Abstract
Objectives:
Individuals with a childhood maltreatment history tend to have various psychological symptoms and impaired social functioning. This study aimed to investigate the related therapeutic effects of a mindfulness-based intervention in this population.
Methods:
We analyzed self-report questionnaire scores of the Mindful Attention Awareness Scale (MAAS), Non-Attachment Scale (NAS), Adult Rejection Sensitivity Questionnaire (A-RSQ), Interpersonal Reactivity Index (IRI), PTSD CheckList (PCL), and Anxiety Sensitivity Index (ASI), from 16 (3 males) young adults (age range 22–29) with mild to moderate childhood maltreatment, compared to 18 matched participants (6 males) on a waiting list, during both pre- and post-intervention/waiting periods. Analyses were conducted with linear mixed effects models, partial correlation analyses and t-tests.
Results:
There were group by time interaction effects with the scores of MAAS, NAS, PCL, IRI-Fantasy, and A-RSQ (p < .05). The mindfulness group had significant increase in MAAS (17.325%) and NAS (8.957%) scores, as well as reduction in PCL (15.599%) and A-RSQ (23.189%) scores (p < .05). Changes in non-attachment, but not mindfulness, had significant contributions to the score changes of PCL (16.375%), ASI (36.244%), IRI-Personal Distress (24.141%), IRI-Empathic Concern (16.830%), and A-RSQ (10.826%) (p < .05). The number of intervention sessions attended was correlated with score changes of NAS (r = .955, p < .001), and ASI (r = −.887, p < .001), suggesting a dose-dependent effect.
Conclusions:
Findings from this pilot study suggest that the mindfulness-based intervention improved mindfulness, non-attachment and empathy, which contributed to reduced interpersonal distress, rejection sensitivity and other psychological symptoms.
Keywords: childhood maltreatment, mindfulness, non-attachment, empathy, rejection sensitivity
Childhood maltreatment has long-lasting and pervasive impact on individuals’ psychological health (Teicher and Samson 2013), including social functioning (Simon et al. 2009). Childhood maltreatment often refers to adverse experience before the age of 18 due to emotional or physical abuse or neglect from caregivers, or witness of abuse upon their caregivers or siblings (Teicher and Parigger 2015). Post-traumatic stress and anxiety are common symptoms among childhood maltreatment survivors (Breslau et al. 2014). Post-traumatic stress is often expressed in symptoms such as intrusive memories or nightmares, emotional numbness, and avoidance of reminders of traumatic experiences (Kilpatrick et al. 2013); in particular, due to emotional numbness, individuals suffering from Post-Traumatic Stress Disorder (PTSD) often experience strains in interpersonal relationships (Ruscio et al. 2002) and perceive less social support (Beck et al. 2009). Heightened sensitivity to threatening stimuli (Fani et al. 2012), bias towards negative emotions (Krans et al. 2014), and negative interpretations of external stimuli (Bishop 2007) and internal experiences (Clark 1999) are also common symptoms of PTSD and anxiety disorders.
Furthermore, in the domain of interpersonal relationships, previous studies have shown that maltreated children had reduced prosocial behaviors and more withdrawn or disruptive or aggressive behaviors (Alink et al. 2012; Prino and Peyrot 1994). Such adverse impact still influences maltreated individuals when they enter adulthood; adults with a history of childhood maltreatment tend to have lower self-esteem and poorer social functioning (Liem and Boudewyn 1999), accompanied by maladaptive interpersonal schemas such as shame and vulnerability to harm that put them at higher risk for various psychological symptoms (Wright et al. 2009).
With regard to interpersonal relationships, empathy is an essential psychological construct (Davis 1980). Empathy often refers to the ability to understand and feel other people’s experiences (Bellet and Maloney 1991). Previous studies found individuals with childhood maltreatment histories showed impaired empathic processing, e.g., lowered empathic concern for others’ suffering (Locher et al. 2014), suppressed mirroring of others’ emotions (Ardizzi et al. 2016), reduced empathic accuracy in intimate relationships that contributed to marital dissatisfaction (Maneta et al. 2015), as well as lower sensitivity during mother-child interactions (Mielke et al. 2016). Existing literature suggests that empathy impairments among maltreated individuals could be due to empathy impairments in their abusive caregivers, which leads to lack of proper role models and learning opportunities (Francis and Wolfe 2008). Repeated findings of impaired empathic processing in this population and its pervasive impact on individuals’ social functioning call for effective interventions.
A rapidly growing body of research suggests that mindfulness-based interventions might help with the complex array of psychiatric difficulties often observed in individuals with a childhood maltreatment history (Kimbrough et al. 2010). Mindfulness involves awareness of moment-to-moment experiences without judgment or attachment (Kabat-Zinn 1990). It was believed that the “present focus” nature of mindfulness based interventions are particularly helpful for symptoms of avoidance and negative cognitions such as self-blame, shame and guilt among PTSD patients (Boyd et al. 2018), all of which are also common issues among childhood maltreatment victims (Hoglund and Nicholas 1995; Stuewig and McCloskey 2005).
Furthermore, cultivating mindfulness may even help promote empathy and prosocial behaviors. It was suggested that the nonjudgmental and present moment awareness of mindfulness practices can improve empathy by increasing the capacity of perspective taking and empathic concern, and by improving the skills for emotion identification and communication (Barnes et al. 2007). Mindfulness interventions have shown effects for improving social skills and prosocial behaviors among children and adolescents (Beauchemin et al. 2008; Flook et al. 2015). In adult samples, one study showed that various aspects of trait mindfulness were associated with feelings and performance in interpersonal situations (Dekeyser et al. 2008), e.g., “mindful observation” was associated with empathy, “acting with awareness and non-judgmental acceptance” was associated with less social anxiety and distress contagion (Dekeyser et al. 2008). Studies on mindfulness in romantic/marital relationships showed higher trait mindfulness predicted higher relationship satisfaction and better response to relationship stress (Barnes et al. 2007; Wachs and Cordova 2007).
Nevertheless, increasing empathy for individuals with a history of trauma, particularly those with active PTSD and/or anxiety symptoms, can be a double-edged sword. On one hand, increased empathy can alleviate the emotional numbness (van Der Kolk and Saporta 1991) and interpersonal aloofness (DeWall and Baumeister 2006) often experienced by trauma victims in response to the overwhelming emotional distress associated with the traumatic experience and their anxiety symptoms (Paivio and Laurent 2001). On the other hand, over-sensitivity to other people’s thoughts and feelings can lead to increased anxiety which results in more interpersonal difficulties (Wilhelm et al. 2004; Butler et al. 2007; Vidyanidhi and Sudhir 2009), either as a result of reactivity to others’ negative emotional experience in terms of vicarious anxiety (Kendall et al. 1978), or as a result of negative interpretations about the situation or others’ intentions which is a common cognitive bias among individuals with PTSD or anxiety disorders (Ashley et al. 2013; Mogg et al. 2000). Therefore, it’s necessary to investigate the particular psychological elements cultivated through the mindfulness intervention and their specific roles in eliciting changes in empathy and social functioning.
A keen probe into changes in prosociality is changes in how individuals perceive common social threats such as interpersonal rejection (Berenson et al. 2009), termed “rejection sensitivity”. Excessive concern about possible rejection is often accompanied by maladaptive relational patterns such as hostility, withdrawal or over-accommodation (Berenson et al. 2009; Romero-Canyas et al. 2010), which are common relationship issues among individuals suffering from PTSD (McFarlane and Bookless 2001). Rejection sensitivity perpetuates maladaptive interpersonal problems by prioritizing detection and reactivity to threats of rejection and readily activation of defense mechanisms (Berenson et al. 2009). A previous study showed that dispositional mindfulness, particularly the component of non-judgment, was negatively associated with rejection sensitivity (Peters et al. 2016).
Non-attachment, a construct related to mindfulness, may be able to serve as an antidote to the above-mentioned possible negative impact associated with interpersonal oversensitivity. Non-attachment, a concept that arose from Buddhism philosophy, reflects “a flexible way of relating to one’s experiences without clinging to or suppressing them” (Sahdra et al. 2015, page 263). Buddhist experts suggest that non-attachment can be expressed as “psychological flexibility (lack of fixation), nonreactivity (even-mindedness), more quickly recovering from upsets, allowing, releasing, supporting others’ capacity to choose, and a sense of ease” (Sahdra et al. 2010, page 118). Studies have shown that nonattachment was positively related to yet distinguishable from mindfulness (Sahdra et al. 2016; Sahdra et al. 2017). In a previous study, nonattachment independently predicted prosocial behaviors of helpfulness and kindness in an adolescent sample (Sahdra et al. 2015). It’s important to investigate whether non-attachment can be cultivated through mindfulness practices, as well as the effects of non-attachment on other prosocial traits such as rejection sensitivity.
In this study, we aimed to investigate whether a mindfulness-based intervention can help improve the above-mentioned prosocial elements, i.e., empathy, non-attachment and rejection sensitivity, and reduce psychological symptoms such as PTSD and anxiety. We hypothesized that after the mindfulness-based intervention, young adults with a history of childhood maltreatment would show improvement in empathic processing and rejection sensitivity, and non-attachment should play an important role in the prosocial changes. The primary outcome measures were changes in empathy, non-attachment and rejection sensitivity, the secondary outcome measures were changes in PTSD and anxiety symptom severity. With regard to the relationships among the psychological variables, we hypothesized that changes in mindfulness and non-attachment contribute to changes in empathy, which contributes to reduction in rejection sensitivity and psychological symptoms.
Methods
Participants
The present study was approved by the Institutional Review Board (IRB) of Partners HealthCare (IRB#: 2014P000295), which is the IRB for Massachusetts General Hospital, McLean Hospital, and several other local hospitals. Participants were recruited from the database of a previous study (Khan et al. 2015), among those who consented to be contacted for future studies. The previous study had comprehensive assessments of participants’ history of childhood maltreatment and psychological health. When participants were recruited for the present study, they were re-assessed with the Longitudinal Interview Follow-up Evaluation - Psychiatric Status Ratings (LIFE) (Keller et al. 1987) on their recent mental health conditions. Participants were enrolled into the study if they had at least one category of adverse childhood experience or childhood maltreatment as measured by the Adverse Childhood Experience (ACE) questionnaire (Felitti et al. 1998) or the Maltreatment and Abuse Chronology of Exposure (MACE) questionnaire (Teicher and Parigger 2015), had no history of psychotic or neurological disorders, between 19–35 years old, had no suicidal attempts during the past six months, eligible for MRI, and had no prior experience with systematic meditation programs. Participants were required to refrain from using illicit drugs throughout the course of the study.
A total of 43 participants were recruited, 21 of whom were enrolled into the mindfulness intervention while 22 were placed on the waiting list. Among participants in the mindfulness intervention, three participants dropped out, and another three participants did not yield any research data due to logistic issues with the study. Among participants on the waiting list, one participant dropped out, and two participants only completed the MRIs but not any questionnaire, one participant only completed questionnaires at post-waiting period but not at baseline thus was not included in the data analysis of the control group; therefore the total number of subjects included in the analysis of the waiting list control group was 18.
After the waiting period, six participants in the waiting list entered the mindfulness-based intervention program and completed research procedures a third time after completing the intervention program, among them, one participant completed other research procedures but did not complete questionnaires after the mindfulness intervention, another four participants completed the third assessment but they were not included in the data analyses of the mindfulness group out of statistical concerns, one participant completed questionnaires only after the waiting period and after the mindfulness intervention, but not at the baseline timepoint prior to the waiting period, thus data from this subject was included in the analysis of the mindfulness group but not the control group, which increased the total number of participants included in the analysis of the mindfulness group to 16.
Procedure
Detailed research procedure of this study was reported in our recent publication (Joss et al., 2019). There were a total of three waves of enrollment for three corresponding cohorts of mindfulness-based internetion programs. Upon enrollment into the study, prior to the start of the intervention program, research participants completed a battery of research questionnaires online via the REDCap electronic data capture tools (Harris et al., 2009). Upon completion of the intervention program, the same questionnaires were administered. Participants on the waiting lists were administered the same questionnaires at the same time periods as the those in the corresponding cohort of mindfulness-based intervention. MRIs and an episodic memory test were also administered at the same time, which will be reported in other publications. Participants on the waiting list were enrolled into the mindfulness-based intervention of the following cohort, and were administered the same research procedures for the third time upon completion of the intervention. The third cohort of mindfulness based intervention program did not have a correpsonding waiting list and did not yield research data due to logistic reasons.
The mindfulness-based intervention program was modeled after the Mindfulness Based Stress Reduction (MBSR) program protocol (Kabat-Zinn 1990). We followed the manual from the Center for Mindfulness in Medicine, Health Care, and Society (CFM) at University of Massachusetts Medical School (Santorelli et al. 2017). The intervention program was structured with eight weekly group sessions plus one full day (six hours) session. Our intervention program covered topics such as mindfulness, attention and awareness, perception and perspectives, being present, identifying stressors, stress physiology, responding vs. reacting to stress, stress coping strategies, handling difficult emotions and communications, and applying mindfulness in everyday life. A range of mindful meditation skills were taught throughout the program, such as breath awareness meditation, body scan meditation, mindful yoga, open awareness meditation, loving-kindness meditation, walking meditation, mountain meditation, mindful eating as well as noticing mindful moments in daily lives.
The intervention courses were taught by a licensed social worker and a licensed trauma-sensitive yoga instructor. Participants were instructed to practice the skills at home in-between the weekly meetings and discuss their experience with the home practice at the beginning of each weekly meeting; participants were also instructed to fill out a daily log of the amount of time they spent practicing each skill. Audio recordings of various length of primary meditation skills such as breath awareness meditation and body scan meditation were provided for home practice.
It was suggested in the MBSR manual that a history of trauma or abuse could “heighten emotional reactions” during the MBSR program (Santorelli et al. 2017, page 10). A previous study showed that individuals with a trauma history could have difficulty with long periods of practice, or struggle with some of the sitting meditation practices such as body scan and breath awareness meditation (Vallejo & Amaro, 2009); the study also showed that shorter practices and gentle movements were very helpful for individuals with a trauma history (Vallejo & Amaro, 2009). Another pilot study that applied the Mindfulness Based Cognitive Therapy program to combat veterans with PTSD showed that the “three-minute breathing space” exercise was particularly helpful (King et al. 2013). Therefore, in order to accommodate the needs of our study population, several modifications from the original MBSR manual were adapted to increase trauma sensitivity of the intervention program, such as providing instruction audios of various lengths to allow participants to have various options for their homework practices, inclusion of the “three-minute breathing space” exercise, encouragement of mindful movements, and general emphasis on empowering participants and giving them choices.
Measures
Participants’ childhood maltreatment history was assessed in the previous study (Khan et al. 2015) with ACE (Felitti et al. 1998), MACE (Teicher and Parigger 2015) and Childhood Trauma Questionnaire (CTQ) (Bernstein and Fink 1998). Participants completed the following psychological questionnaires online via the REDCap electronic data capture tools (Harris et al. 2009) before and after the intervention program, or the corresponding time points for participants in the waiting list group:
Mindful Attention Awareness Scale (MAAS) (Brown and Ryan 2003): a 15-item questionnaire assessing the frequency of mindful states with a focus on the presence or absence of attention to, and awareness of, what is occurring in the present. Example items include: “I could be experiencing some emotion and not be conscious of it until some-time later.”, “I break or spill things because of carelessness, not paying attention, or thinking of something else.”, “I rush through activities without being really attentive to them” and “I find myself listening to someone with one ear, doing something else at the same time.” Participants were instructed to respond with a six-point Likert scale to indicate how frequently they experienced each of the statements. This scale was reported to have an internal consistency of .82 – .87, and test-retest reliability of .81 (Brown and Ryan 2003).
Anxiety Sensitivity Index (ASI) (Peterson and Heilbronner 1987): a 16-item questionnaire on the fear of anxiety-related sensations based on beliefs about their harmful consequences. Example items include: “It is important for me not to appear nervous.”, “Other people notice when I feel shaky.”, and “It scares me when I am unable to keep my mind on a task”. Participants were instructed to respond with a five-point Likert scale to indicate how much each item applies to them. This scale was reported to have an internal consistency of .90 – .94, and test-retest reliability of .76 – .81 (Armstrong et al. 2006).
Posttraumatic Stress Disorder Checklist (PCL) (Blanchard et al., 1996): a self-report rating scale for DSM-IV-TR PTSD symptoms, including re-experiencing of trauma through intrusive recollections, flashback and nightmares, emotional numbness and avoidance of reminders of trauma, and hyperarousal such as sleep disturbances and irritability. The civilian version (as opposed to the military version) was used in the present study. Participants are prompted to indicate on a five-point Likert scale how much they had been bothered by each of the 17 “problems and complaints” in the scale, such as “Repeated, disturbing dreams of a stressful experience from the past”, “Avoid thinking about or talking about a stressful experience from the past to avoid having feelings related to it”, “Feeling distant or cut off from other people”, and “Feeling emotionally numb or being unable to have loving feelings for those close to you”. PCL was reported to have an internal consistency of .96 (Blanchard et al., 1996).
Adult Rejection Sensitivity Questionnaire(A-RSQ) (Berenson et al. 2009): a nine-item questionnaire about the extent of expected rejection in hypothetical scenarios that are common in the everyday life of an adult. For example: “Scenario #2: You approach a close friend to talk after doing or saying something that seriously upset him/her. (a) How concerned or anxious would you be over whether or not your friend would want to talk with you? (to respond on a six-point Likert scale from “very unconcerned” to “very concerned”) (b) I would expect that he/she would want to talk with me to try to work things out. (to respond on a six-point Likert scale from “very unlikely” to “very likely”)”. Previous research showed this questionnaire had internal consistency of .89 (Berenson et al. 2011) to .91 (Berenson et al. 2016).
Nonattachment Scale (NAS) (Sahdra et al. 2010): a 30-item scale informed by Buddhism philosophy to measure several aspects of “nonattachment”, including psychological flexibility, nonreactivity, mindedness, capability of recovery from emotional disturbances, and a sense of ease. Example items include “I can remain open to what life offers me regardless of whether it seems desirable or undesirable at a particular time.”, “I can admit my shortcomings without shame or embarrassment.”, and “I experience and acknowledge grief following significant losses, but do not become overwhelmed, devastated, or incapable of meeting life’s other demands.” Items are responded with a six-point Likert scale ranging from “disagree strongly” to “agree strongly”. This scale was reported to have an internal consistency of .94 and test-retest reliability of .87 (Sahdra et al. 2010).
Interpersonal Reactivity Index (IRI) (Davis 1983): a measure of dispositional empathy with four seven-item subscales (totally 28 items): Perspective Taking (PT), which is the tendency to spontaneously adopt the psychological point of view of others; Fantasy (FS), which taps respondents’ tendencies to transpose themselves imaginatively into the feelings and actions of fictitious characters in books, movies, and plays; Empathic Concern (EC), which assesses “other-oriented” feelings of sympathy and concern for unfortunate others; Personal Distress (PD), which measures “self-oriented” feelings of personal anxiety and unease in tense interpersonal settings. Below are some example items for each of the subscales: “(PT) I try to look at everybody’s side of a disagreement before I make a decision.”, “(FS) When I am reading an interesting story or novel, I imagine how I would feel if the events in the story were happening to me.”, “(EC) I am often quite touched by things that I see happen.”, and “(PD) I sometimes feel helpless when I am in the middle of a very emotional situation.” Items are responded with a five-point Likert scale ranging from “does not describe me well” to “describes me very well”. The subscales’ internal reliabilities range from .71 to .77, and test-retest reliabilities range from .62 to .71 (Birnie et al. 2010).
Data analyses
We used statistical software R to perform several linear mixed effects model analyses. We first used linear mixed effects models to test for group by time interaction effects for each of the questionnaire scores, with age, sex, race and time interval between the two measurements as covariates. Then with additional linear mixed effects models, we calculated the amount of variance in score changes of PCL, ASI, A-RSQ, and the four IRI subscales explained by score change of NAS or MAAS respectively, with group, age, sex, race and time interval between the two measurements as covariates. Similarly, we also calculated the amount of variance in score change of A-RSQ explained by score change of each of the IRI subscales. Effect sizes were evaluated with likelihood ratio and corresponding p-values.
After the linear mixed effects models analyses, we used SPSS to perform the following t-tests: (1) we first used independent two-sample t-tests to compare baseline questionnaire scores of the two groups; (2) then we used paired samples t-test on the data from each group to test whether there were significant score changes after the intervention or waiting period; (3) then we calculated the percent change amounts between the two timepoints (post- minus pre- intervention/waiting scores), and used independent two-sample t-test to assess group differences in questionnaire score changes. Effect size of t-tests were evaluated with Cohen’s d.
We used SPSS to perform the following correlation analyses: (1) partial correlation analyses, with group, age, sex, race and time-interval between measurements as covariates, were used to investigate the relationships among baseline questionnaire scores; (2) partial correlation analyses, with age, sex, race and time-interval between measurements as covariates, were used to investigate the relationships among questionnaire score changes within the mindfulness group only.
There were missing data with 3 participants in the mindfulness group and 5 participants in the control group (for details see Table S1 in Supplementary Material). Missing data were handled with the following methods in the two corresponding scenarios: (1) For participants with single items missing in questionnaires, imputation was performed with SPSS; the imputed value for the missing item was calculated as the mean of the output from 50 permutations. (2) For participants that had missing data with a whole scale, “pair-wise deletion” method was used, i.e., participants with missing data on a particular questionnaire were excluded from analyses involving that particular questionnaire, but the questionnaires in which the participant did not have missing data were analyzed with the participant’s data included.
Results
Participants’ demographic information, childhood maltreatment assessment scores and lifetime DSM diagnoses are displayed in Table 1. The two groups did not differ significantly in the distribution of sex (χ2= 0.926, p = .336) and race (χ2= 3.421, p = .490), however, there was a marginally significant difference with age (t =−1.950, p = .060), in that the mindfulness group was slightly older than the control group. All demographic variables were used as covariates in subsequent analyses. There was no significant group difference on any of the childhood maltreatment measures, or frequency of lifetime DSM-IV-TR disorder diagnosis. In terms of DSM diagnoses, 35.3% participants met diagnosis criteria for lifetime depressive disorders, 41.2% participants met diagnosis criteria for lifetime anxiety disorders, 11.8% met diagnosis criteria for lifetime personality disorders (see Table 1); in particular, 2.9% participants met diagnosis criteria for PTSD, which was classified under anxiety disorder in DSM-IV-TR. Participants in the mindfulness group on average attended 7.563 (SE = 0.376, range 5–9) out of the total of 9 intervention sessions, and on average practiced at home for 758.688 minutes (SE = 132.060, range 40–1804).
Table 1.
Demographic, childhood maltreatment assessment and DSM diagnosis information of research participants.
| Mindfulness | Waitlist | Group Difference | |
|---|---|---|---|
| Sample Size (N) | N=16 | N=18 | |
| Sex: Female(F); Male(M) | F:13, M:3 | F:12, M:6 | χ2= 0.926, p = .336 |
| Average Age (in years) (SE, range) | 26.44 (SE=0.474, 22–29) | 24.94 (SE=0.586, 22–29) | t= −1.950, p = .060 |
| Race (Frequencies) | |||
| White | 9 | 13 | χ2= 3.421, p = .490 |
| Black/African American | 4 | 1 | |
| Asian | 2 | 2 | |
| Hispanic | 1 | 1 | |
| Unknown | 0 | 1 | |
| Childhood Maltreatment Assessments (Mean (SE), range) | One-Way ANOVA | ||
| ACE Scores | 2.000(0.465), 0–5 | 1.647(0.507), 0–7 | F = 0.261, p = .613 |
| CTQ-Emotional Abuse | 9.188(1.133), 5–21 | 9.941(1.123), 5–21 | F = 0.189, p = .667 |
| CTQ-Physical Abuse | 6.688(0.454), 5–10 | 6.000(0.429), 5–11 | F = 1.215, p = .279 |
| CTQ-Sexual Abuse | 6.438(1.245), 5–25 | 5.529 (0.471), 5–13 | F = 0.488, p = .490 |
| CTQ-Emotional Neglect | 9.938(1.131), 5–18 | 11.059(1.384), 5–22 | F = 0.388, p = .538 |
| CTQ-Physical Neglect | 6.438(0.532), 5–10 | 6.706(0.580), 5–13 | F = 0.115, p = .736 |
| MACE-number of types of maltreatment | 1.625 (0.523), 0–6 | 2.059 (0.591), 0–7 | F = 0.299, p = .588 |
| MACE-total severity scores | 18.000 (3.833), 0–40 | 21.412 (3.448), 5–51 | F = 0.440, p = .512 |
| MACE-sexual abuse | 0.625 (0.301), 0–4 | 0.647 (0.363), 0–5 | F = 0.002, p = .963 |
| MACE-parental verbal abuse | 3.563 (1.016), 0–10 | 3.941 (0.872), 0–10 | F = 0.081, p = .778 |
| MACE-non-verbal emotional abuse | 2.625 (0.591), 0–8 | 2.941 (0.639), 0–8 | F = 0.131, p = .720 |
| MACE-parental physical maltreatment | 3.125 (0.625), 0–6 | 2.588 (0.556), 0–8 | F = 0.414, p = .525 |
| MACE-witnessing violence between parents | 0.875 (0.547), 0–8 | 1.176(0.487), 0–6 | F = 0.170, p = .683 |
| MACE-witnessing siblings abused by parents | 0.688 (0.384), 0–5 | 0.882 (0.342), 0–3 | F = 0.144, p = .707 |
| MACE-peer verbal abuse | 3.750 (0.911), 0–10 | 5.647 (0.878), 0–10 | F = 2.249, p = .144 |
| MACE-peer physical abuse | 0.875 (0.437), 0–5 | 1.235(0.450),0–6 | F = 0.329, p = .570 |
| MACE-emotional neglect | 1.500 (0.438), 0–4 | 1.882(0.499), 0–6 | F = 0.334, p = .567 |
| MACE-physical neglect | 0.375 (0.272), 0–4 | 0.471(0.212), 0–2 | F = 0.078, p = .782 |
| DSM-IV-TR diagnosis (Frequencies) | Fisher’s exact test | ||
| Depressive Disorders | 7 | 5 | p = .475 |
| Anxiety Disorders | 7 | 7 | p = .524 |
| Personality Disorders | 1 | 3 | p = .348 |
Intervention related score changes
Results from linear mixed effects model analyses, with covariates including age, sex, race and time-interval between measurements, are displayed in Table 2. There were significant group by time interaction effects with scores of MAAS (F(1,29) = 7.252, p < 0.05, effect size: likelihood ratio = 9.690, p < .05), NAS (F(1, 29) = 6.889, p < .05, effect size: likelihood ratio = 10.294, p < .05), PCL (F(1,31) = 5.310, p < .05, effect size: likelihood ratio = 11.766, p < .01), IRI-Fantasy (F(1,31) = 9.084, p < .01, effect size: likelihood ratio = 9.876, p < .05) as well as A-RSQ (F(1,30) = 9.274, p < .01, effect size: likelihood ratio = 8.591, p < .05); the effect was marginally significant for IRI-PD scores (F(1,31)=3.615, p = .067; effect size: likelihood ratio = 6.814, p = .078).
Table 2.
Scores and statistics of self-report questionnaires.
| Mindfulness Mean (SE) | Waiting List Control Mean (SE) | Linear Mixed Effects Model | ||||
|---|---|---|---|---|---|---|
| group X time interaction(F-value) | Effect Size: Likelihood Ratio | |||||
| Pre | Post | Pre | Post | |||
| Mindful Attention Awareness Scale (MAAS) | 3.442 (0.159) | 4.009** (0.198) | 3.521 (0.189) | 3.563 (0.190) | 7.252* | 9.690* |
| Non-Attachment Scale (NAS) | 123.933 (5.951) | 133.533* (5.317) | 118.625 (4.11) | 114.688 (4.18) | 6.889* | 10.294* |
| Anxiety Sensitivity Index (ASI) | 15.533 (2.342) | 14.787 (2.407) | 14.938 (1.883) | 17.996 (2.056) | 1.040 | 6.630 |
| PTSD Checklist (PCL) | 30.063 (2.709) | 24.000** (1.381) | 29.412 (2.35) | 29.824 (3.07) | 5.310* | 11.766** |
| Interpersonal Reactivity Index (IRI): Fantasy | 16.813 (1.600) | 18.438 (1.057) | 19.353 (1.225) | 16.688 (1.492)* | 9.084** | 9.876* |
| IRI: Personal Distress | 10.375 (1.480) | 8.375* (1.524) | 10.647 (1.303) | 10.974 (1.063) | 3.615 | 6.814 |
| IRI: Empathic concern | 19.750 (0.998) | 20.625 (1.110) | 18.706 (1.29) | 18.824 (0.70) | 0.340 | 0.641 |
| IRI: Perspective Taking | 18.320 (1.192) | 18.313 (1.106) | 16.824 (0.86) | 17.000 (0.93) | 0.035 | 0.071 |
| Adult Rejection Sensitivity Questionnaire | 8.937 (1.204) | 6.750* (1.147) | 8.416 (0.823) | 9.580 (0.949) | 9.274** | 8.591* |
SE: standard error. Significance levels are indicated as:
p<0.01,
p<0.05.
None of the questionnaire scores had significant group difference at baseline (p-values range from .16 to .99 from independent two-samples t-tests). Within the mindfulness group, there were significant post-intervention score changes (compared to baseline) on the following scales: significant increase of NAS scores (t(14)=2.466, p < .05, Cohen’s d = 0.681) and MAAS scores (t(14)= 3.877, p < .01, Cohen’s d = 1.002), as well as significant decrease of PCL scores (t(15) = −3.227, p < .01, Cohen’s d = 0.807), IRI-PD scores (t(15) = −2.138, p < .05, Cohen’s d = 0.535) and A-RSQ scores (t(15)= −2.534, p < .05, Cohen’s d = 0.634), while the scores of IRI-PT, IRI-FS, IRI-EC and ASI did not have significant change (p values ranged from .161 to .992). Within the control group, there was a significant decrease on scores of IRI-FS (t(16) =−2.873, p < .05, Cohen’s d = 0.697), and a marginally significant increase on scores of A-RSQ (t(15)=1.904, p = .076, Cohen’s d = 0.476) and ASI (t(15) = 2.040, p = .059, Cohen’s d = 0.510). Changes in MAAS was reported in detail in our previous study (Joss et al., 2019), and is included in this paper for completeness of narrative; the numbers are slightly different because in this paper, data from the 4 participants that completed the mindfulness intervention after their waiting period were only included in the analyses of the control group but not the mindfulness group.
For illustration purpose, the percent change (post- minus pre-intervention or waiting period, then divided by baseline scores) of scores on NAS, MAAS, PCL and A-RSQ were calculated for each participant, with the means of each group and corresponding standard errors plotted in Figure 2. The mindfulness group had significant (p < .05) increase in MAAS (17.325%) and NAS (8.957%) scores, as well as reduction in PCL (15.599%) and A-RSQ (23.189%) scores. Significant group difference was found with the percent change in scores of MAAS (t(29) = −2.568, p < .05, Cohen’s d = 0.923), NAS (t(29)= −3.055, p < .01, Cohen’s d = 1.101), PCL (t(31)=2.319, p < .05, Cohen’s d = 0.806) and A-RSQ (t(30)=3.270, p < .01, Cohen’s d =1.156).
Figure 2:
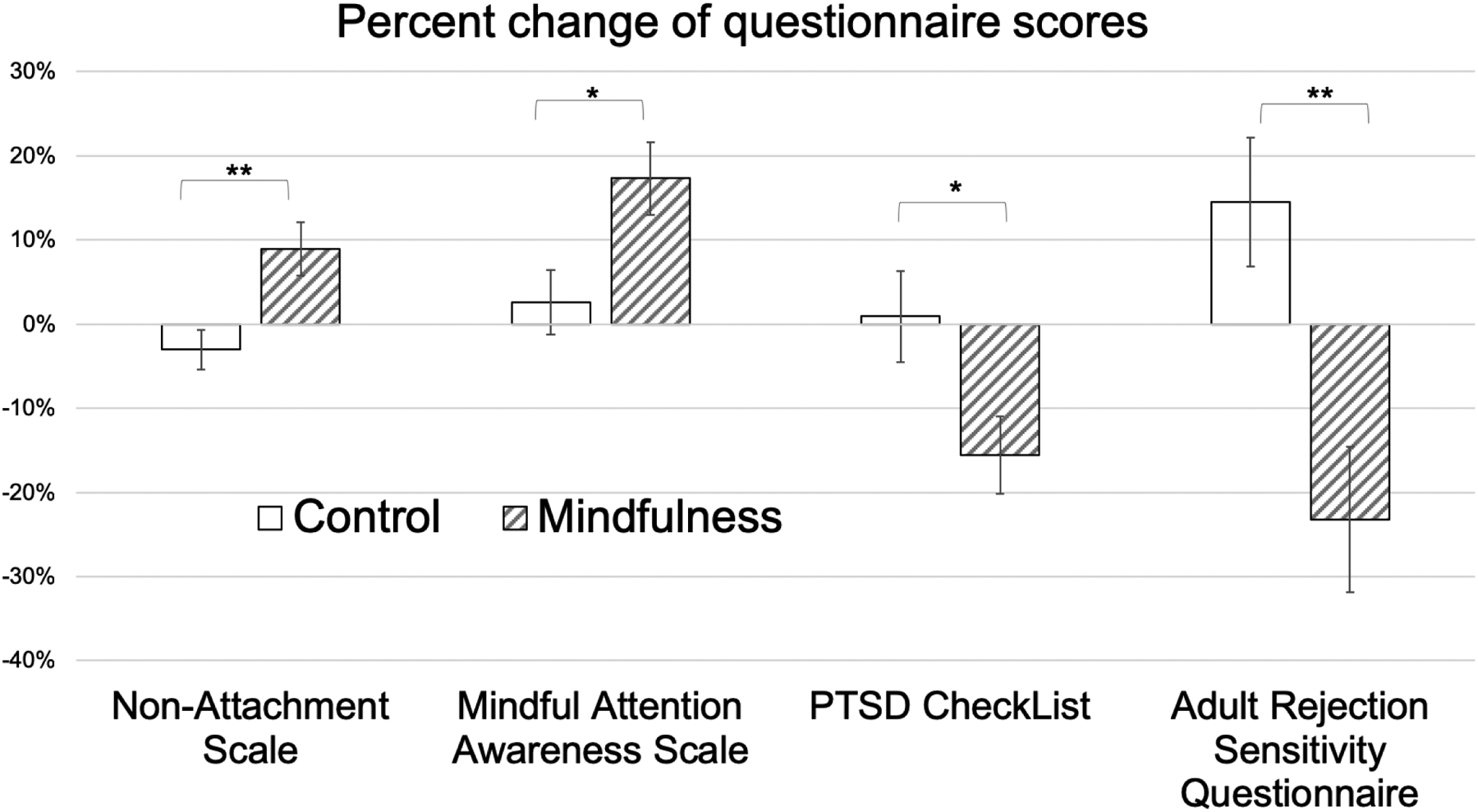
Illustration of questionnaire score percent change (post-intervention or post-waiting period). Asterisks (*) indicate the significance level of group differences: **: p<0.01, *: p<0.05.
Correlation between questionnaire scores at baseline
At baseline prior to the intervention or waiting period, among all participants in both groups (Table 3.A), there was significant negative correlations between NAS scores and the scores of PCL (r = −.489, p < .01), ASI (r = −.449, p < .05), IRI-FS (r = −.412, p < .05) and IRI-PD (r = −.616, p < .001) (Table 3.A). There were also positive correlations between baseline PCL scores and those of A-RSQ (r = .396, p < .05), ASI (r = .507, p < .01), and IRI-PD (r = .522, p < .01) (Table 3.A). There was a negative correlation between baseline IRI-PT scores and those of IRI-PD (r = −.430, p < .05).
Table 3.
Cross correlation among questionnaire scores. Correlation coefficients are from partial correlation analyses with (A)baseline questionnaire scores among all participants in both groups, controlled for group age, sex and race, or (B) score changes within the mindfulness group only, controlled for age, sex and race.
| (A) Correlations Among Baseline Questionnaire Scores | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| MAAS | A-RSQ | PCL | ASI | IRI-PT | IRI-FS | IRI-EC | IRI-PD | ||
| Non-Attachment Scale (NAS) | .130 | −.264 | −.489** | −.449* | .280 | −.412* | −.221 | −.616*** | |
| Mindful Attention Awareness Scale (MAAS) | 1 | −.304 | −.273 | .070 | .475* | −.272 | .156 | −.148 | |
| Adult Rejection Sensitivity Questionnaire (A-RSQ) | 1 | .396* | .093 | −.060 | .362 | −.195 | .227 | ||
| PTSD CheckList (PCL) | 1 | .507** | −.214 | .270 | −.282 | .522** | |||
| Anxiety Sensitivity Index (ASI) | 1 | −.174 | .107 | .274 | .385* | ||||
| IRI-Perspective Taking (PT) | 1 | −.214 | .170 | −.430* | |||||
| IRI- Fantasy (FS) | 1 | .047 | .288 | ||||||
| IRI-Empathic Concern (EC) | 1 | −.043 | |||||||
| IRI-Personal Distress (PD) | 1 | ||||||||
| (B) Correlations Among Score Changes in Mindfulness Group (Post- minus Pre-Intervention Scores) | |||||||||
| NAS | MAAS | A-RSQ | PCL | ASI | IRI-PT | IRI-FS | IRI-EC | IRI-PD | |
| Non-Attachment Scale (NAS) | 1 | .174 | .242 | −.086 | −.510 | .283 | −.388 | .441 | −.199 |
| Mindful Attention Awareness Scale (MAAS) | 1 | .258 | .008 | −.167 | −.183 | .552 | .050 | .053 | |
| Adult Rejection Sensitivity Questionnaire (A-RSQ) | 1 | .675* | .256 | .516 | .424 | .386 | −.286 | ||
| PTSD CheckList (PCL) | 1 | .357 | .869*** | .525 | .860*** | .048 | |||
| Anxiety Sensitivity Index (ASI) | 1 | .112 | .464 | −.054 | .689* | ||||
| IRI-Perspective Taking (PT) | 1 | .337 | .818** | −.007 | |||||
| IRI- Fantasy (FS) | 1 | .284 | .236 | ||||||
| IRI-Empathic Concern (EC) | 1 | .184 | |||||||
| Number of Sessions Attended | .955*** | .245 | .330 | .131 | −.887*** | .096 | −.364 | .246 | −.644* |
| Total Home Practice Minutes | .363 | −.013 | .345 | .170 | −.607* | .134 | −.258 | .110 | −.565 |
Significance levels are indicated as
p<0.001,
p < 0.01,
p < 0.05.
Correlation between score changes
In the mindfulness group (Table 3.B), the amounts of post-intervention score changes (compared to pre-intervention scores) of PCL showed significant positive correlations with score changes of A-RSQ (r = .675, p < .05), IRI-PT (r = .869, p < .001), IRI-EC (r = .860, p < .001) with a marginally significant correlation with IRI-FS (r = .525, p = .080). In addition, the ASI score change was positively correlated with score change of IRI-PD (r = .689, p < .05); the IRI-PT score change was positively correlated with score change of IRI-EC (r = .818, p < .01).
Dose-dependent effects of the intervention
There were significant dose dependent effects of number of sessions attended on score changes of NAS, IRI-PD, and ASI, with more attendance associated with a greater score increase of NAS (r = .955, p < .001, Table 3.B) and a greater score reduction of IRI-PD (r = .644, p < .05) and ASI (r = .887, p < .001), after controlling for age, sex, race and time-interval. Participants who practiced more at home also had a greater score reduction of ASI (r = .607, p < .05) and IRI-PD (r = .565, p = .055) (Table 3.B).
Contribution of NAS and MAAS for questionnaire score changes
Additional linear mixed effects models analyses showed that score changes of NAS explained significant amounts of variance in score changes of PCL (16.375%, effect size: likelihood ratio = 20.701, p < .001), ASI (36.244%, effect size: likelihood ratio = 41.104, p < .0001), A-RSQ (10.826%, Likelihood ratio = 10.397, p < .05), IRI-EC (16.830%, effect size: likelihood ratio = 22.646, p = .0001), and IRI-PD (24.141%, effect size: likelihood ratio = 21.433, p < .001) (Figure 3.A). In contrast, similar analyses with MAAS scores showed that changes in mindfulness levels only explained a significant amount of variance for the score changes of ASI (10.503%, effect size: likelihood ratio =10.434, p < .05) and IRI-FS (6.817%, effect size: likelihood ratio =13.117, p < .05), but not any other scales (Figure 3.A).
Figure 3:
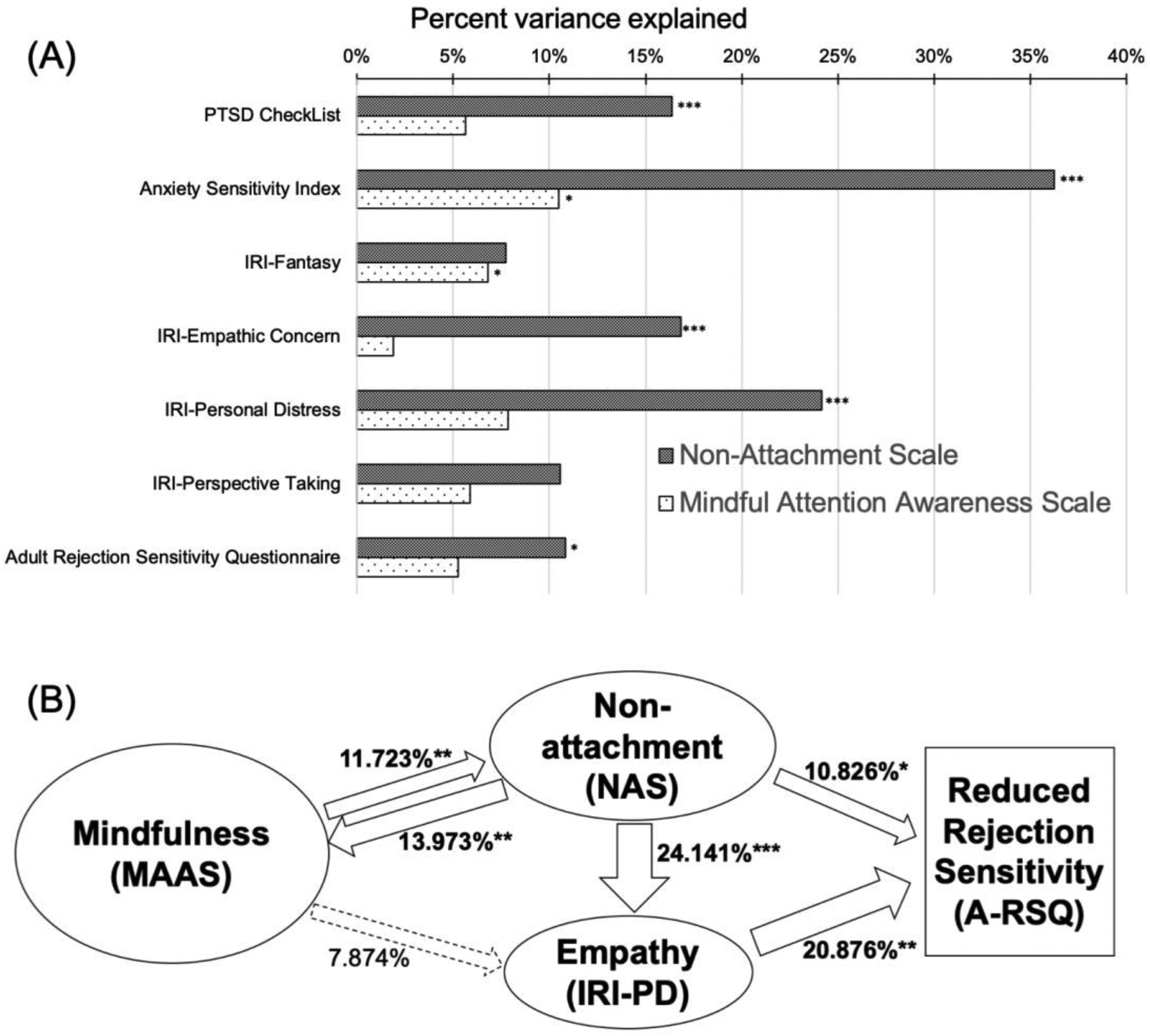
(A) Amount of variance in score change of each questionnaire explained by score change of NAS and MAAS. (B) Diagram of relationships among major psychological variables in the present study, with numbers on arrows representing amount variance explained, e.g., changes in MAAS scores explained 11.72% variance in changes in NAS scores. Asterisks (*) indicate the significance level of the effect size of each model: ***: p < 0.001, **: p<0.01, *: p<0.05.
With regard to the relationships among the questionnaires, we hypothesized that changes in mindfulness and non-attachment contributed to changes in empathy, which contributed to reduction in rejection sensitivity and psychological symptoms. Corresponding analyses showed that (see Figure 3.B): (1) Changes of MAAS scores explained a significant amount variance in the score changes of NAS (11.723%, effect size: Likelihood ratio = 15.214, p < .01); at the same time, changes of NAS scores also explained a significant amount of variance in the score changes of MAAS (13.973%, effect size: Likelihood ratio = 16.325, p < .01) (2) MAAS score changes did not explain a significant amount variance in the score changes of IRI-PD (7.874%, effect size: Likelihood ratio = 7.633, p = .106), but NAS score changes did (24.141%, effect size: Likelihood ratio = 21.433, p < .001). (3) IRI-PD score changes explained a significant amount variance in A-RSQ score changes (20.876%, effect size: Likelihood ratio =17.212, p < .01); other IRI subscales did not explain a significant amount of variance in A-RSQ score changes. (4) IRI-PD score changes explained a significant amount of variance in score changes of ASI (25.028%, effect size: likelihood ratio = 23.128, p = .0001) and PCL (19.893%, effect size: likelihood ratio = 16.337, p < .01); IRI-EC also explained a significant amount of variance in the score change of PCL (5.744%, effect size: likelihood ratio = 12.539, p < .05), with marginal significance for ASI (4.567%, effect size: likelihood ratio = 8.827, p = .066); IRI-PT explained a significant amount of variance in the score change of ASI (10.133%, effect size: likelihood ratio = 13.504, p < .01); besides the above mentioned, other IRI subscales did not explain a significant amount of variance in ASI or PCL score changes.
Discussion
This pilot study looked at the effects of a mindfulness-based intervention on mindfulness, non-attachment, empathy and rejection sensitivity, as well as the roles of these psychological constructs in alleviating psychological symptoms, among a sample of young adults with a childhood maltreatment history, compared to matched participants on the waiting list. Our results showed that participants in the mindfulness group had increased mindfulness and non-attachment, as well as reduced rejection sensitivity and PTSD symptoms. There was a dose-dependent relationship between the amount of intervention participation on changes of non-attachment and anxiety. Our results also suggest that non-attachment played an important role for changes in empathy, rejection sensitivity and psychopathology.
The study population: young adults with a history of childhood maltreatment
“Childhood maltreatment” is a complex concept and its definition has evolved with increasing amounts of research; traditionally, such as in the CTQ, physical and emotional abuse and neglect as well as sexual abuse have been the major categories of childhood maltreatment (Bernstein and Fink 1998); recent research development, such as the MACE, has included additional categories such as parental verbal abuse, non-verbal emotional abuse, peer verbal and physical abuse, witnessing violence between parents and witnessing siblings abused by parents (Teicher and Parigger 2015). Childhood maltreatment histories of research participants in the present study were assessed with both the CTQ and the MACE.
Depression, anxiety, and PTSD symptoms are common symptoms among adults with a childhood maltreatment history; one study showed that 37% of adults with a childhood abuse history had a lifetime diagnosis of major depressive disorder, 39.6% had an anxiety disorder and 19% had PTSD (Collishaw et al. 2007). The prevalence of depression (35.3%) and anxiety disorders (41.2%) in the sample of the present study are similar to the previous finding (Collishaw et al. 2007), the prevalence of PTSD is lower (2.9%), which could be due to our small sample of research participants who mostly had mild to moderate childhood maltreatment. Note that having PTSD symptoms is different from meeting the DSM-IV-TR diagnostic criteria of PTSD; the PCL scale in the present study provided a continuous score of PTSD symptom severity, whereas the DSM clinical interview provided a binary diagnosis result.
Our previous study investigated in the same sample of participants the effect of the mindfulness-based intervention on depression and anxiety symptoms (Joss et al. 2019), whereas the present study is focused on PTSD symptoms and anxiety sensitivity. Anxiety sensitivity is a nuanced aspect of anxiety that focuses on individuals’ fear of anxiety-related sensations and consequences, i.e., “fear of fear” (Reiss et al. 1986), which we hypothesized would benefit from the mindfulness based intervention due to its training on acceptance, present-focus and non-judgment.
The concept of non-attachment
The concept of non-attachment was derived from the Buddhism philosophy (Sahdra et al. 2010). It reflects “a flexible way of relating to one’s experiences without clinging to or suppressing them” (Sahdra et al. 2015, page 263). It is “related but distinguishable from the Western construct of attachment” (Sahdra et al. 2010, page 116). The Buddhist notion of non-attachment is “based on insight into the constructed and impermanent nature of mental representations” (Sahdra et al. 2010, page 116). The state of “nonattachment” indicates “release of mental fixations”, which in turn encourages “more objective perception, greater compassion, reduced selfishness, and release from, or letting go of, what Buddhists call “afflictive” emotions, thus alleviating suffering.” (Sahdra et al. 2010, page 125). Both the “non-attachment” and “mindfulness” concepts rise from the Buddhism philosophy; existing studies indicate that although non-attachment is positively related to mindfulness, it’s distinguishable from mindfulness (Sahdra et al. 2016; Sahdra et al. 2017).
Trait non-attachment and its relationship with other psychological traits
Trait non-attachment can be an indicator of psychological health. In previous studies, scores of NAS have been shown to be positively correlated with positive psychological traits such as mindfulness, acceptance, nonreactivity, self-compassion, autonomous motivation and noncontingent happiness, while negatively correlated with maladaptive psychological phenomenon such as anxious attachment, avoidant attachment, depersonalization, amnesia and materialism (Sahdra et al. 2010). Previous research also showed that NAS scores were positively correlated with measurements of life satisfaction, pleasant affect, purpose in life, perspective taking (measured by IRI-PT) and empathic concern (measured by IRI-EC) and negatively correlated with depression, anxiety, stress, difficulty in emotion regulation, and personal distress (measured by IRI-PD) (Sahdra et al. 2010).
The present study found that prior to the intervention or waiting period, baseline scores of NAS had significant negative correlations with the severity of PTSD and anxiety sensitivity, as well as the personal distress subscale of IRI, which is consistent with prior findings that trait non-attachment is negatively associated with psychopathology (Sahdra et al. 2010).
Increased non-attachment after the mindfulness-based intervention
With respect to the effect of the mindfulness-based intervention on non-attachment, the present study found a significant group by time interaction with the NAS scores, as well as a significant score increase after the mindfulness-based intervention, suggesting that the mindfulness-based intervention could help cultivate non-attachment traits. Although the positive correlation between non-attachment and mindfulness scores did not reach significance at baseline, the amounts of changes in non-attachment was positively correlated with the amounts of changes in mindfulness in the whole study sample of both groups (supplementary material, Table S2), which is consistent with prior reports on the positive associations between non-attachment and mindfulness (Sahdra et al. 2010; Sahdra et al. 2016; Sahdra et al. 2017).
Furthermore, results from the present study also showed that changes in NAS scores significantly contributed to changes in PTSD symptom severity, anxiety sensitivity, rejection sensitivity, as well as score changes of the empathic concern and personal distress aspects of empathy, suggesting that improvement of non-attachment traits positively influenced the overall psychological landscape. More importantly, similar analyses found mindfulness was not a significant contributor to symptom reduction, which is consistent with prior reports that nonattachment was distinguishable from mindfulness (Sahdra et al. 2016; Sahdra et al. 2017).
The concept of empathy and its relevance with psychopathology
Empathy is the capacity to understand others’ perspectives and to feel and share others’ feelings (Snyder et al. 2011). Broadly speaking there are two major aspects in empathy: the cognitive aspect and the affective/emotional aspect, with the former emphasizes perception of others’ mental state while the latter emphasizes the ability to respond emotionally to others’ emotions. “Perspective taking”, i.e., the ability to adopt others’ perspectives, and “fantasy”, i.e., the ability to identify with fictional characters, two of the subscales of the IRI scale used in the present study, reflect cognitive empathy (Rogers et al. 2007). The other two subscales of IRI, “empathic concern” and “personal distress”, reflect affective empathy (Rogers et al. 2007), in which empathic concern is about the sympathy and compassion for others while personal distress is the “self-oriented feelings of anxiety and discomfort” in response to others’ suffering (Rogers et al. 2007, page 711). Some prior studies suggest the “fantasy” subscale is less robust than other subscales since it measures mental processes that are not exclusive to empathy and it does not have concurrent validity with other empathy measures (Birnie et al. 2010).
Empathy is critical for interpersonal relationships, which are essential for healthy psychological functioning (Davis 1980). Impairment of empathy, particularly the affective aspect, has been found in various psychological disorders, such as social anxiety disorder (Morrison et al. 2016), depression (O’Connor et al. 2002), and PTSD (Mazza et al. 2015). Findings in the present study suggest that histories of different kinds of childhood maltreatment could have different impacts on perspective taking or empathic concern (see Supplementary Material Figures S1&S2), which expanded the existing knowledge on impaired empathy among individuals with childhood maltreatment histories (Benarous et al. 2015).
The present study found a significant negative correlation between the baseline scores of IRI-PD and IRI-PT, which is consistent with prior findings on negative correlations between the two subscales (Davis 1980; Gilet et al. 2013). The present study also found that the baseline scores of IRI-PD were positively correlated with the severity of PTSD and anxiety sensitivity, which is consistent with prior findings that IRI-PD scores were associated with severity of PTSD (Nietlisbach et al. 2010) and social anxiety (Contardi et al. 2013). These findings confirmed the existence of empathy impairment in our study population, as well as its association with psychopathology.
Effects of the mindfulness-based intervention on empathy
Several previous studies have investigated the impact of mindfulness on empathy (Beddoe and Murphy 2004; Block-Lerner et al. 2007; Birnie et al. 2010). It was suggested that the “nonjudgmental” and “present focused” nature of mindfulness practices could help increase the capacity for perspective taking and empathic concern (Block-Lerner et al. 2007). A previous study showed increased scores on the Perspective Taking subscale and decreased scores on the Personal Distress subscale of IRI after MBSR in an adult community sample (Birnie et al. 2010).
In the present study, among our sample of young adults with a history of childhood maltreatment, we observed significantly decreased personal distress scores of IRI after the mindfulness-based intervention and a significant group by time interaction with the fantasy subscale. Some studies suggest that the Fantasy (Birnie et al. 2010) and Personal Distress (Cliffordson 2001) facets of the IRI scale are tangential to empathy, while Perspective Taking and Empathic Concern are the major facets of cognitive (the former) and affective (the latter) empathy. In the present study, there was no significant group by time interaction effect with the scores of IRI-PT and IRI-EC, nor was there significant change after the mindfulness intervention. The finding that participants in the present study did not have significant improvement on IRI-PT or IRI-EC scores could be due to the fact that the mindfulness intervention used in the present study was not particularly focused on empathy. Some other mindfulness practice, such as the loving-kindness meditation, provides concentrated training on empathy and compassion (Kristeller and Johnson 2005). For example, a prior study found a significant relationship between loving-kindness meditation and perspective taking (Leppma and Young 2016). Although the intervention program in the present study also introduced the loving-kindness meditation practice, it was only briefly introduced towards the end of the program and was not emphasized as much as other practices such as the breath awareness and body scan meditation practices.
The present study also found positive associations between PCL score changes and score changes of IRI-PT and IRI-EC, i.e., participants with greater increase in Empathic Concern or Perspective Taking had less reduction in PTSD symptoms. It was suggested that constructs of empathy are intertwined with core PTSD symptoms such as emotional numbing and avoidance of social interactions (Nietlisbach and Maercker 2009). Findings in the present study suggest that increase in certain aspects of empathy, if looking at in isolation, could interfere with PTSD symptom reduction; increase in empathy shall be accompanied by other factors such as increased non-attachment and reduced rejection sensitivity to alleviate PTSD symptoms. This is consistent with existing thoughts in the literature that proposes “perceived social exclusion as a maintenance factor for PTSD” (Nietlisbach and Maercker 2009, page 382).
Rejection Sensitivity
Rejection sensitivity is an aspect of prosociality. Prior research suggests that child abuse is predictive of rejection sensitivity, which in turn mediates the impact of early life trauma on interpersonal relationships (Purdie and Downey 2000). Interpersonal traumatic experience, e.g., childhood maltreatment, often involves negligence of victim’s needs, violation of their boundaries, or other forms of deviations from social norms, which leads to victims’ threatened sense of belonging and perception of social isolation, which further leads to heightened sensitivity to cues of rejection in the aftermath of traumatic experiences (Nietlisbach and Maercker 2009). Social exclusion and social stigmatization are powerful factors for triggering and maintaining psychological symptoms related to traumatic life experiences (Nietlisbach and Maercker 2009). Therefore, it was suggested that social acknowledgment and “re-inclusion” are important factors of trauma processing and recovery (Mueller et al. 2008; Wagner et al. 2012).
The present study observed significantly reduced rejection sensitivity among young adults with a history of childhood maltreatment after the mindfulness-based intervention. Our data suggests that increase in non-attachment had significant contribution to the decrease in rejection sensitivity, which can be attributed to the psychological elements cultivated in the mindfulness-based intervention such as non-judgment, acceptance and self-compassion (Joss et al. 2019), all of which are closely related to the concept of non-attachment. The decreased rejection sensitivity could also be partially attributed to the group format of the intervention, which creates the opportunity for rebuilding participants’ sense of belonging and inclusion. Because the control condition in the present study is waiting list, the group difference on rejection sensitivity changes could be attributed to the difference in group social support; to clarify this factor, future study shall employ an active control group that also has a group format.
Limitations and Future Research
This pilot study provided preliminary insights on the effects of a mindfulness-based intervention for cultivating traits of non-attachment and empathy within a population of young adults with childhood maltreatment histories. Findings from this pilot study pointed out the important roles of non-attachment and empathy in the therapeutic effects of the mindfulness-based intervention in reducing rejection sensitivity and psychological symptoms.
This study has several major limitations, including having a relatively small sample, only having a waiting list control as opposed to an active control condition, lack of randomization, and lack of long term follow up. Such limitations affect the generalizability of the findings and shall be addressed in future studies. There are also limitations with the use of self-reported measures. Use of self-reported measures is vulnerable to the “common method bias”, i.e., spurious effects due to the measurement instruments rather than to the constructs being measured (Podsakoff et al. 2003), which can be addressed with a multitrait–multimethod study in which the same research participants are measured on multiple constructs using multiple methods or instruments (Bagozzi and Yi 1993). In particular, the use of self-report questionnaires to measure empathy is a major limitation, future studies shall consider using performance tasks such as the Multifaceted Empathy Test (Dziobek et al., 2008) for more in-depth measurement of empathy. The use of MAAS as a measure of mindfulness is also a major limitation; concerns have been raised in the literature with regard to the disadvantages of MAAS (Van Dam et al. 2010; Grossman 2011), e.g., it does not measure the acceptance (Sauer et al. 2013) nor the non-judgment (Baer et al. 2006) aspects of mindfulness, furthermore, its primarily negative wording and measurement of “inattentiveness” (Van Dam et al. 2010) limit its measurement of mindfulness to a very specific aspect: “acting with awareness” (Coffey and Hartman 2008); to effectively measure mindfulness, future research shall use other approaches that provide a comprehensive examination of mindfulness.
Supplementary Material
Figure 1:
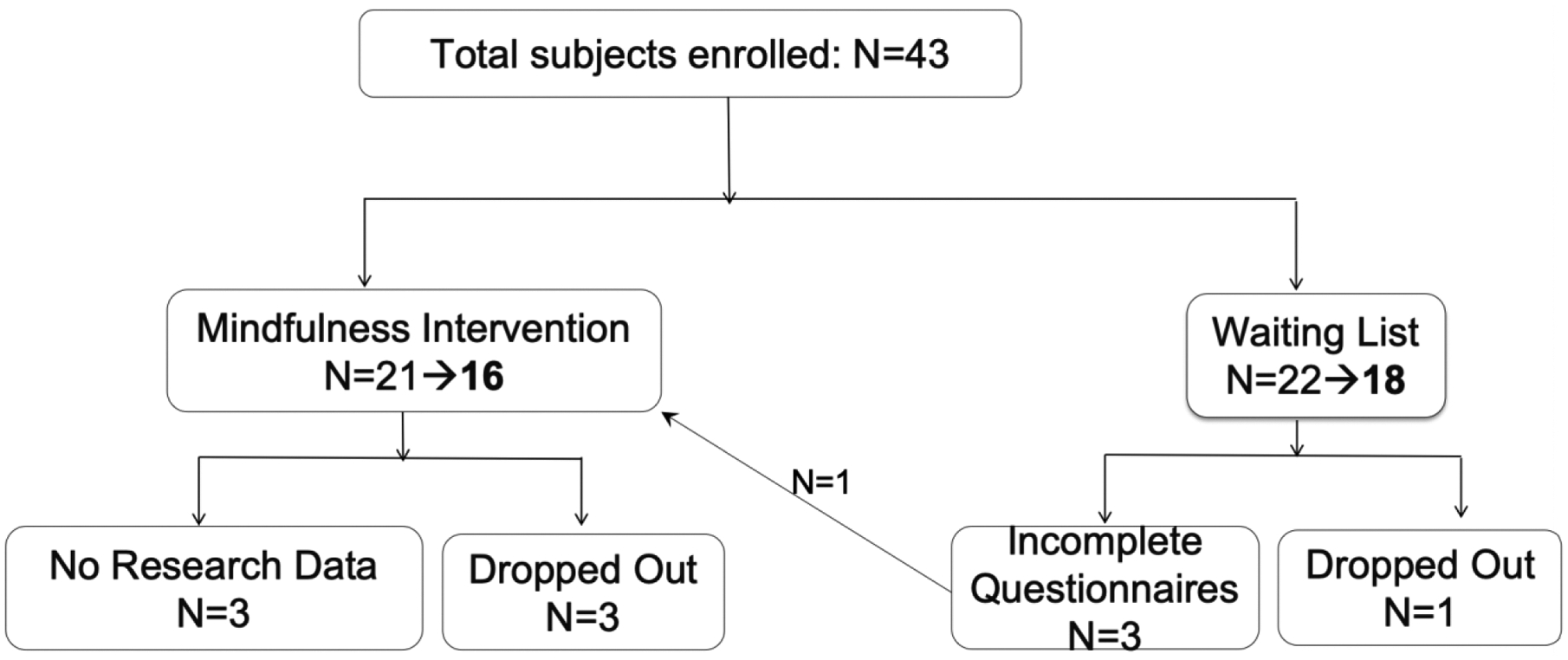
Flow chart of participant enrollment and retention information. Numbers in bold after the arrows are final participant numbers in data analyses.
Acknowledgement
We thank Zayda Vallejo for assistance with modification of the Mindfulness Based Stress Reduction program into the trauma-sensitive mindfulness-based intervention used in the current study, and we thank Lauri J Klein and David Schouela for teaching the intervention sessions. We thank Alaptagin Khan for performing clinical interviews.
Funding
This study was supported by funding from the Mind and Life Institute. The first author was supported by funding from NIH (grant number: 5K01AT009085) while working on this manuscript.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Disclosures
All authors declare no conflict of interest.
Research involving human participants
The present study was approved by the Institutional Review Board (IRB) of Partners HealthCare (IRB#: 2014P000295), which is the IRB for Massachusetts General Hospital, McLean Hospital, and several other major local hospitals.
Informed consent
Informed consent was obtained from all research subjects after the research procedure and all potential risks were explained face-to-face to subjects by research staff. IRB approved informed consent forms were signed by all subjects in the present study.
References
- Alink LR, Cicchetti D, Kim J, & Rogosch FA (2012). Longitudinal associations among child maltreatment, social functioning, and cortisol regulation. Developmental psychology, 48(1), 224–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardizzi M, Umiltà MA, Evangelista V, Di Liscia A, Ravera R, & Gallese V (2016). Less empathic and more reactive: the different impact of childhood maltreatment on facial mimicry and vagal regulation. PLoS One, 11(9), e0163853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong KA, Khawaja NG, & Oei TP (2006). Confirmatory factor analysis and psychometric properties of the Anxiety Sensitivity Index-Revised in clinical and normative populations. European Journal of Psychological Assessment, 22(2), 116–125. [Google Scholar]
- Ashley V, Honzel N, Larsen J, Justus T, & Swick D (2013). Attentional bias for trauma-related words: exaggerated emotional Stroop effect in Afghanistan and Iraq war veterans with PTSD. BMC Psychiatry, 13(1), 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. [DOI] [PubMed] [Google Scholar]
- Bagozzi RP, & Yi Y (1993). Multitrait–multimethod matrices in consumer research: Critique and new developments. Journal of Consumer Psychology, 2(2), 143–170. [Google Scholar]
- Barnes S, Brown KW, Krusemark E, Campbell WK, & Rogge RD (2007). The role of mindfulness in romantic relationship satisfaction and responses to relationship stress. Journal of Marital and Family Therapy, 33(4), 482–500. [DOI] [PubMed] [Google Scholar]
- Beauchemin J, Hutchins TL, & Patterson F (2008). Mindfulness meditation may lessen anxiety, promote social skills, and improve academic performance among adolescents with learning disabilities. Complementary Health Practice Review, 13(1), 34–45. [Google Scholar]
- Beck JG, Grant DM, Clapp JD, & Palyo SA (2009). Understanding the interpersonal impact of trauma: Contributions of PTSD and depression. Journal of Anxiety Disorders, 23(4), 443–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beddoe AE, & Murphy SO (2004). Does mindfulness decrease stress and foster empathy among nursing students? Journal of Nursing Education, 43(7), 305–312. [DOI] [PubMed] [Google Scholar]
- Bellet PS, & Maloney MJ (1991). The importance of empathy as an interviewing skill in medicine. JAMA, 266(13), 1831–1832. [PubMed] [Google Scholar]
- Benarous X, Guilé J-M, Consoli A, & Cohen D (2015). A systematic review of the evidence for impaired cognitive theory of mind in maltreated children. Frontiers in Psychiatry, 6, 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson KR, Downey G, Rafaeli E, Coifman KG, & Paquin NL (2011). The rejection–rage contingency in borderline personality disorder. Journal of Abnormal Psychology, 120(3), 681–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson KR, Gregory WE, Glaser E, Romirowsky A, Rafaeli E, Yang X, et al. (2016). Impulsivity, rejection sensitivity, and reactions to stressors in borderline personality disorder. Cognitive Therapy and Research, 40(4), 510–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson KR, Gyurak A, Ayduk Ö, Downey G, Garner MJ, Mogg K, et al. (2009). Rejection sensitivity and disruption of attention by social threat cues. Journal of Research in Personality, 43(6), 1064–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein D, & Fink L (1998). Childhood Trauma Questionnaire: A retrospective self-report. San Antonio, TX:The Psychological Corporation. [Google Scholar]
- Birnie K, Speca M, & Carlson LE (2010). Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR). Stress and Health, 26(5), 359–371. [Google Scholar]
- Bishop SJ (2007). Neurocognitive mechanisms of anxiety: an integrative account. Trends in Cognitive Sciences, 11(7), 307–316. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research And Therapy, 34(8), 669–673. [DOI] [PubMed] [Google Scholar]
- Block-Lerner J, Adair C, Plumb JC, Rhatigan DL, & Orsillo SM (2007). The case for mindfulness-based approaches in the cultivation of empathy: Does nonjudgmental, present-moment awareness increase capacity for perspective-taking and empathic concern? Journal of Marital and Family Therapy, 33(4), 501–516. [DOI] [PubMed] [Google Scholar]
- Boyd JE, Lanius RA, & McKinnon MC (2018). Mindfulness-based treatments for posttraumatic stress disorder: a review of the treatment literature and neurobiological evidence. Journal of Psychiatry and Neuroscience, 43(1), 7–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Koenen KC, Luo Z, Agnew-Blais J, Swanson S, Houts RM, et al. (2014). Childhood maltreatment, juvenile disorders and adult post-traumatic stress disorder: a prospective investigation. Psychological Medicine, 44(9), 1937–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. [DOI] [PubMed] [Google Scholar]
- Butler JC, Doherty MS, & Potter RM (2007). Social antecedents and consequences of interpersonal rejection sensitivity. Personality and Individual Differences, 43(6), 1376–1385. [Google Scholar]
- Clark DM (1999). Anxiety disorders: Why they persist and how to treat them. Behaviour Research and Therapy, 37(1), S5. [DOI] [PubMed] [Google Scholar]
- Cliffordson C (2001). Parents’ judgments and students’ self-judgments of empathy: The structure of empathy and agreement of judgments based on the interpersonal reactivity index (IRI). European Journal of Psychological Assessment, 17(1), 36–47. [Google Scholar]
- Coffey KA, & Hartman M (2008). Mechanisms of action in the inverse relationship between mindfulness and psychological distress. Complementary Health Practice Review, 13(2), 79–91. [Google Scholar]
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, & Maughan B (2007). Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse & Neglect, 31(3), 211–229. [DOI] [PubMed] [Google Scholar]
- Contardi A, Farina B, Fabbricatore M, Tamburello S, Scapellato P, Penzo I, et al. (2013). Difficulties in emotion regulation and personal distress in young adults with social anxiety. Rivista Di Psichiatria, 48(2), 155–161 [DOI] [PubMed] [Google Scholar]
- Davis MH (1980). A multidimensional approach to individual differences in empathy. JSAS Catalog of Selected Documents in Psychology, 10, 85. [Google Scholar]
- Davis MH (1983). Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology, 44(1), 113–126. [Google Scholar]
- Dekeyser M, Raes F, Leijssen M, Leysen S, & Dewulf D (2008). Mindfulness skills and interpersonal behaviour. Personality and Individual Differences, 44(5), 1235–1245. [Google Scholar]
- DeWall CN, & Baumeister RF (2006). Alone but feeling no pain: Effects of social exclusion on physical pain tolerance and pain threshold, affective forecasting, and interpersonal empathy. Journal of Personality and Social Psychology, 91(1), 1–15. [DOI] [PubMed] [Google Scholar]
- Dziobek I, Rogers K, Fleck S, et al. Dissociation of cognitive and emotional empathy in adults with Asperger syndrome using the Multifaceted Empathy Test (MET). Journal of Autism and Developmental Disorders. 2008; 38(3), 464–473. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Flook L, Goldberg SB, Pinger L, & Davidson RJ (2015). Promoting prosocial behavior and self-regulatory skills in preschool children through a mindfulness-based kindness curriculum. Developmental Psychology, 51(1), 44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis KJ, & Wolfe DA (2008). Cognitive and emotional differences between abusive and non-abusive fathers. Child Abuse & Neglect, 32(12), 1127–1137. [DOI] [PubMed] [Google Scholar]
- Gilet A-L, Mella N, Studer J, Grühn D, & Labouvie-Vief G (2013). Assessing dispositional empathy in adults: A French validation of the Interpersonal Reactivity Index (IRI). Canadian Journal of Behavioural Science, 45(1), 42–48. [Google Scholar]
- Grossman P (2011). Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology’s (re) invention of mindfulness: Comment on Brown et al.(2011). Psychological assessment, 23(4), 1034–1040. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoglund CL, & Nicholas KB (1995). Shame, guilt, and anger in college students exposed to abusive family environments. Journal of Family Violence, 10(2), 141–157. [Google Scholar]
- Joss D, Khan A, Lazar SW, & Teicher MH (2019). Effects of a mindfulness-based intervention on self-compassion and psychological health among young adults with a history of childhood maltreatment. Frontiers in Psychology, 10, 2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: Using the wisdom of your body and mind in everyday life. New York: Delacorte. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. (1987). The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry, 44(6), 540–548. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Finch A, & Montgomery L (1978). Vicarious anxiety: A systematic evaluation of a vicarious threat to self-esteem. Journal of Consulting and Clinical Psychology, 46(5), 997–1008. [DOI] [PubMed] [Google Scholar]
- Khan A, McCormack HC, Bolger EA, McGreenery CE, Vitaliano G, Polcari A, et al. (2015). Childhood maltreatment, depression, and suicidal ideation: critical importance of parental and peer emotional abuse during developmental sensitive periods in males and females. Frontiers in Psychiatry, 6, 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26(5), 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrough E, Magyari T, Langenberg P, Chesney M, & Berman B (2010). Mindfulness intervention for child abuse survivors. Journal of Clinical Psychology, 66(1), 17–33. [DOI] [PubMed] [Google Scholar]
- King AP, Erickson TM, Giardino ND, Favorite T, Rauch SA, Robinson E, et al. (2013). A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depression and Anxiety, 30(7), 638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krans J, de Bree J, & Bryant RA (2014). Autobiographical memory bias in social anxiety. Memory, 22(8), 890–897. [DOI] [PubMed] [Google Scholar]
- Kristeller JL, & Johnson T (2005). Cultivating loving kindness: A two-stage model of the effects of meditation on empathy, compassion, and altruism. Zygon®, 40(2), 391–408. [Google Scholar]
- Leppma M, & Young ME (2016). Loving-kindness meditation and empathy: A wellness group intervention for counseling students. Journal of Counseling & Development, 94(3), 297–305. [Google Scholar]
- Liem JH, & Boudewyn AC (1999). Contextualizing the effects of childhood sexual abuse on adult self-and social functioning: An attachment theory perspective. Child Abuse & Neglect, 23(11), 1141–1157. [DOI] [PubMed] [Google Scholar]
- Locher SC, Barenblatt L, Fourie MM, Stein DJ, & Gobodo-Madikizela P (2014). Empathy and childhood maltreatment: A mixed-methods investigation. Annals of Clinical Psychiatry, 26(2), 97–110. [PubMed] [Google Scholar]
- Maneta E, Cohen S, Schulz M, & Waldinger R (2015). Linkages between childhood emotional abuse and marital satisfaction: The mediating role of empathic accuracy for hostile emotions. Child Abuse & Neglect, 44, 8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza M, Tempesta D, Pino MC, Nigri A, Catalucci A, Guadagni V, et al. (2015). Neural activity related to cognitive and emotional empathy in post-traumatic stress disorder. Behavioural Brain Research, 282, 37–45. [DOI] [PubMed] [Google Scholar]
- McFarlane AC, & Bookless C (2001). The effect of PTSD on interpersonal relationships: Issues for emergency service workers. Sexual and Relationship Therapy, 16(3), 261–267. [Google Scholar]
- Mielke EL, Neukel C, Bertsch K, Reck C, Möhler E, & Herpertz SC (2016). Maternal sensitivity and the empathic brain: Influences of early life maltreatment. Journal of Psychiatric Research, 77, 59–66. [DOI] [PubMed] [Google Scholar]
- Mogg K, Millar N, & Bradley BP (2000). Biases in eye movements to threatening facial expressions in generalized anxiety disorder and depressive disorder. Journal of Abnormal Psychology, 109(4), 695–704. [DOI] [PubMed] [Google Scholar]
- Morrison AS, Mateen MA, Brozovich FA, Zaki J, Goldin PR, Heimberg RG, et al. (2016). Empathy for positive and negative emotions in social anxiety disorder. Behaviour Research and Therapy, 87, 232–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller J, Moergeli H, & Maercker A (2008). Disclosure and social acknowledgement as predictors of recovery from posttraumatic stress: A longitudinal study in crime victims. The Canadian Journal of Psychiatry, 53(3), 160–168. [DOI] [PubMed] [Google Scholar]
- Nietlisbach G, & Maercker A (2009). Social cognition and interpersonal impairments in trauma survivors with PTSD. Journal of Aggression, Maltreatment & Trauma, 18(4), 382–402. [Google Scholar]
- Nietlisbach G, Maercker A, Rösler W, & Haker H (2010). Are empathic abilities impaired in posttraumatic stress disorder? Psychological Reports, 106(3), 832–844. [DOI] [PubMed] [Google Scholar]
- O’Connor LE, Berry JW, Weiss J, & Gilbert P (2002). Guilt, fear, submission, and empathy in depression. Journal of Affective Disorders, 71(1–3), 19–27. [DOI] [PubMed] [Google Scholar]
- Paivio SC, & Laurent C (2001). Empathy and emotion regulation: Reprocessing memories of childhood abuse. Journal of Clinical Psychology, 57(2), 213–226. [DOI] [PubMed] [Google Scholar]
- Peters JR, Eisenlohr-Moul TA, & Smart LM (2016). Dispositional mindfulness and rejection sensitivity: The critical role of nonjudgment. Personality and Individual Differences, 93, 125–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson RA, & Heilbronner RL (1987). The anxiety sensitivity index: Construct validity and factor analytic structure. Journal of Anxiety Disorders, 1(2), 117–121. [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee J-Y, & Podsakoff NP (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of applied psychology, 88(5), 879–903. [DOI] [PubMed] [Google Scholar]
- Prino CT, & Peyrot M (1994). The effect of child physical abuse and neglect on aggressive, withdrawn, and prosocial behavior. Child Abuse & Neglect, 18(10), 871–884. [DOI] [PubMed] [Google Scholar]
- Purdie V, & Downey G (2000). Rejection sensitivity and adolescent girls’ vulnerability to relationship-centered difficulties. Child Maltreatment, 5(4), 338–349. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, & McNally RJ (1986). Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy, 24(1), 1–8. [DOI] [PubMed] [Google Scholar]
- Rogers K, Dziobek I, Hassenstab J, Wolf OT, & Convit A (2007). Who cares? Revisiting empathy in Asperger syndrome. Journal of Autism and Developmental Disorders, 37(4), 709–715. [DOI] [PubMed] [Google Scholar]
- Romero-Canyas R, Downey G, Berenson K, Ayduk O, & Kang NJ (2010). Rejection sensitivity and the rejection–hostility link in romantic relationships. Journal of Personality, 78(1), 119–148. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Weathers FW, King LA, & King DW (2002). Male war-zone veterans’ perceived relationships with their children: The importance of emotional numbing. Journal of Traumatic Stress, 15(5), 351–357. [DOI] [PubMed] [Google Scholar]
- Sahdra BK, Ciarrochi J, & Parker PD (2016). Nonattachment and mindfulness: Related but distinct constructs. Psychological Assessment, 28(7), 819–829. [DOI] [PubMed] [Google Scholar]
- Sahdra BK, Ciarrochi J, Parker PD, Basarkod G, Bradshaw EL, & Baer R (2017). Are people mindful in different ways? Disentangling the quantity and quality of mindfulness in latent profiles and exploring their links to mental health and life effectiveness. European Journal of Personality, 31(4), 347–365. [Google Scholar]
- Sahdra BK, Ciarrochi J, Parker PD, Marshall S, & Heaven P (2015). Empathy and nonattachment independently predict peer nominations of prosocial behavior of adolescents. Frontiers in Psychology, 6, 263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahdra BK, Shaver PR, & Brown KW (2010). A scale to measure nonattachment: A Buddhist complement to Western research on attachment and adaptive functioning. Journal of Personality Assessment, 92(2), 116–127. [DOI] [PubMed] [Google Scholar]
- Santorelli SF, Kabat-Zinn J, Blacker M, Meleo-Meyer F, & Koerbel L (2017). Mindfulness-based stress reduction (MBSR) authorized curriculum guide. Center for Mindfulness in Medicine, Health Care, and Society (CFM). University of Massachusetts Medical School. [Google Scholar]
- Sauer S, Walach H, Schmidt S, Hinterberger T, Lynch S, Büssing A, et al. (2013). Assessment of mindfulness: Review on state of the art. Mindfulness, 4(1), 3–17. [Google Scholar]
- Simon NM, Herlands NN, Marks EH, Mancini C, Letamendi A, Li Z, et al. (2009). Childhood maltreatment linked to greater symptom severity and poorer quality of life and function in social anxiety disorder. Depression and Anxiety, 26(11), 1027–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder CR, Lopez SJ, & Pedrotti JT (2011). Positive psychology: The scientific and practical explorations of human strengths, 2nd ed. Thousand Oaks, CA, US: Sage Publications, Inc. [Google Scholar]
- Stuewig J, & McCloskey LA (2005). The relation of child maltreatment to shame and guilt among adolescents: Psychological routes to depression and delinquency. Child Maltreatment, 10(4), 324–336. [DOI] [PubMed] [Google Scholar]
- Teicher MH, & Parigger A (2015). The ‘Maltreatment and Abuse Chronology of Exposure’(MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One, 10(2), e0117423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, & Samson JA (2013). Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. American Journal of Psychiatry, 170(10), 1114–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallejo Z, & Amaro H (2009). Adaptation of mindfulness-based stress reduction program for addiction relapse prevention. The Humanistic Psychologist, 37(2), 192–206. [Google Scholar]
- Van Dam NT, Earleywine M, & Borders A (2010). Measuring mindfulness? An item response theory analysis of the Mindful Attention Awareness Scale. Personality and individual differences, 49(7), 805–810. [Google Scholar]
- van Der Kolk BA, & Saporta J (1991). The biological response to psychic trauma: Mechanisms and treatment of intrusion and numbing. Anxiety Research, 4(3), 199–212. [Google Scholar]
- Vidyanidhi K, & Sudhir PM (2009). Interpersonal sensitivity and dysfunctional cognitions in social anxiety and depression. Asian Journal of Psychiatry, 2(1), 25–28. [DOI] [PubMed] [Google Scholar]
- Wachs K, & Cordova JV (2007). Mindful relating: Exploring mindfulness and emotion repertoires in intimate relationships. Journal of Marital and Family Therapy, 33(4), 464–481. [DOI] [PubMed] [Google Scholar]
- Wagner B, Keller V, Knaevelsrud C, & Maercker A (2012). Social acknowledgement as a predictor of post-traumatic stress and complicated grief after witnessing assisted suicide. International Journal of Social Psychiatry, 58(4), 381–385. [DOI] [PubMed] [Google Scholar]
- Wilhelm K, Boyce P, & Brownhill S (2004). The relationship between interpersonal sensitivity, anxiety disorders and major depression. Journal of Affective Disorders, 79(1–3), 33–41. [DOI] [PubMed] [Google Scholar]
- Wright MOD, Crawford E, & Del Castillo D (2009). Childhood emotional maltreatment and later psychological distress among college students: The mediating role of maladaptive schemas. Child Abuse & Neglect, 33(1), 59–68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


