou M., Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]