Abstract
Obesity is a constantly increasing health problem worldwide. It is associated with a systemic low-grade inflammation, which contributes to the development of metabolic disorders and comorbidities such as type 2 diabetes. Diet has an important role in the prevention of obesity and its adverse health effects; as a part of healthy diet, polyphenol-rich berries, such as lingonberry (Vaccinium vitis-idaea L.) have been proposed to have health-promoting effects. In the present study, we investigated the effects of lingonberry supplementation on high-fat diet induced metabolic and inflammatory changes in a mouse model of obesity. Thirty male C57BL/6N mice were divided into three groups (n = 10/group) to receive low-fat (LF), high-fat (HF) and lingonberry-supplemented high-fat (HF+LGB) diet for six weeks. Low-fat and high-fat diet contained 10% and 46% of energy from fat, respectively. Lingonberry supplementation prevented the high-fat diet induced adverse changes in blood cholesterol and glucose levels and had a moderate effect on the weight and visceral fat gain, which were 26% and 25% lower, respectively, in the lingonberry group than in the high-fat diet control group. Interestingly, lingonberry supplementation also restrained the high-fat diet induced increases in the circulating levels of the proinflammatory adipocytokine leptin (by 36%) and the inflammatory acute phase reactant serum amyloid A (SAA; by 85%). Similar beneficial effects were discovered in the hepatic expression of the inflammatory factors CXCL-14, S100A10 and SAA by lingonberry supplementation. In conclusion, the present results indicate that lingonberry supplementation significantly prevents high-fat diet induced metabolic and inflammatory changes in a murine model of obesity. The results encourage evaluation of lingonberries as a part of healthy diet against obesity and its comorbidities.
1. Introduction
The prevalence of obesity, metabolic syndrome and type 2 diabetes has increased rapidly worldwide during the last decades. Reasons can be found in changing lifestyles, which lead to reduced physical activity and obesogenic diet. It seems that obesity is continuing to be an increasing global health burden; according to the WHO statistics, 13% of adults aged 18 and over (corresponding to over 650 million people) were obese (body mass index BMI > 30 kg/m2) and 39% overweight in 2016 [1]. Obesity is a complex chronic disorder with a multifactorial etiology, involving genetics, hormones, diet and environment [2], and it has a major impact on various metabolic and (patho)physiological functions in the human body. Obesity is a major risk factor and underlying condition in the progression of many metabolic disorders, particularly type 2 diabetes, cardiovascular diseases and cancer, through its effects on the development of, for instance hypertension, insulin resistance, nonalcoholic fatty liver disease and inflammation [3,4].
Adipose tissue is an active tissue regulating various physiological and pathological processes, including immunity and inflammation. It is therefore no longer considered only as a passive energy storage. Adipose tissue produces and releases several hormone-like factors called adipokines, and many of them have pro- or anti-inflammatory properties [2,5]. In obese adipose tissue, immune cells secreting pro-inflammatory substances increase in number while those producing anti-inflammatory substances have been shown to decrease. This imbalance is responsible for the obesity induced low-grade inflammation and insulin resistance in the body [3].
Diet has an important role in the prevention and treatment of obesity, type 2 diabetes and other obesity-related diseases. Diets containing plenty of polyphenol-rich vegetables have been shown to lower the risk of obesity-related comorbidities [6–8]. Berries are specifically rich in various polyphenols [9,10]. Diets containing berries are associated with lowered risk of type 2 diabetes, probably due to the flavonoids [11], anthocyanidins [8,12,13] or other polyphenols [14] present in berries. Several intervention studies have shown beneficial effects of berries also on inflammation and cardiovascular diseases [15].
Lingonberry (Vaccinium vitis-idaea L.) has been reported to have promising health-beneficial effects and anti-inflammatory properties in experimental models [16–19]. Lingonberries / lingonberry extracts were found to exhibit antidiabetic potential in various in vitro tests [20] and beneficial metabolic effects in mice exposed to high-fat diet [21–25]. Lingonberries are rich in dietary polyphenols with high antioxidant activities [16,26–28] and contain also essential omega-3 fatty acids [29] and plant sterols [30,31], which may contribute to their health-promoting effects. Lingonberries are commonly consumed in the Nordic countries and commercially available in many different forms. They are also the most generally collected and commercially utilized wild berries in Finland [32].
In the present study, we aimed to investigate the effects of lingonberry supplementation on metabolic and inflammatory changes in high-fat diet induced experimental obesity in mice to extend the current understanding on the health benefits of lingonberries. As the test material, we used commercially available air-dried lingonberry powder made from Finnish lingonberries.
2. Materials and methods
Animals and study design
Male C57BL/6N mice (Scanbur Research A/S, Karlslunde, Denmark), 8 weeks of age and 24.3±0.2g of weight at the beginning of the experiment, were divided into three groups of 10 mice, and housed two mice per cage in the animal facility of the Tampere University under standard conditions (12/12h light/dark cycle, 22±1 °C temperature, and 50–60% humidity) with food and water provided ad libitum.
The mice were fed with normal low-fat diet (LF, 10 kcal% fat), with high-fat diet (HF, 46 kcal% fat) or with high-fat diet supplemented with air-dried lingonberry (Vaccinium vitis-idaea L.) powder (HF + LGB, 20% w/w) for 6 weeks. Both high-fat diets contained 46% of energy from fat and 36% from carbohydrate, while the low-fat diet had 10% of energy from fat and 72% from carbohydrate (Table 1). Otherwise the custom-made pelleted diets (Research Diets, Inc, New Brunswick, NJ, USA) were matched for protein (18% of energy from protein), fiber, vitamin and trace element contents considering the composition of the lingonberry powder. Air-dried lingonberry powder (100 g powder corresponds to ca 900 g fresh berries) was produced from Finnish lingonberries by Kiantama Ltd (Suomussalmi, Finland).
Table 1. Composition of the experimental diets.
| LF | HF | HF+LGB | |
|---|---|---|---|
| Calculated energy (kcal) | |||
| Protein | 716 | 716 | 716 |
| Carbohydrate | 2840 | 1422 | 1422 |
| Starch | 2110 | 691 | 691 |
| Sugar | 730 | 731 | 731 |
| Fat | 405 | 1823 | 1823 |
| Total energy | 3961 | 3961 | 3961 |
| Calculated energy per gram diet (kcal/g) | 3.60 | 4.39 | 4.30 |
| Calculated Energy (kcal%) | |||
| Protein | 18 | 18 | 18 |
| Carbohydrate | 72 | 36 | 36 |
| Fat | 10 | 46 | 46 |
| Fiber (g%) | 9 | 10 | 10 |
| Lingonberry powder (g) | 0 | 0 | 184* |
| Ingredients (g) | |||
| (+ from LGB powder) | |||
| Casein | 200 | 200 | 194 (+ 6) total: 200 |
| L-Cystine | 3 | 3 | 3 |
| Corn Starch | 452 | 73 | 31 (+ 42) total: 73 |
| Maltodextrin 10 | 75 | 100 | 100 |
| Sucrose | 173 | 173 | 103 (+ 70) total: 173 |
| Cellulose | 94 | 94 | 50 (+ 44) total: 94 |
| Soybean Oil | 25 | 25 | 24 (+ 1) total: 25 |
| Lard | 20 | 178 | 178 |
| Mineral Mix S10026 | 10 | 10 | 10 |
| DiCalcium Phosphate | 13 | 13 | 13 |
| Calcium Carbonate | 6 | 6 | 6 |
| Potassium Citrate | 17 | 17 | 17 |
| Vitamin Mix V10001 | 10 | 10 | 10 |
| Choline Bitartrate | 2 | 2 | 2 |
LF = low-fat diet, HF = high-fat diet, HF+LGB = lingonberry-supplemented high-fat diet
*Nutrient content/100 g lingonberry powder: fat 0.8 g, carbohydrates 61 g (of which sugars 38 g), fiber 24 g, protein 3 g
Body weight of the mice and food consumption was monitored weekly. At the end of the study, 6h-fasted mice were anesthetized with isoflurane (Oriola Corp., Espoo, Finland), blood glucose was measured and blood was collected by cardiac puncture. Tissue samples were collected for further analyses. The study was approved by the National Animal Experimental Board (permission number ESAVI- 984/04.10.07/2018) and the experiments were carried out in accordance with the EU legislation for the protection of animals used for scientific purposes (Directive 2010/63/EU).
Blood samples and analyses
Six-hour fasting (morning fast) blood glucose levels in mice were measured from the tip of the tail with Contour Next One (Oy Diabet Ab, Lemu, Finland). Blood collected by cardiac puncture was centrifuged for 15 minutes at 1500 x g after 30 minutes incubation at room temperature, and obtained serum was immediately storaged at -80 °C. Serum triglyceride and total cholesterol levels, and alanine aminotransferase (ALT) activity were measured by fluorometric assays (Abcam, Cambridge, UK). Enzyme-linked immunoassays were used to measure the concentrations of leptin, resistin and adiponectin (R&D Systems Europe Ltd., Abingdon, UK), insulin (Mercodia Ltd., Uppsala, Sweden) and serum amyloid A (Tridelta Development Ltd., Maynooth, Ireland) in serum samples. Detection limits were 7.8 pg/mL for leptin and resistin, 15.6 pg/mL for adiponectin, 33 pmol/L for insulin and 16 ng/mL for SAA.
RNA extraction and qRT-PCR
Total RNA was extracted from liver using RNeasy Mini Kit (Qiagen Inc., Hilden, Germany). Briefly, samples stored immediately after collection in RNA Later® (Ambion, Thermo Fisher Scientific, Waltham, MA, USA) were weighed and maximum of 30 mg of tissue was cut into smaller pieces and homogenized with Qiashredder (Qiagen). RNA was extracted with RNeasy Mini Kit with on-column DNase digestion. RNA was transcribed to cDNA by using Maxima First Strand cDNA Synthesis Kit (Thermo Fisher Scientific) in 10 ul reaction volume and diluted 1:5 with RNase-free water. Quantitative PCR was performed using TaqMan Universal Master Mix and ABI Prism 7500 sequence detection system (Applied Biosystems, Foster City, CA, USA). The PCR cycling parameters were incubation at 50 °C for 2 minutes, incubation at 95 °C for 10 minutes, and thereafter 40 cycles of denaturation at 95 °C for 15 s and annealing and extension at 60 °C for 1 minute. Primers and probe for the housekeeping gene glyceraldehyde 3-phosphate dehydrogenase GAPDH) were GCATGGCCTTCCGTGTTC (forward, 300 nM), GATGTCATCATACTTGGCAGGTTT (reverse, 300nM) and TCGTGGATCTGACGTGCCGCC (probe, 150 nM); and TCGGAGGCTTAATTACACATGTTC (forward, 900 nM), CAAGTGCATCATCGTTGTTCATAC (reverse, 300 nM) and CAGAATTGCCATTGCACAACTCTTTTCTCA (probe, 200 nM) for interleukin 6 (IL-6). The sequences and concentrations were optimized according to the manufacturer’s guidelines in TaqMan Universal PCR Master Mix Protocol part number 4304449 revision C (Applied Biosystems). TaqMan Gene Expression assays for interleukin 1β (IL-1β, Mm00434228_m1), monocyte chemoattractant protein 1 (MCP-1, Mm00441242_m1), tumor necrosis alpha (TNF-α, Mm00443260_g1), glucose transporter 2 (GLUT2, Mm00446229_m1), serum amyloid A2 (SAA2, Mm04208126_mH), C-X-C motif chemokine ligand 14 (CXCL-14, Mm00444699_m1), S100 calcium-binding protein A10 (S100A10, Mm00501458_g1), and insulin receptor (Insr, Mm01211875_m1) were used (Thermo Fisher Scientific) and expression levels were calculated using the 2(−ΔΔCT) method. When calculating results, all of the mRNA expression levels were first normalized against GAPDH mRNA levels.
Statistics
Results are expressed as mean + standard error of mean (SEM). One-way and two-way ANOVA with Bonferroni’s post-test, and the analysis of covariance were performed using GraphPad InStat version 3.10 and GraphPad Prism 8 (GraphPad Software, San Diego, USA), and IBM SPSS Statistics version 25.0 (IBM Corporation, Armonk, NY, USA). Asterisks *, **, and *** indicate p values smaller than 0.05, 0.01 and 0.001, respectively.
3. Results
3.1. Weight gain
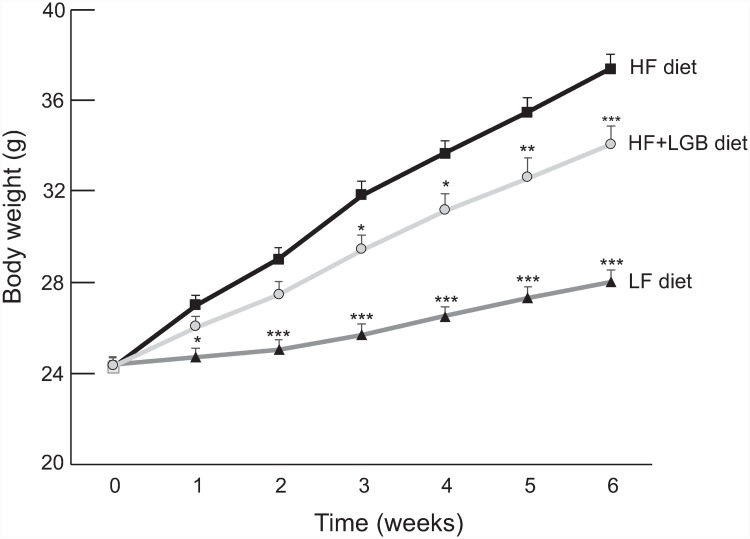
The weight of mice in the high-fat (HF) group increased considerably during the study as compared to the mice in the low-fat (LF) control group. Interestingly, lingonberry supplementation prevented significantly the high-fat diet induced weight gain (p < 0.001 between HF and HF+LGB groups). After 6 weeks, the average weight of the low-fat group was 28.0±0.4 g, 37.4±0.6 g in the high-fat group and 34.1±0.6 g in the lingonberry supplemented high-fat group, respectively (p < 0.001 between groups). The development of weight of the mice in the test groups is presented in the Fig 1.
Fig 1. Body weight gain of the mice during the study.
Animals received low-fat diet (LF diet, 10% of energy from fat, dark grey line), high-fat diet (HF diet, 46% of energy from fat, black line) or high-fat diet supplemented with lingonberry (HF + LGB diet, light grey line). Weight was measured once a week. The results are expressed as grams (g). Values represent mean + SEM, n = 10 mice per group. Repeated measures two-way ANOVA with Bonferroni post-test was used in the statistical analysis. Mean values significantly different from the high-fat group (HF diet) are marked with *p < 0.05, **p < 0.01 and ***p < 0.001.
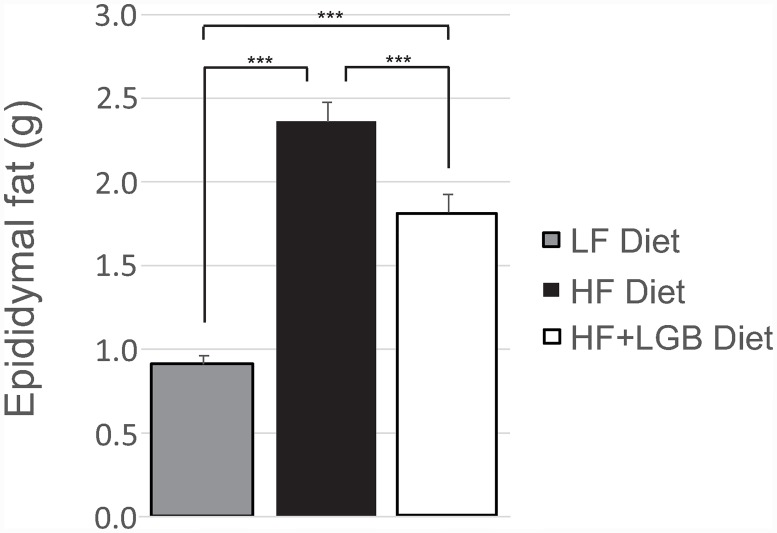
The amount of epididymal fat increased in the high-fat diet group, when compared to the low-fat control group (p < 0.001). Lingonberry supplementation prevented significantly the accumulation of epididymal fat when compared to the high-fat control group (p < 0.001). At the end of the study, the amount of epididymal fat was 2.4±0.1 g in the high-fat group and 1.8±0.1 g in the lingonberry supplemented high-fat group. Both high-fat groups had significantly (p < 0.001) higher amount of epididymal fat than the low-fat group (0.9±0.0 g; Fig 2). When the ratio of the epididymal fat to the whole-body mass was calculated, it was lower in the HF+LGB group than in the HF group (p < 0.01) suggesting that lingonberry supplementation prevents particularly the accumulation of the metabolically highly detrimental visceral adipose tissue. That was also supported by the fact that in the analysis of covariance when the body weight was set as a covariate, the epididymal fat mass was lower in the LF and the HF+LGB groups than in the HF group (p < 0.01).
Fig 2. The amount of epididymal fat of the mice at the end of the study.
Animals received low-fat diet (LF diet, 10% energy from fat, grey column), high-fat diet (HF diet, 46% energy from fat, black column) or high-fat diet supplemented with lingonberry (HF + LGB diet, white column). The amount of epididymal fat was measured at the end of the study. The results are expressed as grams (g). Values represent mean + SEM, n = 10 mice per group. One-way ANOVA with Bonferroni post-test was used in the statistical analysis. Differences between the groups are marked with ***p < 0.001.
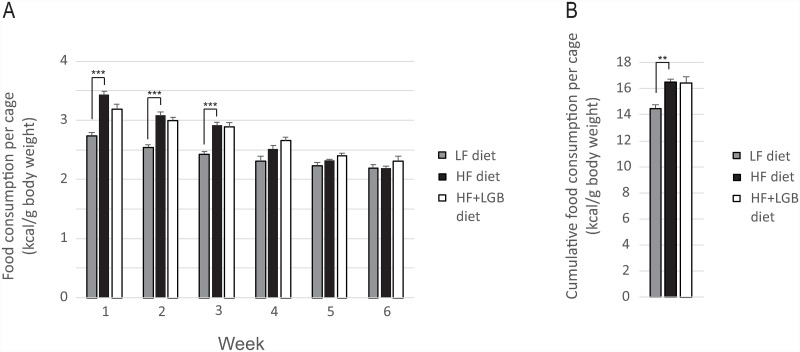
Food consumption (kcal/g body weight) was measured weekly and it did not differ between the high-fat and the lingonberry supplemented high-fat diet groups although energy intake in the low-fat diet group was lower, particularly during the first half of the study (Fig 3A). We also calculated the cumulative food consumption (kcal/g body weight) during the six weeks’ study: no difference was found between the high-fat and the lingonberry supplemented high-fat groups while the value in the low-fat group was lower (p < 0.01; Fig 3B). This result was reproduced in repeated measures analysis of covariance with body weight as a covariate.
Fig 3. Food consumption during the study.
Fig 3A shows the weekly and Fig 3B the cumulative food consumption during the six weeks’ study. Animals received low-fat diet (LF diet, 10% energy from fat, grey columns), high-fat diet (HF diet, 46% energy from fat, black columns) or high-fat diet supplemented with lingonberry (HF + LGB diet, white columns). Food consumption was measured once a week. The results are expressed as kcal/body weight in grams. Values represent mean + SEM, n = 10 mice per group; as the mice were housed two mice per cage, n = 5 was used in the statistical calculations. Repeated measures two-way ANOVA (Fig 3A) and one-way ANOVA (Fig 3B) with Bonferroni post-test was used in the statistical analysis. Differences between the groups are marked with **p<0.01 and ***p < 0.001.
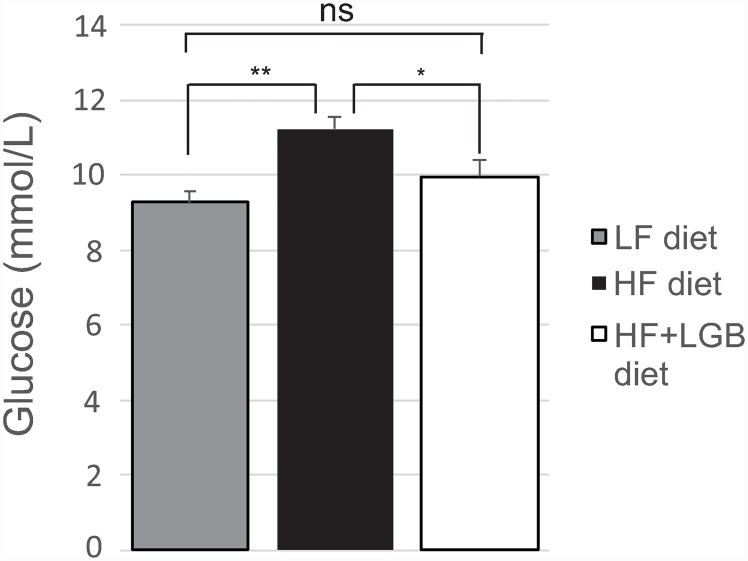
3.2. Glucose and insulin
Fasting blood glucose level at the end of the study was increased in the high-fat diet group, as compared to the low-fat control group (p < 0.01). Interestingly, in the lingonberry supplemented high-fat diet group, the glucose level (10.0±0.5 mmol/L) was lower than that in the high-fat control group (11.2±0.4 mmol/L; p < 0.05), and there was no statistically significant difference between the low-fat and the lingonberry supplemented high-fat groups (Fig 4).
Fig 4. The fasting blood glucose levels of mice at the end of the study.
Animals received low-fat diet (LF diet, 10% energy from fat, grey column), high-fat diet (HF diet, 46% energy from fat, black column) or high-fat diet supplemented with lingonberry (HF + LGB diet, white column). At the end of the study, blood samples for glucose measurements were collected after 6 h fasting. The results are expressed as mmol/L. Values represent mean + SEM, n = 10 mice per group. One-way ANOVA with Bonferroni post-test was used in the statistical analysis. Differences between the groups are marked with *p < 0.05, **p < 0.01 and ns = not significant.
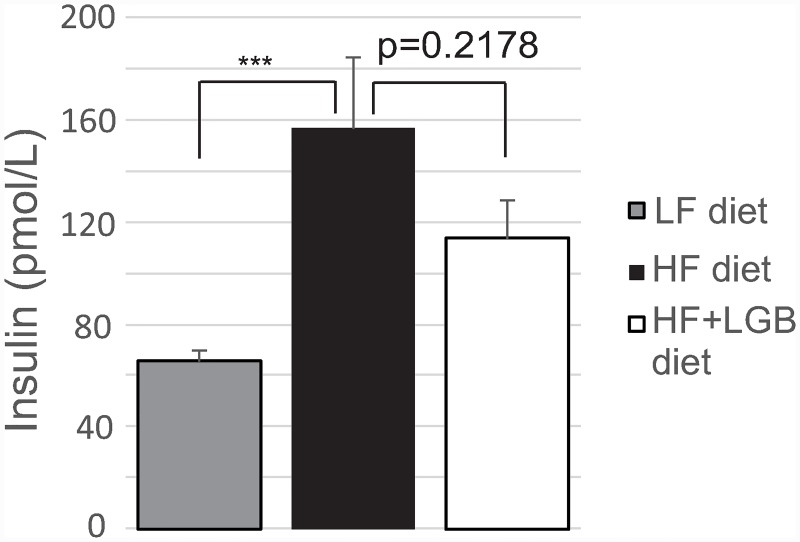
As expected, fasting insulin level was significantly higher in the high-fat group (156.5 pmol/L) as compared to the low-fat group (65.5 pmol/L; p < 0.001). In the lingonberry supplemented high-fat group, the insulin level (113.7 pmol/L) was lower than in the high-fat group, although the effect did not reach statistical significance (Fig 5).
Fig 5. The insulin levels of mice at the end of the study.
Animals received low-fat diet (LF diet, 10% energy from fat, grey column), high-fat diet (HF diet, 46% energy from fat, black column) or high-fat diet supplemented with lingonberry (HF + LGB diet, white column). At the end of the study, blood samples were collected after 6 h fasting and serum insulin concentrations were analyzed with ELISA. The results are expressed as pmol/L. Values represent mean + SEM, n = 10 mice per group. One-way ANOVA with Bonferroni post-test was used in the statistical analysis. Differences between the groups are marked with *** p < 0.001.
3.3. Cholesterol and triglycerides
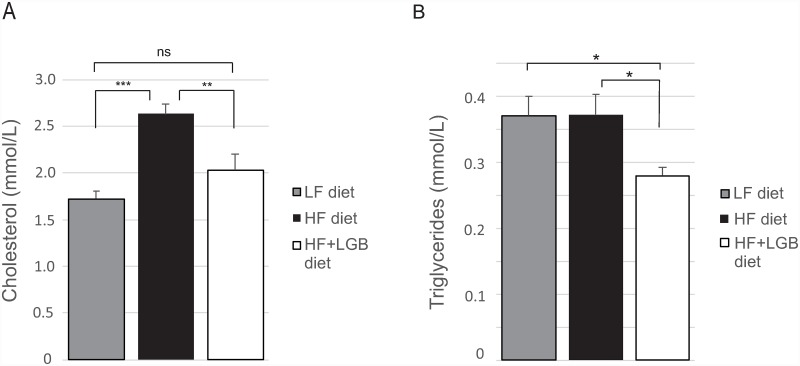
Cholesterol level was significantly increased in the high-fat group when compared to the low-fat group (p < 0.001) being 2.6±0.1 mmol/L in the high-fat group and 1.7±0.1 mmol/L in the low-fat group at the end of the study. Importantly, the cholesterol level in the lingonberry supplemented high-fat group (2.0±0.2 mmol/L) was significantly lower when compared to the high-fat group (p < 0.01). There was no statistically significant difference in the cholesterol levels between the low-fat and the lingonberry supplemented high-fat groups indicating that lingonberry supplementation prevented the high-fat diet induced increase in cholesterol levels (Fig 6A).
Fig 6. Cholesterol (A) and triglyceride (B) levels of mice at the end of the study.
Animals received low-fat diet (LF diet, 10% energy from fat, grey columns), high-fat diet (HF diet, 46% energy from fat, black columns) or high-fat diet supplemented with lingonberry (HF + LGB diet, white columns). At the end of the study, blood samples were collected after 6 h fasting and serum cholesterol and triglyceride concentrations were analyzed with fluorometric assays. The values are presented as mmol/L. Values represent mean + SEM, n = 10 mice per group. One-way ANOVA with Bonferroni post-test was used in the statistical analysis. Differences between the groups are marked with *p < 0.05, **p < 0.01, ***p < 0.001 and ns = not significant.
There were no differences in the triglyceride levels between the low-fat and high-fat groups whereas the triglyceride level in the lingonberry supplemented high-fat group was lower than that in the two other groups (p < 0.05; Fig 6B).
3.4. Adipokines and inflammatory factors
As expected, leptin levels were significantly higher in the high-fat group as compared to the low-fat group (p < 0.001). Leptin levels were lower in the lingonberry supplemented high-fat group (27.1±3.5 ng/mL) than in the high-fat control group (39.7±2.8 ng/mL; p < 0.01, Table 2). Interestingly, the statistically significant difference was also observed in weight-related values (1.1±0.1 ng/mL/body weight (g) in HF group vs. 0.8±0.1 ng/mL/body weight (g) in HF+LGB group, p < 0.01). In adiponectin, there was a trend towards decreased levels in the high-fat group when compared to low-fat control group (p = 0.277). Adiponectin level was maintained at normal levels with lingonberry supplementation. There were no significant differences in the resistin levels between the groups (Table 2).
Table 2. The circulating adipokine and serum amyloid A (SAA) levels, and alanine aminotransferase (ALT) activity of the mice at the end of the study.
| Low-fat (LF) | High-fat (HF) | High-fat + lingonberry (HF+LGB) | p-value between LF and HF | p-value between HF and HF+LGB | |
|---|---|---|---|---|---|
| Adiponectin (μg/mL) | 6.9 ± 0.2 | 6.4 ± 0.2 | 7.1 ± 0.3 | 0.277 | 0.100 |
| Leptin (ng/mL) | 4.6 ± 0.6 | 39.7 ± 2.8 | 27.1 ± 3.5 | < 0.001 | < 0.01 |
| Resistin (ng/mL) | 17.8 ± 1.4 | 16.8 ± 0.8 | 17.6 ± 0.9 | > 0.999 | > 0.999 |
| SAA (μg/mL) | 6.6 ± 0.6 | 11.7 ± 0.7 | 7.4 ± 0.4 | < 0.001 | < 0.001 |
| ALT (U/L) | 8.1 ± 0.6 | 14.1 ± 0.8 | 7.2 ± 0.2 | < 0.001 | < 0.001 |
Adiponectin, leptin, resistin and SAA concentrations were measured by ELISA, and ALT activity by fluorometric assay. The results are presented as mean ± SEM; n = 10 mice per group. One-way ANOVA with Bonferroni post-test was used in the statistical analysis.
The levels of the inflammatory acute phase reactant serum amyloid A (SAA) were increased (p < 0.001) in the high-fat diet group (11.7±0.7 μg/mL) as compared to the low-fat diet group (6.6±0.6 μg/mL). Importantly, the SAA levels in the lingonberry supplemented high-fat group (7.4±0.4 μg/mL) were significantly lower (p < 0.001) than those in the high-fat control group. Similarly, alanine aminotransferase activity was increased in the high-fat diet group as compared to the low-fat diet group (p<0.001) which was prevented by the lingonberry supplementation (p < 0.001) (Table 2).
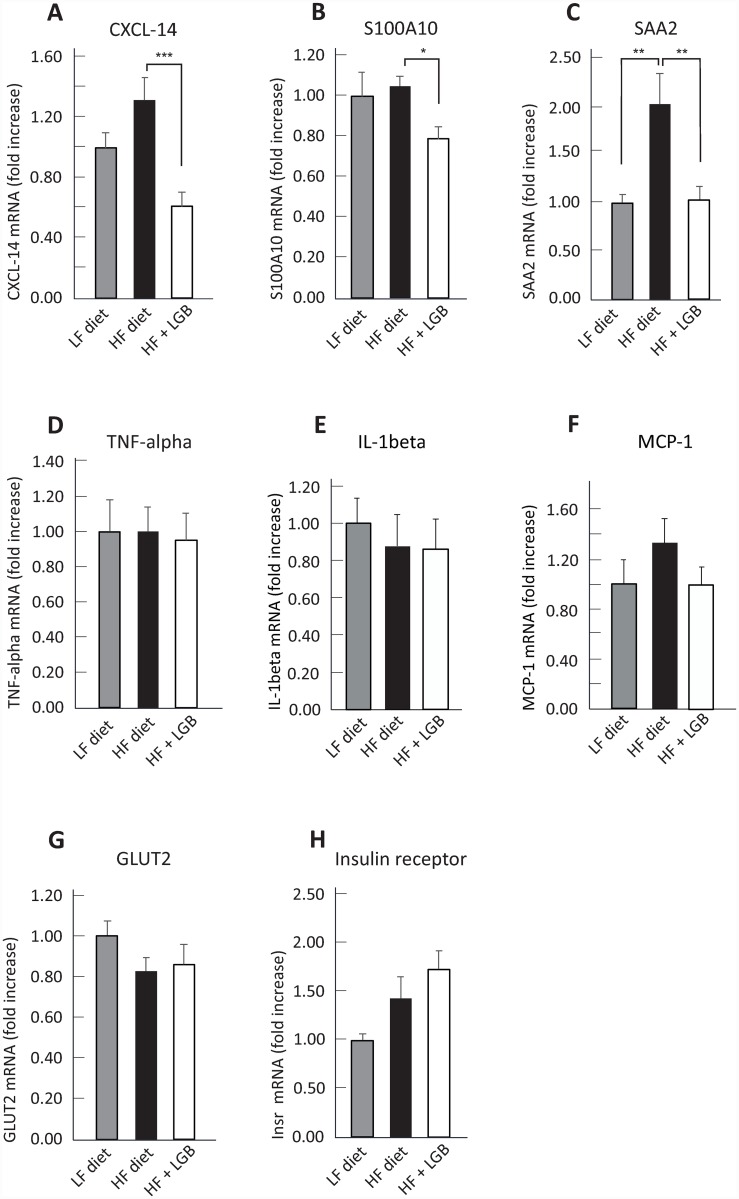
High-fat diet is known to induce metabolic and inflammatory changes in the liver. Therefore, we analyzed the expression of insulin receptor and glucose transporter GLUT2 as well as the inflammatory factors TNF-α, IL-1β, IL-6, MCP-1, SAA2, CXCL-14 and S100A10 in the liver by quantitative RT-PCR. As shown in the Fig 7, the hepatic expression of CXCL-14 (p < 0.001), S100A10 (p < 0.05), and SAA2 (p < 0.01) were significantly lower in the lingonberry supplemented high-fat diet group than in the high-fat control group, while IL-6 was under detection limit and no statistically significant differences in the expression of TNF-α, IL-1β, MCP-1, GLUT2 or insulin receptor were observed between the groups.
Fig 7. The expression of C-X-C motif chemokine ligand 14 (CXCL-14, A), S100 calcium-binding protein A10 (S100A10, B), serum amyloid A2 (SAA2, C), tumor necrosis alpha (TNF-α, D), interleukin 1β (IL-1β, E), monocyte chemoattractant protein 1 (MCP-1, F), glucose transporter 2 (GLUT2, G), and insulin receptor (H) in the liver.
Animals received low-fat diet (LF diet, 10% energy from fat, grey columns), high-fat diet (HF diet, 46% energy from fat, black columns) or high-fat diet supplemented with lingonberry (HF + LGB diet, white columns). At the end of the study, liver samples were collected after 6 h fasting and the expression of the genes of interest were measured with RT-PCR. After normalizing to the housekeeping gene glyceraldehyde 3-phosphate dehydrogenase (GAPDH), the expression level in each sample was compared to the mean expression level in the LF-group, which was set as 1. One-way ANOVA with Bonferroni post-test was used in the statistical analysis. Differences between the groups are marked with *p < 0.05, **p < 0.01 and ***p < 0.001.
Discussion
In the present study, we found that lingonberry supplementation prevented high-fat diet induced adverse effects on blood cholesterol, glucose and insulin levels as well as visceral fat gain in a murine model of obesity. In addition, the circulating levels of the pro-inflammatory adipocytokine leptin and the inflammatory acute phase reactant and biomarker serum amyloid A (SAA), as well as the alanine aminotransferase (ALT) activity were maintained at lower level by lingonberry supplementation, and the same was detected in hepatic expression of the inflammatory factors CXCL-14, S100A10 and SAA. To our knowledge, this is the first study in which such significant results have been obtained with an air-dried lingonberry powder. The results are remarkable also considering the rather short duration (6 weeks) of the study.
Obesity is a risk factor for glucose intolerance leading to diabetes, which is first detected as increased circulating insulin concentrations followed by increased fasting blood glucose levels [33,34]. In the present study, increased insulin and glucose levels were found already after six weeks on high-fat diet. Lingonberry supplementation prevented these effects. These findings are supported by previous studies with freeze-dried lingonberries and lingonberry extract on a longer follow-up [21–23,25,35] while bilberry supplementation did not have any effect on blood glucose levels [36]. Anthocyanins in the lingonberry powder could contribute to the beneficial effects on glucose tolerance as anthocyanin-rich supplements from Montmorency tart cherries have been reported to have insulin lowering effects in patients with metabolic syndrome [37] and purified blueberry anthocyanins reduced blood glucose levels in a murine model of obesity [38]. In the present study, lingonberry supplementation did not alter hepatic expression of the glucose transporter GLUT2 or insulin receptor. Further studies are needed to understand the mechanisms which mediate the positive effects of lingonberries on glucose tolerance in obesity.
Hyperlipidemia is another characteristic feature of obesity associated metabolic syndrome [4]. In the present study, lingonberry supplementation normalized the detrimental effects of the high-fat diet on the cholesterol levels, and triglycerides were also reduced. Proanthocyanidins present in lingonberries may explain, at least partly, the favorable effects on cholesterol levels [39–41]. In addition, the purified lingonberry anthocyanidin compound cyanidin-3-O-β-glucoside was found effective in decreasing total cholesterol levels in hypercholesterolemic ApoE deficient mice [42]. Lingonberries are also known to contain plant sterols at moderate levels of 20–30 mg/100 g of fresh weight [30,31] and they may contribute to the lipid lowering effects of lingonberries [43]. The lipid lowering effect seems to be characteristic for lingonberry among berries since freeze-dried blueberry and black raspberry [44] as well blackcurrant [21] were reported to enhance serum lipids in high-fat diet fed mice, while our findings are supported by previous studies with lingonberry containing diets [21,35,45]. High-fat treatment normally results in increased circulating triglycerides in humans [46], but in mice their levels may stay unchanged or decrease [21,38,45,47–49], and the former was found also in the present study. These effects on triglycerides may result from increased clearance of triglycerides and/or reduced production of triglycerides in the liver [47–49]. Increased ALT activity in the serum, as was also shown in the current study, supports the former assumption likewise associated with the development of nonalcoholic fatty liver disorder [50].
Adipokines are cytokine-like hormones originally found to be produced by adipose tissue and to regulate energy metabolism and appetite [51,52]. Leptin is a prototype adipokine, the concentrations of which are closely related to the amount of adipose tissue and body mass index [53,54]. This is the first study showing reduced leptin levels during lingonberry supplementation of high-fat diet but the results are supported by studies using blueberry anthocyanins [38,44]. It is not clear if this effect is simply a consequence of the moderate weight gain restraining effect of lingonberry supplementation or whether it has mechanistic relevancy. Anyhow, reduced leptin level may be considered as a beneficial effect because leptin has pro-inflammatory effects and contributes to the development of co-morbidities of obesity [55]. In addition, an increasing trend in adiponectin levels was seen in mice on lingonberry supplemented high-fat diet. Since adiponectin has insulin sensitizing effects [4], this is a positive signal and motivates further studies.
Obesity is associated with low-grade inflammation, which contributes to the obesity-related metabolic diseases. Serum amyloid A (SAA) is an example of the biomarkers and effectors of obesity-related inflammation, and it is involved in the mechanisms of lipid metabolism, atherosclerosis and acute phase response besides inflammation [56,57]. In the present study, circulating SAA concentrations, as well as its expression in the liver, were substantially increased during high-fat diet while lingonberry supplementation prevented these changes in a statistically significant manner. In addition, lingonberry supplementation reduced the hepatic expression of two other pro-inflammatory factors, i.e. the chemokine CXCL-14 and the S100 calcium-binding protein A10. These data indicate that lingonberry supplementation indeed suppresses the obesity-related inflammatory response.
Based on the present data, it remains unclear, which factor(s) present in the lingonberry powder may have caused the beneficial effects found in the current study, and further studies are needed to reveal the active constituents. The effects of lingonberry supplementation on the weight gain were moderate while it significantly prevented many of the metabolic and inflammatory adverse effects induced by the high-fat diet. Therefore, it is possible that lingonberry supplementation in the high-fat containing diet has anti-inflammatory consequences and shifts endogenous responses towards metabolically healthier obesity. Lingonberries contain several polyphenolic compounds, which have anti-inflammatory potential such as anthocyanins, ellagitannins, flavonols, phenolic acids and proanthocyanidins [58], flavonols and proanthocyanidins as well as anthocyanins forming the largest groups among the lingonberry polyphenols [58–62].
Quercetin is abundantly present in lingonberries [63]. Quercetin has been reported to have anti-inflammatory effects in in vitro and in vivo models [64–66]. Moreover, quercetin has also been suggested to have anti-adiposity activity in vitro by activating the AMPK signal pathway in adipocytes [67] and in vivo by preventing high-fat diet induced obesity in mice [68]. Lingonberries are also a rich source of proanthocyanidins [60,69] and anthocyanins, particularly cyanidin-3-galactoside, cyanidin-3-arabinoside, and cyanidin-3-glucoside [70,71]. Proanthocyanidins have been reported to contribute to the reduced weight gain and hypolipidemic effects of berry-derived preparations in animal models of obesity [40,72,73] while purified anthocyanins from mulberry (M. australis P.) and cherry (Prunus avium L.) prevented obesogenic diet induced weight gain, oxidative stress and inflammation in mice [74,75]. Lingonberry contains also the stilbenoid compound resveratrol (together with its glycosylated derivative piceid), which is a strong antioxidant with anti-inflammatory properties [76–78]. We have recently shown that resveratrol inhibits the production of nitric oxide and pro-inflammatory cytokines in activated macrophages and suppresses inflammatory responses in vivo [79]. Resveratrol has also been beneficial in animal models of obesity [80–82], and in a clinical study resveratrol supplementation improved glycemic control in patients with type 2 diabetes [83].
In conclusion, the present results show that lingonberry supplementation significantly prevents high-fat diet induced metabolic and inflammatory changes in a murine model of obesity. Further studies are needed to reveal the detailed molecular mechanisms and the active constituents responsible for the observed beneficial effects. The results encourage evaluation of lingonberries as a part of healthy diet against obesity and its comorbidities.
Acknowledgments
We wish to acknowledge Meiju Kukkonen and Salla Hietakangas for excellent technical assistance.
Data Availability
All relevant data are within the paper.
Funding Statement
The study was financially supported by a grant from the European Regional Development Fund (ERDF). Kiantama Ltd, Suomussalmi, Finland provided the lingonberry powder. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.World Health Organization. Obesity and overweight. 2018. [Google Scholar]
- 2.Lee H, Lee IS, Choue R. Obesity, Inflammation and Diet. Pediatric Gastroenterology, Hepatology & Nutrition. 2013;16: 143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asghar A, Sheikh N. Role of immune cells in obesity induced low grade inflammation and insulin resistance. Cell Immunol. 2016;315: 18–26. [DOI] [PubMed] [Google Scholar]
- 4.Jung UJ, Choi M. Obesity and its metabolic complications: The role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. International Journal of Molecular Sciences. 2014;15: 6184–6223. 10.3390/ijms15046184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mraz M, Haluzik M. The role of adipose tissue immune cells in obesity and low-grade inflammation. J Endocrinol. 2014;222: 113–127. [DOI] [PubMed] [Google Scholar]
- 6.Dembinska-Kiec A, Mykkänen O, Kiec-Wilk B, Mykkänen H. Antioxidant phytochemicals against type 2 diabetes. Br J Nutr. 2008;99: ES109–ES117. 10.1017/S000711450896579X [DOI] [PubMed] [Google Scholar]
- 7.Pan M, Lai C, Ho C. Anti-inflammatory activity of natural dietary flavonoids. Food and Function. 2010;1: 15–31. 10.1039/c0fo00103a [DOI] [PubMed] [Google Scholar]
- 8.Williamson G. The role of polyphenols in modern nutrition. Nutr Bull. 2017;42: 226–235. 10.1111/nbu.12278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Szajdek A, Borowska EJ. Bioactive Compounds and Health-Promoting Properties of Berry Fruits: A Review. Plant Foods for Human Nutrition. 2008;63: 147–156. 10.1007/s11130-008-0097-5 [DOI] [PubMed] [Google Scholar]
- 10.Häkkinen SH, Kärenlampi SO, Heinonen IM, Mykkänen HM, Törronen AR. Content of the flavonols quercetin, myricetin, and kaempferol in 25 edible berries. J Agric Food Chem. 1999;47: 2274–2279. 10.1021/jf9811065 [DOI] [PubMed] [Google Scholar]
- 11.Knekt P, Kumpulainen J, Järvinen R, Rissanen H, Heliövaara M, Reunanen A, et al. Flavonoid intake and risk of chronic diseases. Am J Clin Nutr. 2002;76: 560–568. 10.1093/ajcn/76.3.560 [DOI] [PubMed] [Google Scholar]
- 12.Nile SH, Park SW. Edible berries: Bioactive components and their effect on human health. Nutrition. 2014;30: 134–144. 10.1016/j.nut.2013.04.007 [DOI] [PubMed] [Google Scholar]
- 13.Kolehmainen M, Mykkänen O, Kirjavainen PV, Leppänen T, Moilanen E, Adriaens M, et al. Bilberries reduce low-grade inflammation in individuals with features of metabolic syndrome. Molecular Nutrition and Food Research. 2012;56: 1501–1510. 10.1002/mnfr.201200195 [DOI] [PubMed] [Google Scholar]
- 14.Mursu J, Virtanen JK, Tuomainen TP, Nurmi T, Voutilainen S. Intake of fruit, berries, and vegetables and risk of type 2 diabetes in Finnish men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am J Clin Nutr. 2014;99: 328–333. 10.3945/ajcn.113.069641 [DOI] [PubMed] [Google Scholar]
- 15.Basu A, Rhone M, Lyons TJ. Berries: Emerging impact on cardiovascular health. Nutr Rev. 2010;68: 168–177. 10.1111/j.1753-4887.2010.00273.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drozdz P, Seziene V, Wojcik J, Pyrzynska K. Evaluation of Bioactive Compounds, Minerals and Antioxidant Activity of Lingonberry (Vaccinium vitis-idaea L.) Fruits. Molecules. 2017;23: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kowalska K, Olejnik A. Current evidence on the health-beneficial effects of berry fruits in the prevention and treatment of metabolic syndrome. Curr Opin Clin Nutr Metab Care. 2016;19: 446–452. 10.1097/MCO.0000000000000322 [DOI] [PubMed] [Google Scholar]
- 18.Mane C, Loonis M, Juhel C, Dufour C, Malien-Aubert C. Food grade lingonberry extract: Polyphenolic composition and in vivo protective effect against oxidative stress. J Agric Food Chem. 2011;59: 3330–3339. 10.1021/jf103965b [DOI] [PubMed] [Google Scholar]
- 19.Kivimäki AS, Siltari A, Ehlers PI, Korpela R, Vapaatalo H. Lingonberry juice negates the effects of a high salt diet on vascular function and low-grade inflammation. Journal of Functional Foods. 2014;7: 238–245. [Google Scholar]
- 20.Harbilas D, Martineau LC, Harris CS, Adeyiwola-Spoor DCA, Saleem A, Lambert J, et al. Evaluation of the antidiabetic potential of selected medicinal plant extracts from the Canadian boreal forest used to treat symptoms of diabetes: part II. Can J Physiol Pharmacol. 2009;87: 479–492. 10.1139/y09-029 [DOI] [PubMed] [Google Scholar]
- 21.Heyman L, Axling U, Blanco N, Sterner O, Holm C, Berger K, et al. Evaluation of beneficial metabolic effects of berries in high-fat fed C57BL/6J mice. Journal of Nutrition and Metabolism. 2014;2014: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heyman-Lindén L, Kotowska D, Sand E, Bjursell M, Plaza M, Turner C, et al. Lingonberries alter the gut microbiota and prevent low-grade inflammation in high-fat diet fed mice. Food & nutrition research. 2016;60: 29993–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Z, Zhou Q, Huangfu G, Wu Y, Zhang J. Anthocyanin extracts of lingonberry (Vaccinium vitis-idaea L.) attenuate serum lipids and cholesterol metabolism in HCD-induced hypercholesterolaemic male mice. International Journal of Food Science and Technology. 2018. [Google Scholar]
- 24.Anhê FF, Varin TV, Le Barz M, Pilon G, Dudonné S, Trottier J, et al. Arctic berry extracts target the gut–liver axis to alleviate metabolic endotoxaemia, insulin resistance and hepatic steatosis in diet-induced obese mice. Diabetologia. 2018;61: 919–931. 10.1007/s00125-017-4520-z [DOI] [PubMed] [Google Scholar]
- 25.Marungruang N, Kovalenko T, Osadchenko I, Voss U, Huang F, Burleigh S, et al. Lingonberries and their two separated fractions differently alter the gut microbiota, improve metabolic functions, reduce gut inflammatory properties, and improve brain function in ApoE−/− mice fed high-fat diet. Nutr Neurosci. 2018: 1–13. [DOI] [PubMed] [Google Scholar]
- 26.Bhullar KS, Rupasinghe HPV. Antioxidant and cytoprotective properties of partridgeberry polyphenols. Food Chem. 2015;168: 595–605. 10.1016/j.foodchem.2014.07.103 [DOI] [PubMed] [Google Scholar]
- 27.Zheng W, Wang SY. Oxygen radical absorbing capacity of phenolics in blueberries, cranberries, chokeberries, and lingonberries. J Agric Food Chem. 2003;51: 502–509. 10.1021/jf020728u [DOI] [PubMed] [Google Scholar]
- 28.Ehala S, Vaher M, Kaljurand M. Characterization of phenolic profiles of Northern European berries by capillary electrophoresis and determination of their antioxidant activity. J Agric Food Chem. 2005;53: 6484–6490. 10.1021/jf050397w [DOI] [PubMed] [Google Scholar]
- 29.Bere E. Wild berries: a good source of omega-3. Eur J Clin Nutr. 2007;61: 431–433. 10.1038/sj.ejcn.1602512 [DOI] [PubMed] [Google Scholar]
- 30.Piironen V, Toivo J, Lampi A-M. Natural Sources of Dietary Plant Sterols. Journal of Food Composition and Analysis. 2000;13: 619–624. [Google Scholar]
- 31.Szakiel A, Pączkowski C, Koivuniemi H, Huttunen S. Comparison of the triterpenoid content of berries and leaves of lingonberry Vaccinium vitis-idaea from Finland and Poland. J Agric Food Chem. 2012;60: 4994–5002. 10.1021/jf300375b [DOI] [PubMed] [Google Scholar]
- 32.Turtiainen M, Salo K, Saastamoinen O. Variations of yield and utilisation of bilberries (Vaccinium myrtillus L.) and cowberries (V. vitis-idaea L.) in Finland. Silva Fenn. 2011;45: 237–251. [Google Scholar]
- 33.Blaak EE, Antoine J, Benton D, Björck I, Bozzetto L, Brouns F, et al. Impact of postprandial glycaemia on health and prevention of disease: Postprandial glycaemia and health. Obesity Reviews. 2012;13: 923–984. 10.1111/j.1467-789X.2012.01011.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boucher J, Kleinridders A, Kahn CR. Insulin Receptor Signaling in Normal and Insulin-Resistant States. Cold Spring Harbor perspectives in biology. 2014;6: a009191 10.1101/cshperspect.a009191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anhê FF, Varin TV, Le Barz M, Pilon G, Dudonné S, Trottier J, et al. Arctic berry extracts target the gut–liver axis to alleviate metabolic endotoxaemia, insulin resistance and hepatic steatosis in diet-induced obese mice. Diabetologia. 2018;61: 919–931. 10.1007/s00125-017-4520-z [DOI] [PubMed] [Google Scholar]
- 36.Mykkänen OT, Huotari A, Herzig K, Dunlop TW, Mykkänen H, Kirjavainen PV. Wild blueberries (Vaccinium myrtillus) alleviate inflammation and hypertension associated with developing obesity in mice fed with a high-fat diet. PLoS ONE. 2014;9: e114790 10.1371/journal.pone.0114790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desai T, Roberts M, Bottoms L. Effects of Montmorency tart cherry supplementation on cardio-metabolic markers in metabolic syndrome participants: A pilot study. Journal of Functional Foods. 2019;57: 286–298. [Google Scholar]
- 38.Prior RL, E. Wilkes S, R. Rogers T, Khanal RC, Wu X, Howard LR. Purified blueberry anthocyanins and blueberry juice alter development of obesity in mice fed an obesogenic high-fat diet. J Agric Food Chem. 2010;58: 3970–3976. 10.1021/jf902852d [DOI] [PubMed] [Google Scholar]
- 39.Rasmussen SE, Frederiksen H, Krogholm KS, Poulsen L. Dietary proanthocyanidins: Occurrence, dietary intake, bioavailability, and protection against cardiovascular disease. Molecular Nutrition and Food Research. 2005;49: 159–174. 10.1002/mnfr.200400082 [DOI] [PubMed] [Google Scholar]
- 40.Bladé C, Arola L, Salvadó M. Hypolipidemic effects of proanthocyanidins and their underlying biochemical and molecular mechanisms. Molecular Nutrition and Food Research. 2010;54: 37–59. 10.1002/mnfr.200900476 [DOI] [PubMed] [Google Scholar]
- 41.Razavi S, Gholamin S, Eskandari A, Mohsenian N, Ghorbanihaghjo A, Delazar A, et al. Red grape seed extract improves lipid profiles and decreases oxidized low-density lipoprotein in patients with mild hyperlipidemia. Journal of Medicinal Food. 2013;16: 255–258. 10.1089/jmf.2012.2408 [DOI] [PubMed] [Google Scholar]
- 42.Wang DL, Xia M, Gao S, Li D, Zhang Y, Jin TR, et al. Cyanidin-3-O-ss-glucoside upregulates hepatic cholesterol 7a-hydroxylase expression and reduces hypercholesterolemia in mice. Molecular Nutrition and Food Research. 2012;56: 610–621. 10.1002/mnfr.201100659 [DOI] [PubMed] [Google Scholar]
- 43.AbuMweis SS, Jones PJH. Cholesterol-lowering effect of plant sterols. Curr Atheroscler Rep. 2008;10: 467–472. 10.1007/s11883-008-0073-4 [DOI] [PubMed] [Google Scholar]
- 44.Prior RL, Wu X, Gu L, Hager T, Hager A, Wilkes S, et al. Purified berry anthocyanins but not whole berries normalize lipid parameters in mice fed an obesogenic high fat diet. Molecular Nutrition and Food Research. 2009;53: 1406–1418. 10.1002/mnfr.200900026 [DOI] [PubMed] [Google Scholar]
- 45.Eid HM, Ouchfoun M, Brault A, Vallerand D, Musallam L, Arnason JT, et al. Lingonberry (Vaccinium vitis-idaea L.) exhibits antidiabetic activities in a mouse model of diet-induced obesity. Evidence-based Complementary and Alternative Medicine. 2014;2014: 645812–10. 10.1155/2014/645812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tonstad S, Després J. Treatment of lipid disorders in obesity. Expert Review of Cardiovascular Therapy. 2011;9: 1069–1080. 10.1586/erc.11.83 [DOI] [PubMed] [Google Scholar]
- 47.Biddinger SB, Almind K, Miyazaki M, Kokkotou E, Ntambi JM, Kahn CR. Effects of Diet and Genetic Background on Sterol Regulatory Element-Binding Protein-1c, Stearoyl-CoA Desaturase 1, and the Development of the Metabolic Syndrome. Diabetes. 2005;54: 1314–1323. 10.2337/diabetes.54.5.1314 [DOI] [PubMed] [Google Scholar]
- 48.Guo J, Jou W, Gavrilova O, Hall KD. Persistent diet-induced obesity in male C57BL/6 mice resulting from temporary obesigenic diets. PLoS ONE. 2009;4: e5370 10.1371/journal.pone.0005370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Podrini C, Cambridge EL, Lelliott CJ, Carragher DM, Estabel J, Gerdin A, et al. High-fat feeding rapidly induces obesity and lipid derangements in C57BL/6N mice. Mammalian Genome. 2013;24: 240–251. 10.1007/s00335-013-9456-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Smith BW, Adams LA. Nonalcoholic fatty liver disease and diabetes mellitus: Pathogenesis and treatment. Nature Reviews Endocrinology. 2011;7: 456–465. 10.1038/nrendo.2011.72 [DOI] [PubMed] [Google Scholar]
- 51.Shibata R, Ouchi N, Ohashi K, Murohara T. The role of adipokines in cardiovascular disease. J Cardiol. 2017;70: 329–334. 10.1016/j.jjcc.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 52.Scotece M, Conde J, Vuolteenaho K, Koskinen A, López V, Gómez-Reino J, et al. Adipokines as drug targets in joint and bone disease. Drug Discov Today. 2014;19: 241–258. 10.1016/j.drudis.2013.07.012 [DOI] [PubMed] [Google Scholar]
- 53.Pan H, Guo J, Su Z. Advances in understanding the interrelations between leptin resistance and obesity. Physiol Behav. 2014;130: 157–169. 10.1016/j.physbeh.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 54.Zhou Y, Rui L. Leptin signaling and leptin resistance. Frontiers of Medicine. 2013;7: 207–222. 10.1007/s11684-013-0263-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paz-Filho G, Mastronardi C, Franco CB, Wang KB, Wong M, Licinio J. Leptin: molecular mechanisms, systemic pro-inflammatory effects, and clinical implications. Arquivos Brasileiros de Endocrinologia & Metabologia. 2012;56: 597–607. [DOI] [PubMed] [Google Scholar]
- 56.Sack GH. Serum amyloid A—a review. Mol Med. 2018;24: 46 10.1186/s10020-018-0047-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sun L, Ye RD. Serum amyloid A1: Structure, function and gene polymorphism. Gene. 2016;583: 48–57. 10.1016/j.gene.2016.02.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Joseph SV, Edirisinghe I, Burton-Freeman BM. Berries: Anti-inflammatory effects in humans. J Agric Food Chem. 2014;62: 3886–3903. 10.1021/jf4044056 [DOI] [PubMed] [Google Scholar]
- 59.Bujor O, Ginies C, Popa VI, Dufour C. Phenolic compounds and antioxidant activity of lingonberry (Vaccinium vitis-idaea L.) leaf, stem and fruit at different harvest periods. Food Chemistry. 2018;252: 356–365. 10.1016/j.foodchem.2018.01.052 [DOI] [PubMed] [Google Scholar]
- 60.Heinonen M. Antioxidant activity and antimicrobial effect of berry phenolics—A Finnish perspective. Molecular Nutrition and Food Research. 2007;51: 684–691. 10.1002/mnfr.200700006 [DOI] [PubMed] [Google Scholar]
- 61.Ek S, Kartimo H, Mattila S, Tolonen A. Characterization of phenolic compounds from lingonberry (Vaccinium vitis-idaea). J Agric Food Chem. 2006;54: 9834–9842. 10.1021/jf0623687 [DOI] [PubMed] [Google Scholar]
- 62.Kähkönen MP, Hopia AI, Heinonen M. Berry phenolics and their antioxidant activity. J Agric Food Chem. 2001;49: 4076–4082. 10.1021/jf010152t [DOI] [PubMed] [Google Scholar]
- 63.Hajazimi E, Landberg R, Zamaratskaia G. Simultaneous determination of flavonols and phenolic acids by HPLC-CoulArray in berries common in the Nordic diet. LWT—Food Science and Technology. 2016;74: 128–134. [Google Scholar]
- 64.Nardi GM, De Farias Januário Adriana Graziele, Freire CG, Megiolaro F, Schneider K, Perazzoli MRA, et al. Anti-inflammatory activity of berry fruits in mice model of inflammation is based on oxidative stress modulation. Pharmacognosy Research. 2016;8: S42–S49. 10.4103/0974-8490.178642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hämäläinen M, Nieminen R, Vuorela P, Heinonen M, Moilanen E. Anti-inflammatory effects of flavonoids: Genistein, kaempferol, quercetin, and daidzein inhibit STAT-1 and NF-κB activations, whereas flavone, isorhamnetin, naringenin, and pelargonidin inhibit only NF-κB activation along with their inhibitory effect on iNOS expression and NO production in activated macrophages. Mediators Inflamm. 2007;2007: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yoon JS, Chae MK, Lee SY, Lee EJ. Anti-inflammatory effect of quercetin in a whole orbital tissue culture of Graves' orbitopathy. Br J Ophthalmol. 2012;96: 1117–1121. 10.1136/bjophthalmol-2012-301537 [DOI] [PubMed] [Google Scholar]
- 67.Ahn J, Lee H, Kim S, Park J, Ha T. The anti-obesity effect of quercetin is mediated by the AMPK and MAPK signaling pathways. Biochem Biophys Res Commun. 2008;373: 545–549. 10.1016/j.bbrc.2008.06.077 [DOI] [PubMed] [Google Scholar]
- 68.Jung CH, Cho I, Ahn J, Jeon T, Ha T. Quercetin Reduces High‐Fat Diet‐Induced Fat Accumulation in the Liver by Regulating Lipid Metabolism Genes. Phytotherapy Research. 2013;27: 139–143. 10.1002/ptr.4687 [DOI] [PubMed] [Google Scholar]
- 69.Grace MH, Esposito D, Dunlap KL, Lila MA. Comparative analysis of phenolic content and profile, antioxidant capacity, and anti-inflammatory bioactivity in wild Alaskan and commercial Vaccinium berries. J Agric Food Chem. 2014;62: 4007–4017. 10.1021/jf403810y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bakowska-Barczak AM, Marianchuk M, Kolodziejczyk P. Survey of bioactive components in Western Canadian berries. Can J Physiol Pharmacol. 2007;85: 1139–1152. 10.1139/Y07-102 [DOI] [PubMed] [Google Scholar]
- 71.Debnath SC, Sion M. Genetic Diversity, Antioxidant Activities, and Anthocyanin Contents in Lingonberry. International Journal of Fruit Science. 2009;9: 185–199. [Google Scholar]
- 72.Zheng S, Huang K, Zhao C, Xu W, Sheng Y, Luo Y, et al. Procyanidin attenuates weight gain and modifies the gut microbiota in high fat diet induced obese mice. Journal of Functional Foods. 2018;49: 362–368. [Google Scholar]
- 73.Garbacki N, Kinet M, Nusgens B, Desmecht D, Damas J. Proanthocyanidins, from Ribes nigrum leaves, reduce endothelial adhesion molecules ICAM-1 and VCAM-1. J Inflamm. 2005;2: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wu T, Yin J, Zhang G, Long H, Zheng X. Mulberry and cherry anthocyanin consumption prevents oxidative stress and inflammation in diet‐induced obese mice. Molecular Nutrition & Food Research. 2016;60: 687–694. [DOI] [PubMed] [Google Scholar]
- 75.Wu T, Qi X, Liu Y, Guo J, Zhu R, Chen W, et al. Dietary supplementation with purified mulberry (Morus australis Poir) anthocyanins suppresses body weight gain in high-fat diet fed C57BL/6 mice. Food Chemistry. 2013;141: 482–487. 10.1016/j.foodchem.2013.03.046 [DOI] [PubMed] [Google Scholar]
- 76.Rimando AM, Kalt W, Magee JB, Dewey J, Ballington JR. Resveratrol, pterostilbene, and piceatannol in Vaccinium berries. J Agric Food Chem. 2004;52: 4713–4719. 10.1021/jf040095e [DOI] [PubMed] [Google Scholar]
- 77.Wahab A, Gao K, Jia C, Zhang F, Tian G, Murtaza G, et al. Significance of resveratrol in clinical management of chronic diseases. Molecules. 2017;22: 1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Eräsalo H, Hämäläinen M, Leppänen T, Mäki-Opas I, Laavola M, Haavikko R, et al. Natural Stilbenoids Have Anti-Inflammatory Properties in Vivo and Down-Regulate the Production of Inflammatory Mediators NO, IL6, and MCP1 Possibly in a PI3K/Akt-Dependent Manner. J Nat Prod. 2018;81: 1131–1142. 10.1021/acs.jnatprod.7b00384 [DOI] [PubMed] [Google Scholar]
- 79.Laavola M, Nieminen R, Leppänen T, Eckerman C, Holmbom B, Moilanen E. Pinosylvin and Monomethylpinosylvin, Constituents of an Extract from the Knot of Pinus sylvestris, Reduce Inflammatory Gene Expression and Inflammatory Responses in Vivo. J Agric Food Chem. 2015;63: 3445–3453. 10.1021/jf504606m [DOI] [PubMed] [Google Scholar]
- 80.Ji G, Wang Y, Deng Y, Li X, Jiang Z. Resveratrol ameliorates hepatic steatosis and inflammation in methionine/choline-deficient diet-induced steatohepatitis through regulating autophagy. Lipids in Health and Disease. 2015;14: 134 10.1186/s12944-015-0139-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ohara K, Kusano K, Kitao S, Yanai T, Takata R, Kanauchi O. ε-Viniferin, a resveratrol dimer, prevents diet-induced obesity in mice. Biochem Biophys Res Commun. 2015;468: 877–882. 10.1016/j.bbrc.2015.11.047 [DOI] [PubMed] [Google Scholar]
- 82.Chang C, Lin K, Peng K, Day Y, Hung L. Resveratrol exerts anti-obesity effects in high-fat diet obese mice and displays differential dosage effects on cytotoxicity, differentiation, and lipolysis in 3T3-L1 cells. Endocr J. 2016;63: 169–178. 10.1507/endocrj.EJ15-0545 [DOI] [PubMed] [Google Scholar]
- 83.Bhatt JK, Thomas S, Nanjan MJ. Resveratrol supplementation improves glycemic control in type 2 diabetes mellitus. Nutr Res. 2012;32: 537–541. 10.1016/j.nutres.2012.06.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.