Abstract
Introduction:
Research shows that loss of control (LOC) eating impacts weight outcomes following bariatric surgery, but mechanisms explaining the development and/or maintenance of post-surgical LOC eating remain unclear. Ecological momentary assessment (EMA) research among eating disorder populations has demonstrated prospective relationships between negative affect (NA) and LOC eating; however, this momentary effect has not been examined among bariatric surgery patients. Thus, this study used EMA data to examine momentary relationships between NA and LOC eating among pre- and post-bariatric surgery patients.
Methods:
Fourteen pre- and 17 post-RYGB patients completed two weeks of EMA data collection. Participants responded to seven signals daily wherein they rated their mood and severity of LOC eating.
Results:
Higher momentary NA predicted more severe LOC eating for all participants. Group had a moderating effect, demonstrating that the association between NA and LOC eating was stronger among the post-surgery group. Percent total body weight loss (%TBWL) had a moderating effect within the post-surgery group, demonstrating that the relationship between NA and LOC eating was stronger for those who experienced less weight loss. Finally, between-subjects analyses revealed that, for individuals with lower %TBWL, lower overall NA and higher overall positive affect (PA) were related to greater LOC eating.
Conclusion:
This research demonstrates that affect influences the effect of LOC eating on weight loss following bariatric surgery. While further work is needed to extend these preliminary findings, this research suggests that affective experience might become an important target in the assessment and treatment of LOC eating among bariatric patients.
Keywords: bariatric surgery, ecological momentary assessment (EMA), loss of control (LOC) eating, negative affect, weight loss
While bariatric surgery often results in substantial weight loss, a subset of patients experience poor weight loss or weight regain following surgery [1–3]. One potential explanatory mechanism for poor weight-related outcomes after surgery is loss of control (LOC) eating and, consequently, the investigation into LOC eating as a possible psychosocial predictor of poor weight outcomes has grown rapidly in the past several years. While LOC eating is a concern among patients prior to bariatric surgery, with recent pre-surgical estimates ranging from 6% to 34%, incidence of LOC eating generally decreases following surgery [4]. However, research suggests that patients who exhibit post-surgical LOC eating are at an increased risk for poor weight loss outcomes in both the short- and long-term [5,6].
Several time course patterns of post-surgical LOC eating have been identified in recent literature. Pre-surgical LOC eating has been shown to persist for some individuals following surgery, while others experience post-surgical resolution of LOC eating over time [7–9]. Additionally, LOC eating may develop for the first time after surgery, posing not only a risk for poor weight-related outcomes but also for additional psychological impairment [10]. Despite these recent observations, the mechanisms behind patterns of post-surgical LOC eating are unknown. In as much as targeting LOC eating is important in improving weight outcomes following bariatric surgery, additional research is needed to elucidate precipitants of LOC eating and whether there are differences in these precipitants before and after surgery.
Affect is one contributor to LOC eating that has gained substantial support in the eating disorder and obesity literature. Several theories posit that negative affect (NA) is central to the development and maintenance of maladaptive eating behaviors (see Haedt-Matt & Keel, 2011 for a review) [11]. Consistent with these theories, studies using ecological momentary assessment (EMA) [12], or the collection of data as it occurs throughout the day in an individual’s natural environment, have shown that NA increases immediately prior to episodes of LOC eating among samples with eating disorders [11] and obesity [13]. However, little is known about the role of NA in LOC eating among bariatric surgery patients and whether this momentary relationship might help explain why some individuals experience poor weight loss outcomes following surgery.
The current study sought to test the momentary relationship between NA and LOC eating among bariatric surgery patients using EMA. The specific aims were: 1) to examine differences in the momentary relationships between NA and LOC eating among pre- and post-bariatric surgery patients, and 2) to determine whether weight loss moderates this relationship after surgery. It was hypothesized that higher NA would lead to subsequent greater LOC eating and that this relationship would be particularly strong for those individuals with lower percent weight loss following surgery.
Method
Participants
A total of 31 patients were included in this study. The sample was 90.0% female, 95.0% Caucasian, and had an average age of 41.16 years (SD = 9.92). Participants were categorized into one of two groups: individuals who were seeking RYGB surgery (“pre-surgery”; n = 14) or individuals who had already received RYGB surgery (“post-surgery”; n = 17). The average Body Mass Index (BMI) was 44.70 kg/m2 (SD = 6.62) for the pre-surgery group and 27.06 kg/m2 (SD = 4.03) for the post-surgery group. The average length of time since surgery for the post-surgery group was 23.54 months (SD = 4.75). There were no significant differences between groups on age, gender, or ethnicity (p’s > .05).
Procedure
Patients were recruited from a bariatric surgery clinic in the Midwest United States. This research was approved by the institutional review boards of two affiliated universities. At the beginning of the study, participants presented to the research laboratory to provide informed consent, height and weight data, and complete a series of baseline questionnaires. Participants were then asked to complete two weeks of the EMA protocol on a small personal digital computer. The daily EMA protocol consisted of six semi-random signals and one end-of-day signal. Once signaled, participants were prompted to respond to questions regarding their affect and eating behavior.
Measures
Height and weight.
Research assistants measured height and weight in the laboratory at the onset of the study. Post-surgical patients provided self-report of their pre-surgical weight. Percent total body weight loss (%TBWL) for the post-surgery group was calculated as [(pre-surgical weight) – (post-surgical weight) / pre-surgical weight] x 100.
Affect.
During the EMA protocol, participants were asked to rate their current affect from 1 “Not at all” to 5 “Extremely.” Affect items were selected from the International Positive and Negative Affect Schedule – Short Form (I-PANAS-SF) [14]. Negative affect (NA) items included afraid, distressed, jittery, scared, and upset. Positive affect (PA) items included determined, enthused, excited, inspired, and interested. The average of all five negative and positive affect items was taken for each signal to create a composite measure of NA and PA, respectively.
Loss of control (LOC) eating.
After indicating whether they had eaten since the last signal in the EMA protocol, participants were asked to respond to the item “Did you experience a sense of loss of control during this eating episode?” Participants provided a score from 1 “Not at all” to 5 “Extremely.”
Data Analysis
A series of generalized estimating equations (GEEs) with a gamma log link response function were conducted in SPSS version 25.0 to assess the hypothesized momentary relationships [15]. GEE models are considered the most appropriate analysis for repeated measures data that are not normally distributed [16]. Given that the dependent variable (LOC eating) was positively skewed, the gamma log link response function effectively accounted for the non-normal distribution when calculating model effects.
For each analysis, affect scores were lagged so that NA at time 1 (t – 1) could predict LOC eating at time 2 (t). The NA scores were then grand-mean and person-mean centered to disaggregate between-subject and within-subject effects [17,18]. Between-subject effects describe differences between individuals in NA that are associated with LOC eating, while within-subject effects describe differences in NA across varying situations that are associated with LOC eating. To assess between-subject effects (i.e., to grand-mean center), the average score for NA across all individuals in the study was subtracted from each participant’s aggregate score for NA (“NA-between”). To assess within-subject effects (i.e., to person-mean center), each individual’s aggregated NA score was subtracted from the signal level NA score (“NA-within”).
For the first analysis examining group as a moderator of the effect between NA and LOC eating, the NA-between, NA-within, and group variables were entered as main effects into the GEE model. Interaction terms for NA-between and group and NA-within and group were also entered into the model. For the second analysis examining %TBWL as a moderator of the NA-LOC eating relationship among post-surgery participants, the NA-between, NA-within, and %TBWL variables were entered as main effects into the GEE model. Time since surgery was grand-mean centered and entered as a covariate into the model. Interaction terms for NA-between and %TBWL and NA-within and %TBWL were also entered into the model.
Results
EMA Adherence and Frequency of LOC Eating
Adherence to the EMA protocol was calculated for each participant by dividing the number of completed random signals from the total number of signals received. The average EMA adherence rate was 88.87% for the pre-surgery group and 91.85% for the post-surgery group. In order to test the hypotheses, all available LOC eating ratings following an episode of eating were utilized, which resulted in 76 of the 217 total signals (35%) being included in analyses. Of those 76 signals, 43 came from the pre-surgery group (56.58%) and 33 came from the post-surgery group (43.42%). Further, LOC eating was reported by 11 pre-surgery and 9 post-surgery participants.
Group as a Moderator of the Effect between NA and LOC Eating
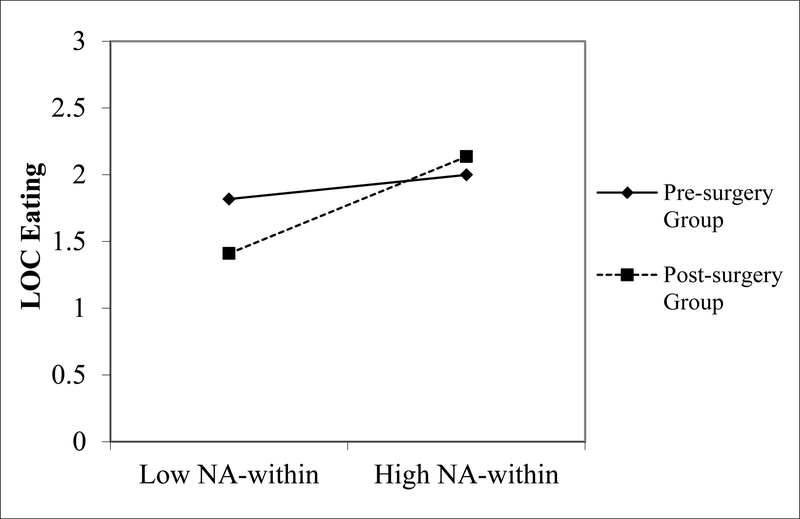
Results of the GEE model examining group as a moderator of the effect between NA and LOC eating failed to find significant effects for group, NA-between, and the NA-between by group interaction (Table 1). However, the main effect for NA-within was significant (p = .050), indicating that higher momentary NA scores predicted greater LOC eating ratings at the next signal. The interaction term between group (with the pre-surgery group as the reference group) and the NA-within variable was also significant (p < .001), indicating the relationship between momentary NA and subsequent LOC eating was stronger among post-surgery participants (Figure 1).
Table 1.
Results of a Model Examining Group as a Moderator of the Effect between Negative Affect and Loss of Control Eating.
| B | SE | p | 95% C.I. (upper, lower) | |
|---|---|---|---|---|
| Group | −0.09 | 0.15 | .536 | −0.39, 0.20 |
| NA-between | −0.03 | 0.08 | .664 | −0.19, 0.12 |
| NA-within | 0.06 | 0.03 | .050* | 0.00, 0.12 |
| Group x NA-between | 0.08 | 0.18 | .675 | −0.28, 0.44 |
| Group x NA-within | 0.16 | 0.04 | < .001*** | 0.08, 0.25 |
Note:
p ≤ .05;
p < .001.
“NA” denotes “negative affect”.
Figure 1.
A graphical breakdown of the interaction effect between momentary negative affect (NA)-within and loss of control (LOC) eating revealed that the prospective relationship was stronger for the post-surgery group when compared to the pre-surgery group.
%TBWL as a Moderator of the Effect between NA and LOC Eating for Post-Surgery Participants
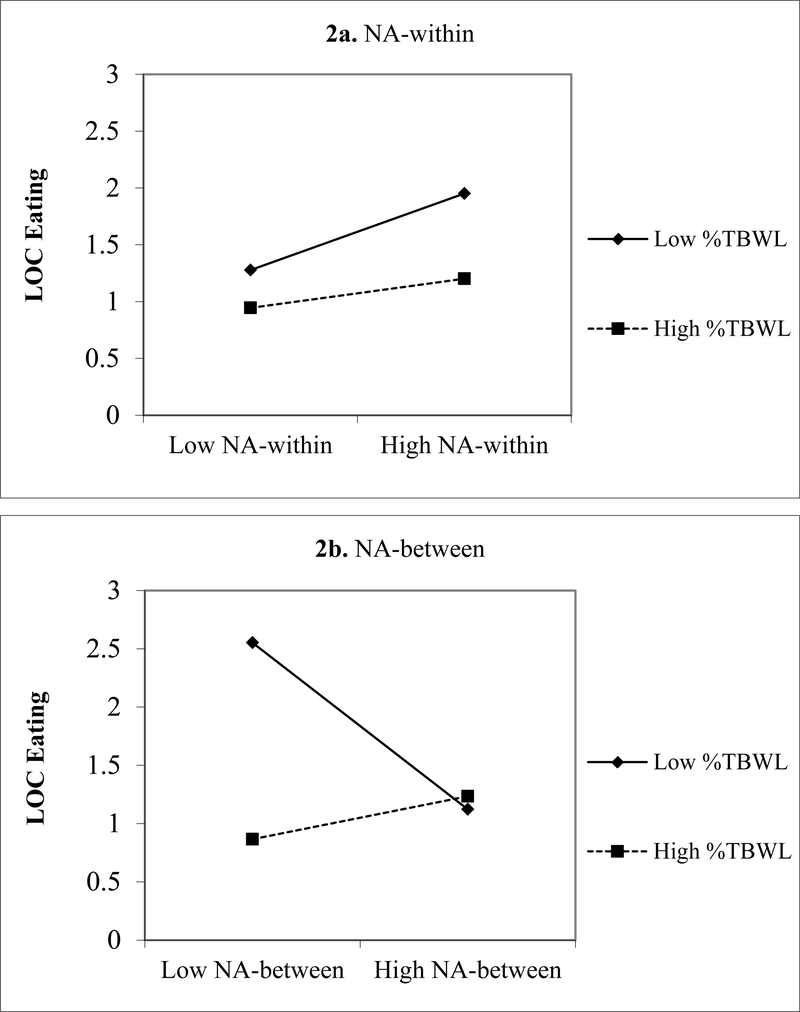
Average %TBWL for the nine post-surgery patients included in analyses was 32.79% (SD = 7.29). Results of the GEE examining %TBWL as a moderator of the relationship between NA and LOC eating among post-surgery participants failed to find significant effects for time since surgery, NA-between, and %TBWL (Table 2). However, NA-within emerged as a significant main effect (p < .001), once again indicating that higher momentary NA scores predicted greater subsequent LOC eating. The interaction terms for NA-within by %TBWL and NA-between by %TBWL emerged as significant (p = .021 and p = .009, respectively). A breakdown of the NA-within by %TBWL interaction revealed that the relationship between momentary NA and LOC eating was strengthened for low levels of %TBWL (Figure 2). However, a breakdown of the NA-between by %TBWL interaction revealed that for individuals with lower %TBWL, lower overall NA was related to reported greater LOC eating over the EMA protocol (Figure 2).
Table 2.
Results of a Model Examining Percent Total Body Weight Loss as a Moderator of the Relationship between Negative Affect and Loss of Control Eating among Post-Surgery Participants.
| B | SE | p | 95% C.I. (upper, lower) | |
|---|---|---|---|---|
| Time since surgery | 0.02 | 0.02 | .376 | −0.02, 0.05 |
| NA-between | −0.16 | 0.19 | .393 | −0.53, 0.21 |
| NA-within | 0.16 | 0.02 | < .001*** | 0.11, 0.20 |
| %TBWL | −0.03 | 0.01 | .066 | −0.05, 0.00 |
| NA-between x %TBWL | 0.06 | 0.02 | .009** | 0.01, 0.10 |
| NA-within x %TBWL | −0.01 | 0.00 | .021* | −0.01, 0.00 |
Note:
p < .05;
p < .01;
p < .001.
“NA” denotes “negative affect.” “%TBWL” denotes “percent total body weight loss.”
Figure 2.
A graphical breakdown of the within-subjects negative affect (NA) by percent total body weight loss (%TBWL) interaction revealed that the relationship between momentary NA and loss of control (LOC) eating was stronger at low levels of weight loss compared to high levels of weight loss (Figure 2a). However, the graphical breakdown for the between-subjects NA by %TBWL interaction revealed that, for individuals with lower %TBWL, lower overall NA was related to greater LOC eating (e.g., as it occurred over the entirety of the EMA protocol) (Figure 2b).
Post-hoc Analysis: Positive Affect
The significant effect demonstrating that lower NA-between scores predicted greater LOC eating for individuals with low, but not high, %TBWL was counterintuitive. While it is possible that this effect was spurious, particularly in light of the smaller cross-sectional sample used for analyses, we chose to conduct the same analysis using positive affect (PA) in an attempt to explore whether this affective valance might clarify the direction of the counterintuitive relationship. Therefore, a parallel post-hoc GEE model was tested using between- and within-person PA components and their interactions with %TBWL as predictors of LOC eating, controlling for time since surgery.
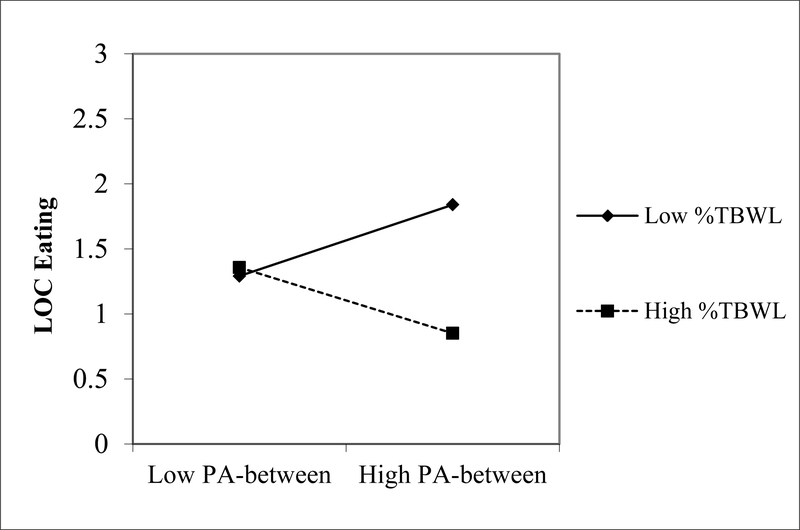
Results failed to demonstrate significant effects for time since surgery, PA-between, PA-within, %TBWL, and the interaction between PA-within and %TBWL (Table 3). However, the interaction between PA-between and %TBWL emerged as significant (p = .043). A breakdown of this effect revealed that among individuals with lower %TBWL, higher overall PA was related to greater LOC eating, whereas for individuals with higher %TBWL, higher overall PA was related to lower LOC eating over the EMA protocol (Figure 3).
Table 3.
Results of a Model Examining Percent Total Body Weight Loss as a Moderator of the Relationship between Positive Affect and Loss of Control Eating among Post-Surgery Participants.
| B | SE | p | 95% C.I. (upper, lower) | |
|---|---|---|---|---|
| Time since surgery | 0.01 | 0.04 | .836 | −0.07, 0.08 |
| PA-between | −0.01 | 0.05 | .907 | −0.10, 0.09 |
| PA-within | 0.00 | 0.04 | .933 | −0.07, 0.08 |
| %TBWL | −0.01 | 0.02 | .621 | −0.05, 0.03 |
| PA-between x %TBWL | −0.01 | 0.00 | .043* | −0.01, 0.00 |
| PA-within x %TBWL | 0.00 | 0.00 | .994 | −0.01, 0.01 |
Note:
p < .05.
“PA” denotes “positive affect.” “%TBWL” denotes “percent total body weight loss.”
Figure 3.
A graphical breakdown of the between-subjects positive affect (PA) by percent total body weight loss (%TBWL) interaction revealed that, among individuals with lower %TBWL, higher overall PA was related to greater LOC eating. Alternatively, for individuals with higher %TBWL, higher overall PA was related to lower LOC eating.
Discussion
This study examined momentary relationships between NA and LOC eating before and after bariatric surgery. Results demonstrated that high momentary NA predicted more severe subsequent LOC eating for all participants. This finding is consistent with previous research on eating disorders and obesity [11,13] and further suggests that intense affect occurring on a moment-to-moment basis in the natural environment may serve as an important precipitant of LOC eating among bariatric surgery patients.
Additionally, our results provide novel evidence that the relationship between momentary NA and LOC eating is stronger among post-surgery patients. While this finding should be considered preliminary due to the limited post-surgery sample size, it reveals a potentially important factor that may help explain why some patients are prone to experiencing LOC eating after surgery. Indeed, it has been suggested that difficulty with regulating emotions following surgery, particularly during stressful situations, is linked with the engagement in maladaptive emotion regulation behaviors [19]. Given the strict dietary regimens needed following bariatric surgery, it is logical to conclude that NA resulting from pressures to adhere to post-surgical guidelines may prompt lapses in dietary restraint [7,20]. While our findings are consistent with this hypothesis, demonstrating that intense momentary NA occurring after surgery may explain why some individuals are more likely to engage in LOC eating, future research utilizing larger sample sizes of patients who report more frequent LOC eating is warranted to further substantiate these results.
We also found several interesting moderating effects for %TBWL. Regarding within-person effects, the relationship between momentary NA and LOC eating was stronger at low, but not high, levels of weight loss among post-surgery patients. This suggests that NA may be a particularly salient predictor of LOC eating among individuals who have experienced poor weight loss outcomes following surgery. Examining this relationship longitudinally through future research in order to further elucidate the temporal precedence of weight loss, NA, and LOC eating following surgery would be beneficial.
In contrast, between-person effects indicated that, for individuals with lower %TBWL, lower overall NA and higher overall PA were related to greater LOC eating. These findings suggest that it is important to consider individual differences in both affect intensity and valence to better understand post-surgical LOC eating, particularly given that positive and negative emotions have distinct influences on eating behavior (for a review see Macht, 2008) [21]. While directionality cannot be inferred from between-person effects, one explanation for this effect may be that individuals who engage in more LOC eating experience greater reinforcing effects (i.e., increased PA and decreased NA) from such behavior, which may reflect heightened food-related reward responsivity [22]. Though such reinforcement may improve overall affect, this process can nevertheless serve to maintain LOC eating over time, which may ultimately impede weight loss. Another possible explanation for this effect involves eating expectancies, as affect can activate particular beliefs about reinforcement from eating (i.e., eating will increase positive or decrease negative emotional states) [23]. It may be the case that individuals with higher overall PA may have stronger positive affect-related eating expectancies (i.e., the expectancy that food is pleasurable and useful as a reward), which in turn could promote increased LOC eating. While further research is necessary to elucidate the direction of these between-person associations, examining other relevant factors (e.g., reward functioning and cognitive eating expectancies) that could influence these affect and LOC eating relationships among bariatric surgery patients could also advance the literature.
Several limitations of the current research should be noted. First, the study utilized a small sample of bariatric surgery patients. This, combined with the number of LOC eating observations and severity ratings available in the data (i.e., only 20 of the original 31 participants reported LOC eating ratings that could be used in analyses), resulted in restricted power in statistical analyses and may reflect the broader issue of collecting self-reported rather than objective measures of eating behavior. Due to these limitations, the findings presented in this paper are considered preliminary and future research should seek to replicate these findings among larger samples of bariatric surgery patients. Second, the sample was comprised mostly of participants who identified themselves as female and White. This may limit the generalizability of findings to other bariatric surgery patients and highlights an important need to incorporate more diverse samples in future research on this topic. Finally, this research used a cross-sectional design, thus limiting the ability to make longitudinal inferences regarding the relationship between affective experiences and LOC eating. Future research could further examine these relationships by following a single cohort of bariatric surgery patients to examine possible changes in the associations between affect and LOC eating from pre- to post-surgery.
In conclusion, this research provides preliminary evidence that affect intensity may serve as an important mechanism that influences LOC eating’s impact on weight loss following bariatric surgery. While further work is needed to replicate and extend these findings, the current research suggests that affective experience might become an important target in the assessment and treatment of LOC eating among bariatric patients.
Acknowledgments
Funding: This study was supported by grants R03-AA-019573 and R01-AA-022336 from the National Institute on Alcohol Abuse and Alcoholism and grant T32-MH-082761 from the National Institute of Mental Health.
Footnotes
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Melton GB, Steele KE, Schweitzer MA, Lidor AO, Magnuson TH. Suboptimal weight loss after gastric bypass surgery: Correlation of demographics, comorbidities, and insurance status with outcomes. J Gastrointest Surg. 2008;12:250–5. [DOI] [PubMed] [Google Scholar]
- 2.Hsu LKG, Benotti PN, Dwyer J, Roberts SB, Saltzman E, Shikora S, et al. Nonsurgical factors that influence the outcome of bariatric surgery: A review. Psychosom Med. 1998;60:338–46. [DOI] [PubMed] [Google Scholar]
- 3.Magro DO, Geloneze B, Delfini R, Pareja BC, Callejas F, Pareja JC. Long-term weight regain after gastric bypass: A 5-year prospective study. Obes Surg. 2008;18:648–51. [DOI] [PubMed] [Google Scholar]
- 4.Williams-Kerver GA, Steffen KJ, Mitchell JE. Eating pathology after bariatric surgery: An updated review of the recent literature. Curr Psychiatry Rep [Internet]. Springer US; 2019. [cited 2019 Nov 22];21:86 Available from: http://link.springer.com/10.1007/s11920-019-1071-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meany G, Conceição E, Mitchell JE. Binge eating, binge eating disorder and loss of control eating: Effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev. 2014;22:87–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wimmelmann CL, Dela F, Mortensen EL. Psychological predictors of weight loss after bariatric surgery: A review of the recent research. Obes Res Clin Pract. 2014;8:e299–313. [DOI] [PubMed] [Google Scholar]
- 7.Devlin MJ, King WC, Kalarchian MA, Hinerman A, Marcus MD, Yanovski SZ, et al. Eating pathology and associations with long-term changes in weight and quality of life in the longitudinal assessment of bariatric surgery study. Int J Eat Disord. 2018;51:1322–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith KE, Orcutt M, Steffen KJ, Crosby RD, Cao L, Garcia L, et al. Loss of control eating and binge eating in the 7 years following bariatric surgery. Obes Surg. 2019;29:1773–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conceição EM, Mitchell JE, Pinto-Bastos A, Arrojado F, Brandão I, Machado PPP. Stability of problematic eating behaviors and weight loss trajectories after bariatric surgery: A longitudinal observational study. Surg Obes Relat Dis. 2017;13:1063–70. [DOI] [PubMed] [Google Scholar]
- 10.Conceição EM, Orcutt M, Mitchell J, Engel S, LaHaise K, Jorgensen M, et al. Eating disorders after bariatric surgery: A case series. Int J Eat Disord. 2013;46:274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychol Bull. 2011;137:660–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stone AA, Hufford MR, Shiffman S. Ecological Momentary Assessment. Annu Rev Clin Psychol. 2008;4:1–32. [DOI] [PubMed] [Google Scholar]
- 13.Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, et al. Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Int J Eat Disord [Internet]. John Wiley & Sons, Ltd; 2015. [cited 2019 Jan 8];48:641–53. Available from: http://doi.wiley.com/10.1002/eat.22401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson ER. Development and validation of an internationally reliable short-form of the Positive and Negative Affect Schedule (PANAS). J Cross Cult Psychol. 2007;38:227–42. [Google Scholar]
- 15.IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.; 2017. [Google Scholar]
- 16.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 17.Curran PJ, Bauer DJ. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu Rev Psychol [Internet]. 2011. [cited 2020 Jan 21];62:583–619. Available from: http://www.annualreviews.org/doi/10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 19.Sarwer DB, Allison KC, Wadden TA, Ashare R, Spitzer JC, McCuen-Wurst C, et al. Psychopathology, disordered eating, and impulsivity as predictors of outcomes of bariatric surgery. Surg Obes Relat Dis. 2019;15:650–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polivy J, Herman CP. Dieting and binging: A causal analysis. Am Psychol. 1985;40:193–201. [DOI] [PubMed] [Google Scholar]
- 21.Macht M How emotions affect eating: A five-way model. Appetite. 2008;50:1–11. [DOI] [PubMed] [Google Scholar]
- 22.Wierenga CE, Ely A, Bischoff-Grethe A, Bailer UF, Simmons AN, Kaye WH. Are Extremes of Consumption in Eating Disorders Related to an Altered Balance between Reward and Inhibition? Front Behav Neurosci. 2014;8:410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hohlstein LA, Smith GT, Atlas JG. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychol Assess. 1998;10:49–58. [Google Scholar]