Abstract
Objective:
To examine the association between fraternity/sorority membership and athlete status with tobacco use by tobacco product type.
Participants:
Undergraduate college students who participated in the Spring 2017 National College Health Assessment-II Survey (n=47,821).
Methods:
Prevalence of current (past-30 day) cigarette smoking, waterpipe tobacco smoking (WTS), and e-cigarette (ECIG) use was examined. Logistic regressions examined associations between fraternity/sorority membership and participation in collegiate athletics with tobacco use.
Results:
Fraternity/sorority members had the highest current use rates for cigarettes, waterpipe tobacco, and ECIGs and were nearly twice as likely to report cigarette smoking, WTS, and ECIG use relative to non-fraternity/sorority members. Relative to non-varsity athletes, varsity athletes were less likely to report cigarette smoking and WTS, but not ECIG use.
Conclusions:
Fraternity/sorority members appear to be at risk for use of multiple tobacco products. Varsity athlete status may be protective for some tobacco products, but does not appear no for ECIG use. ECIGs may appeal to groups typically at low risk for other tobacco products.
Keywords: College, fraternity and sorority members, athletes, tobacco, electronic cigarettes
Introduction
More than 50 years after the first Surgeon General Report on the health impacts of cigarette smoking, nearly half a million deaths are attributed to cigarette smoking in the United States annually.1 While cigarette smoking rates have declined steeply since the Surgeon General Report in 1964, alternative tobacco products have gained popularity in the past approximately 15 years. Waterpipe tobacco smoking (WTS; also known as hookah, shisha, narghile, or argileh) increased in popularity in the United States (U.S.) during the early to mid-2000s, particularly among young adults and college students and is still used today by many young adults and college students.2-8 Typical WTS involves the use of an ignited charcoal to heat moist, sweetened, and flavored tobacco (known as mu’assel) to generate smoke for user inhalation. The smoke is inhaled via a hose and mouthpiece after the smoke has passed through water contained within the body of the waterpipe. Although the prevalence of WTS has decreased in recent years, during its peak years WTS was more common than cigarette smoking among young adults and college students.9 This popularity may have been fueled by common misperceptions of the harms associated with WTS with many young adults and college students perceiving WTS to be associated with fewer health risks compared to cigarette smoking.10-12 However, research has demonstrated that this form of tobacco smoking still exposes users to many of the same toxicants found in cigarette smoke such as carbon monoxide, volatile aldehydes, and nicotine, many in greater amounts than found in the smoke from a cigarettee.g.,13-15 as well as many of the same health risks as cigarette smoking.16
More recently, electronic cigarettes (ECIGs) have emerged as an alternative tobacco product that has gained popularity, particularly among youth and young adults.8,17 ECIGs are a class of products that use a heater to aerosolize a liquid that usually contains nicotine, propylene glycol, vegetable glycerin, and chemical flavorants for user inhalation.18 While ECIGs were introduced to the market in the U.S. in 2006, ECIG use prevalence increased sharply in 2011, a trend that has continued through the present.8,19,20 Similar to when WTS was increasing in popularity, research examining ECIG perceptions demonstrate that many perceive ECIGs to be a safer alternative to cigarettes.e.g.,21-24 However, unlike with WTS, the scientific community has not come to consensus regarding the health risks associated with ECIG use. As such, some see ECIGs as a potential reduced harm alternative to cigarette smoking and others focus on the potential health risks of ECIGs. However, most agree that youth and young adult ECIG use should be prevented, especially given the evidence that ECIG use may increase the risk of cigarette smoking among youth and young adults.25-28
Though cigarette smoking continues to appeal to some youth and young adults, the increasing diversity of tobacco products available in today’s marketplace has resulted in greater tobacco product options for individuals who are not drawn to cigarette smoking. More available tobacco product options may increase the risk of tobacco use among youth and young adults, including college students. Because different tobacco products may be associated with different harm perceptions and appeals due to different product characteristics and trends, there are likely subgroups of college students that are at increased risk for use of specific tobacco products. Similarly, some groups may be at a decreased risk for use of certain tobacco products. For example, fraternity and sorority members have been shown to be at increased risk for many forms of substance use, including tobacco use29-31 and may represent a group at increased risk for many tobacco products. Conversely, some college athletes may be at lower risk for cigarette smoking,32-35 but may be at greater risk for alternative tobacco products such as WTS.36 With the recent increase in popularity of ECIGs among youth and young adults, there is a need to examine population subgroup and tobacco product specific risk.
To identify at-risk populations and develop tobacco prevention messages that are tailored to specific population subgroups, data are needed on the specific tobacco products that likely appeal to and are more prevalent within subgroups of the population. There has been limited research conducted recently examining the association between college fraternity/sorority member status or athlete status and tobacco use. Additionally, this association has not been examined extensively during the time when ECIGs have become the most popular tobacco product among young people. There is a need to examine whether patterns of tobacco use have changed with regard to cigarette smoking and WTS among college fraternity/sorority members and athletes as well as whether these patterns are consistent for ECIG use. Examining the associations between athlete or fraternity/sorority membership status and tobacco use by specific tobacco product type could inform prevention efforts. Therefore, the purpose of this study was to examine the association between fraternity/sorority membership and athlete status with cigarette smoking, WTS, and ECIG use among U.S. undergraduate college students.
Methods
Design, setting, and procedures
The National College Health Assessment-II (NCHA-II) is a national survey of U.S. college students conducted by the American College Health Association (ACHA). The NCHA-II samples over 90,000 college students from public and private colleges and universities, is conducted bi-annually in the spring and fall semesters, and examines numerous health behaviors and outcomes as well as demographic characteristics. Universities are included from different U.S. geographic regions (South, Northeast, Midwest, and West). For the current study, we analyzed data from participants who completed the Spring 2017 NCHA-II survey. From all participants who completed the Spring 2017 NCHA-II survey (N=63,497), we included data from participants who reported being an undergraduate student and excluded graduate students and those not seeking a degree. The sample size for the current study was 47,821.
Measures
Sociodemographic data
Self-reported age, gender, race, and ethnicity were examined and included in models as covariates.
Cigarette, waterpipe, and ECIG use
The NCHA-II assesses many forms of substance use by asking participants to respond to the question: “Within the last 30 days, on how many days did you use: (Please mark the appropriate column for each row).” Response options include Never used; Have used, but not in the last 30 days; 1–2 days; 3–5 days; 6–9 days; 10–19 days; 20–29 days; and Used daily. For the current study, responses to “cigarettes”, “e-cigarettes”, and “tobacco from a water pipe (hookah)” were examined. For each product, participants who reported use on 1 or more of the past 30 days were considered current users.
Fraternity/Sorority membership and organized sports participation
The NCHA-II assesses fraternity/sorority membership by asking participants: “Are you a member of a social fraternity or sorority? (e.g., National Interfraternity Conference, National Panhellenic Conference, National Pan-Hellenic Council, National Association of Latino Fraternal Organizations). Participants were considered fraternity/sorority members if they responded “yes” to this question. College athlete status was assessed based on responses to the question: “Within the last 12 months, have you participated in organized college athletics at any of the following levels? (Please mark the appropriate column for each row)”. Participants could respond yes or no to participating in “Varsity”, “Club Sports”, or “Intramurals” athletics.
Statistical analysis
Descriptive statistics were examined for demographic characteristics, tobacco use, fraternity/sorority membership, and participation in intramural, club, and varsity sports. Prevalence of current cigarette smoking, WTS, and ECIG use were examined in the entire sample as well as among sample subgroups. Chi-square tests were used to examine if current use of cigarettes, waterpipe, or ECIGs was associated with demographic characteristics, fraternity/sorority member status (i.e., fraternity/sorority members vs. non-fraternity/sorority members), and athlete status (i.e., athletes vs. non-athletes). Independent adjusted multivariate logistic regressions were conducted to examine the odds of current cigarette smoking, WTS, and ECIG use based on fraternity/sorority membership and athlete status. Adjusted models included age, gender, race, and ethnicity as covariates. Membership in a fraternity/sorority as well as participation in varsity, club, or intramural athletics was not mutually exclusive. Analyses were conducted in SPSS 25 and an alpha level of .05 was used to determine statistical significance. Cases were included in analyses if they had complete data for each tobacco use item assessed (i.e., cigarette, waterpipe, ECIG).
Results
A total of 47,821 participants who reported being a current undergraduate student completed the Spring 2017 NCHA-II. Demographic characteristics are described in Table 1. In summary, 40.4% were 21 years of age or older, two thirds (67.2%) were female, more than two thirds (69.4%) were white, and most (89.6%) were non-Hispanic. Current membership in a fraternity or sorority was reported by 12.4% of the participants. Past year participation in college athletics was reported by 8.9% of participants for varsity sports, 10.8% for club sports, and 18.9% for intramural sports.
Table 1.
Sample demographic characteristics and current cigarette, waterpipe tobacco, and electronic cigarette (ECIG) use.
| Whole sample N=47,821 |
Current Cigarette |
Current Waterpipe |
Current ECIG |
||||
|---|---|---|---|---|---|---|---|
| Characteristic | % | % | p | % | p | % | p |
| Overall | 9.5 | 3.3 | 4.9 | ||||
| Age | <0.001 | 0.206 | < 0.001 | ||||
| 18 | 15.2 | 7.6a | 3.6 | 6.0a | |||
| 19 | 23.5 | 8.2a | 3.1 | 5.8a | |||
| 20 | 20.9 | 9.2b | 3.6 | 4.5b | |||
| 21+ | 40.4 | 11.1c | 3.3 | 4.2b | |||
| Gender | <0.001 | < 0.001 | < 0.001 | ||||
| Male | 30.3 | 13.0a | 4.5a | 8.0a | |||
| Female | 67.2 | 7.7b | 2.8b | 3.4b | |||
| Transgender or other identity | 2.6 | 16.5c | 5.9c | 8.4a | |||
| Race | <0.001 | < 0.001 | < 0.001 | ||||
| White | 69.4 | 9.8a | 2.9a | 5.3a | |||
| Black | 4.8 | 5.1b | 4.9b | 2.5b | |||
| Asian | 10.2 | 8.0c | 3.6c | 3.7c | |||
| Other or more than one race | 15.6 | 10.6d | 4.5b | 4.7d | |||
| Ethnicity | 0.978 | < 0.001 | 0.199 | ||||
| Hispanic | 10.4 | 9.5 | 4.5a | 4.6 | |||
| Not Hispanic | 89.6 | 9.5 | 3.2b | 5 | |||
| Fraternity or Sorority Member | <0.001 | < 0.001 | < 0.001 | ||||
| Yes | 12.4 | 14.6a | 5.7a | 8.1a | |||
| No | 87.6 | 8.8b | 3.0b | 4.5b | |||
| Varsity sports (last 12 months) | <0.001 | 0.01 | 0.903 | ||||
| Yes | 8.9 | 6.2a | 2.7a | 4.9 | |||
| No | 91.1 | 9.8b | 3.4b | 4.9 | |||
| Club sports (last 12 months) | 0.754 | 0.002 | 0.195 | ||||
| Yes | 10.8 | 9.5 | 4.1a | 5.3 | |||
| No | 89.2 | 9.6 | 3.3b | 4.9 | |||
| Intramural sports (last 12 months) | 0.004 | < 0.001 | < 0.001 | ||||
| Yes | 18.9 | 10.3a | 4.0a | 6.2a | |||
| No | 81.1 | 9.3b | 3.2b | 4.6b |
Note. Values in the “Whole Sample” column represent the percentages of all participants who endorsed each of the participant characteristics. The columns for “Current Cigarette,” “Current Waterpipe,” and “Current ECIG” represent the percentage of participants from each participant characteristic who reported current tobacco use by tobacco product type among those who responded to each tobacco product question. Complete data for tobacco use questions included 47,706 for cigarette smoking, 47,677 for waterpipe tobacco smoking, and 47,533 for ECIG use. P-values for group comparison chi-square tests. Different superscript letters indicate significant differences in current tobacco use percentages within a demographic characteristic.
Cigarette smoking was the most commonly reported tobacco product used with 9.5% of the participants in the total sample reporting current cigarette smoking (See Figure 1). Cigarette smoking was more common among older participants, those who self-reported gender as male or non-binary (i.e., transgender or other gender identity), and those who identified as being white, Asian, or other, biracial, or multiracial (ps < .05). Fraternity/sorority members had the highest rates of cigarette smoking with 14.6% reporting current use. Varsity athletes had the lowest rates of cigarette smoking with 6.2% reporting current use (p < .05).
Figure 1.
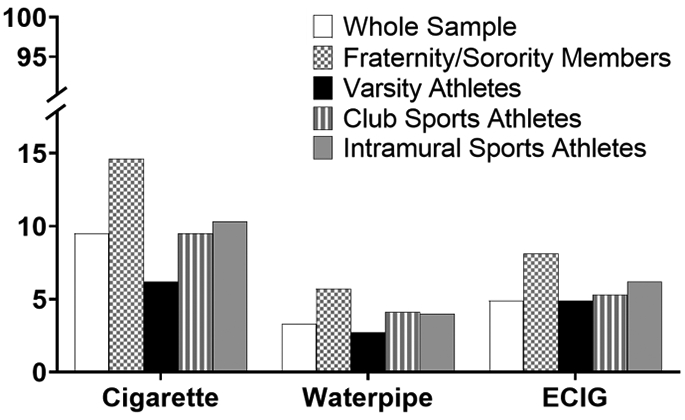
Prevalence of current cigarette smoking, waterpipe tobacco smoking, and electronic cigarette use among the entire sample, fraternity/sorority members, varsity sports athletes, club sports athletes, and intramural sports athletes.
Prevalence of WTS was lowest of the three tobacco products examined with 3.3% of participants reporting current use (see Figure 1). WTS was more common among those who reported their gender as male or non-binary, those who identified their race as black, other, biracial, or multiracial, and those who reported Hispanic ethnicity (ps < .05). Fraternity/sorority members had the highest prevalence of WTS with 5.7% reporting current use (p < .05). The lowest rates of WTS were reported by varsity sports athletes, with 2.7% reporting current use (p < .001).
ECIGs were the second most popular of the products examined: current use was reported by 4.9% of the total sample (see Figure 1). ECIG use was more common among younger (18- and 19-year-old) participants; those who identified as men and non-binary gender; and white, other, biracial, or multiracial race (ps < .05). Fraternity/sorority members had the highest rate of current ECIG use (8.1%) and were significantly more likely to use ECIGs compared to non-members (p < .05). With regard to athlete status, all athlete groups had the same or higher percentages of ECIG use relative to their respective “non-athlete” groups. Specifically, 4.9% of varsity sports athletes reported current ECIG use versus 4.9% of non-varsity sports athletes, 5.3% of club sports athletes reported current ECIG use versus 4.9% of non-club sports athletes, and 6.2% of intramural sports athletes reported current ECIG use vs. 4.6% non-intramural sports athletes. This difference was not statistically significant for varsity athlete status or club sport athlete status, but was for intramural sports athlete status (ps < .05).
Table 2 and Figure 2 display the results of the multivariate logistic regression analyses. With regard to fraternity/sorority member status, fraternity/sorority members were significantly more likely to report current use of all three tobacco products examined after adjusting for age, gender, race, and ethnicity. Specifically, relative to non-fraternity/sorority members, fraternity/sorority members had 1.82 times the odds (95% CI = 1.67–1.98) of reporting current cigarette smoking, 1.99 times the odds (95% CI = 1.75–2.27) of reporting current WTS, and 1.95 times the odds (95% CI = 1.74–2.18) of reporting current ECIG use.
Table 2.
Adjusted odds ratios from logistic regression predicting current (past 30-day) cigarette, waterpipe, and electronic cigarette (ECIG) use.
| Group | Cigarette | Waterpipe | ECIG |
|---|---|---|---|
| Fraternity/Sorority member | 1.82 (1.67, 1.98) | 1.99 (1.75, 2.27) | 1.95 (1.74, 2.18) |
| Varsity sports athlete | 0.60 (0.53, 0.69) | 0.79 (0.64, 0.97) | 0.88 (0.75, 1.03) |
| Club sports athlete | 0.94 (0.84, 1.04) | 1.12 (0.95, 1.32) | 0.90 (0.78, 1.03) |
| Intramural sports athlete | 0.94 (0.86, 1.02) | 1.09 (0.96, 1.25) | 1.02 (0.92, 1.14) |
Note. Adjusted odds ratios (AORs) were adjusted for age, gender, race, and ethnicity. The reference group for each analysis was non-members or non-participants (e.g., fraternity or sorority members vs. non-fraternity or sorority members, varsity athletes vs. non-varsity athletes; club sports athletes vs. non-club sports athletes; intramural sports athletes vs. non-intramural sports athletes).
Figure 2.
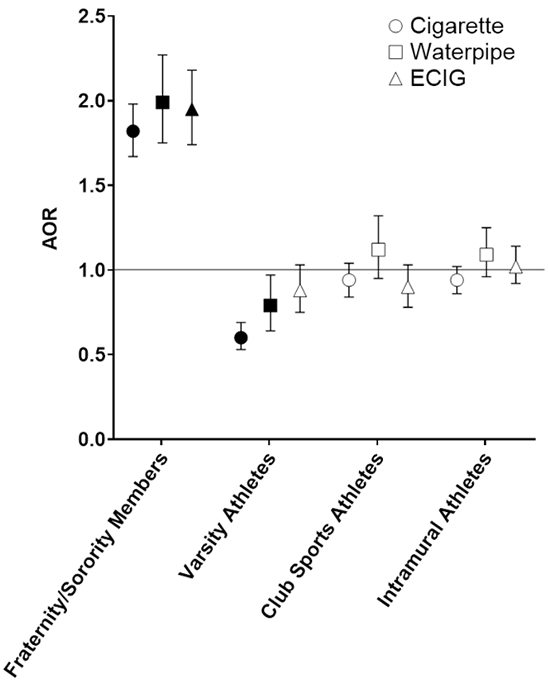
Adjusted odds ratios (AORs) from logistic regressions predicting current (past 30-day) cigarette, waterpipe, and electronic cigarette (ECIG) use. Filled symbols indicate significant AORs (p < .05). All analyses were adjusted for age, gender, race, and ethnicity. The reference group for each analysis was non-members or non-participants (e.g., fraternity or sorority members vs. non-fraternity or sorority members, varsity athletes vs. non-varsity sports athletes; club sports athletes vs. non–club sports athletes, intramural sports athletes vs. non-intramural sports athletes).
Varsity sports athlete status was associated negatively with current cigarette smoking and WTS, but not ECIG use. Specifically, relative to those who were not varsity sports athletes, varsity sports athletes had a decreased odds (AOR = 0.60, 95% CI = 0.53–0.69) of reporting current cigarette smoking and a decreased odds (AOR = 0.79, 95% CI = 0.64–0.97) of reporting current WTS. However, varsity sports athlete status was not associated with increased or decreased odds of current ECIG use. Club sports athlete status and intramural sport athlete status was not associated with current use of cigarettes, waterpipe, or ECIGs.
Discussion
This study examined the association of tobacco use with fraternity/sorority membership and participation in collegiate athletics among college students in the United States. Analysis indicated that fraternity and sorority members appear to be at increased risk for all tobacco products examined in the current study, including traditional tobacco products (i.e., cigarettes) and alternative tobacco products (i.e., waterpipe and ECIGs). Conversely, participation in varsity sports appeared to be protective for current cigarette use and WTS, but this protective effect was not present for ECIG use.
The findings from this study provide an important addition to the discussion of how ECIGs may impact public health. Scientists and health professionals continue to debate what public health impact ECIGs may have. Discussions often focus on specific groups who might use ECIGs including those who may benefit from ECIGs, such as current cigarette smokers who may attempt to switch completely to ECIGs, or youth, who have the highest prevalence rates8 and among whom ECIGs have no public health benefit. However, a group that has been given considerably less attention is the college population, a group who may be at risk for tobacco product use, but where ECIG use represent less of a potential benefit relative to long term highly addicted cigarette smokers. In the current study, fraternity/sorority members represented a group that was at higher risk for tobacco use including cigarette smoking, WTS, and ECIG. While efforts should still be made to prevent tobacco use among high risk groups like fraternity/sorority members, the negative impact of ECIG use on these groups who are already use tobacco products at higher rates may be less significant.
In contrast, there are other college student groups in which ECIGs may have a greater negative impact. In the current study, varsity athletes, a college student population that research has identified as having reduced odds for cigarette smoking and WTS, did not have differential risk for ECIG use relative to non-varsity athletes. Although varsity athletes in the current study did not have increased odds of ECIG use, varsity athlete status did not represent a protective factor for ECIG use as it appeared to be for cigarette smoking and WTS. Additionally, research has demonstrated that youth and young adults who initiate ECIG use are at increased risk for subsequent cigarette smoking.25-28 While varsity athlete status may be protective for cigarette smoking or WTS, future research is needed to see if ECIG use blunts this potential protective factor.
In discussing possible reasons for varsity athletes having lower rates of cigarette smoking and WTS, Primack and colleagues suggested that varsity athletes may have less time to engage in risk-taking behaviors or perceive that cigarette smoking and WTS may carry severe cardiovascular or respiratory risks that could impact athletic performance.36 Research on ECIGs has reported that convenience, such as the ability to “vape” anywhere at any time, is a positive attribute many associated with ECIG use,22,23 eliminating a potential perceived barrier for tobacco use among varsity athletes. Additionally, varsity athletes may not associate ECIGs with the same or risks related to health or athletic performance as they do with other tobacco products. Therefore, ECIGs may represent a tobacco product innovation that is perceived as more compatible with an elite athlete lifestyle. Future studies should examine ECIG perceptions including reasons for use among varsity athletes as well as other groups at lower risk for other tobacco product use to inform prevention efforts among these populations.
College represents a unique time and environment for young adults where many have opportunities for greater independence coupled with increased opportunities to engage in risk-taking behaviors. WTS appears to fit in with college night life/drinking culture,37 and many WTS bars38 and vape shops39 are concentrated in college towns adding to the potential for alternative tobacco use among college students. In addition to continuing to monitor alternative tobacco use trends among youth and young adults as a whole, college students and other youth and young adult subpopulations should be monitored to identify specific groups that may be at risk for traditional and alternative tobacco product use, including those not typically considered at-risk for tobacco product use. Future studies may also track college students over time to determine what factors may promote or inhibit tobacco use experimentation and initiation to inform prevention efforts.
Researchers may attempt to identify factors that are common to all tobacco products as well as specific to certain tobacco products such as ECIGs. These could be used to inform tobacco prevention efforts. Importantly, while the college environment may expose young adults to opportunities for risk-taking behaviors, the college environment also provides intervention opportunities to prevent tobacco use because of the many available university resources. For example, universities in many cases have the authority to create campus-wide initiatives such as tobacco-free policies that have been shown to be effective for reducing tobacco use.40,41 Environment and policy changes at the university level coupled with education of the risks of all tobacco products may greatly decrease the likelihood of all types of tobacco product use among all college students. Such environmental and policy changes also have the potential to denormalize tobacco use, including use of emerging alternative tobacco products.
This study had several limitations. This study examined cross-sectional associations between fraternity/sorority membership and athlete status and tobacco use limiting the ability to assess causal relationships. Additionally, while the participants in the current analysis represent a large national sample from the U.S., because colleges self-select to participate in the NCHA-II study the data are not nationally representative of all college students. Future studies that examine reasons for initiation of various tobacco products or that track college students longitudinally are needed to better understand the causes of the associations reported in the current study. The rates of tobacco use reported in this study, particularly for ECIG use, appear lower than other prevalence estimates of young adults in the U.S. This may be partly due to the wording of the NCHA-II survey questions for WTS and ECIG use. Because there are many different colloquial terms used to describe waterpipe (e.g., hookah) and ECIGs (e.g., vapes), some survey participants may have failed to report current use of waterpipe or ECIGs when they in fact should have been classified as current users. Surveys that utilize pictures and provide descriptions of alternative tobacco products may be more likely to capture all current tobacco product users.42 While data for the NCHA-II examined in the current study were collected recently (i.e, 2017), these data were collected before the rapid increase in popularity of “pod mod” ECIG devices, such as JUUL which currently represents approximately 75% of the ECIG market share.20 These products are popular among youth and young adults.43 Research should examine if the increase of JUUL and other pod mod ECIG use has had an impact on the populations that may be at risk for ECIG use. Finally, while cigarettes and waterpipe represent a single type of tobacco product, ECIGs are a class of tobacco products that include a wide variety of devices. Future analyses that examine population subgroups at risk for ECIG may consider if certain subgroups are at risk for specific ECIG device types, but not others.
This study highlights that young adult and college student populations have differing risk profiles for tobacco product use and these risk profiles may be specific to certain tobacco products. Some groups, such as fraternity/sorority members, are likely at risk for many forms of tobacco product use as well as other substance use. Additionally, other groups, such as college varsity sports athletes, who are typically considered at low risk for tobacco use may be at risk for ECIG use. Indeed, previous research has identified that some youth who initiate ECIG use may have been at risk for cigarette smoking already, but other youth who are not considered at risk for cigarette smoking may experiment with and initiate ECIG use.27 As the tobacco product marketplace continues to evolve and new products become available, youth and young adult tobacco prevention efforts should continue to target those known to be at risk for other tobacco products, as they will also likely be at risk for emerging/alternative tobacco products. During a time when new tobacco products are introduced to the market at a rapid rate, prevention efforts also should be conscious of the potential appeals of new tobacco products among population subgroups not typically at risk for tobacco use.
Acknowledgments
This research was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number 2U54DA036105–06, the Center for Tobacco Products of the U.S. Food and Drug Administration, and by East Carolina University. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH or the FDA.
Footnotes
Disclosure statement
The authors have no conflicts of interest to report.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. http://www.ncbi.nlm.nih.gov/books/NBK179276/. Accessed August 21, 2017. [PubMed] [Google Scholar]
- 2.Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe Tobacco Smoking: An Emerging Health Crisis in the United States. Am J Health Behav. 2010;34(3):275–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maziak W The waterpipe: a new way of hooking youth on tobacco. Am J Addict. 2014;23(2):103–107. doi: 10.1111/j.1521-0391.2013.12073.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soule EK, Lipato T, Eissenberg T. Waterpipe tobacco smoking: A new smoking epidemic among the young? Curr Pulmonol Rep. 2015;4(4):163–172. doi: 10.1007/s13665-015-0124-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011;115(1–2):131–136. doi: 10.1016/j.drugalcdep.2011.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnett TE, Smith T, He Y, et al. Evidence of emerging hookah use among university students: a cross-sectional comparison between hookah and cigarette use. BMC Public Health. 2013;13:302. doi: 10.1186/1471-2458-13-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sidani JE, Shensa A, Yabes J, Fertman C, Primack BA. Waterpipe tobacco use in college and non-college young adults in the USA. Fam Pract. 2019;36(2):103–109. doi: 10.1093/fampra/cmy037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gentzke AS. Vital Signs: Tobacco Product Use Among Middle and High School Students — United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2019;68. doi: 10.15585/mmwr.mm6806e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Primack BA, Sidani J, Agarwal AA, Shadel WG, Donny EC, Eissenberg TE. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann Behav Med Publ Soc Behav Med. 2008;36(1):81–86. doi: 10.1007/s12160-008-9047-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grekin EmilyR, Ayna D. Waterpipe Smoking Among College Students in the United States: A Review of the Literature. J Am Coll Health. 2012;60(3):244–249. [DOI] [PubMed] [Google Scholar]
- 11.Lipkus IM, Eissenberg T, Schwartz-Bloom RD, Prokhorov AV, Levy J. Affecting Perceptions of Harm and Addiction among College Waterpipe Tobacco Smokers. Nicotine Tob Res. 2011;13(7):599–610. doi: 10.1093/ntr/ntr049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith SY, Curbow B, Stillman FA. Harm perception of nicotine products in college freshmen. Nicotine Tob Res. 2007;9(9):977–982. doi: 10.1080/14622200701540796 [DOI] [PubMed] [Google Scholar]
- 13.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37(6):518–523. doi: 10.1016/j.amepre.2009.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Monzer B, Sepetdjian E, Saliba N, Shihadeh A. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc. 2008;46(9):2991–2995. doi: 10.1016/j.fct.2008.05.031 [DOI] [PubMed] [Google Scholar]
- 15.Nguyen T, Hlangothi D, Martinez RA, et al. Charcoal burning as a source of polyaromatic hydrocarbons in waterpipe smoking. J Environ Sci Health B. 2013;48(12):1097–1102. doi: 10.1080/03601234.2013.824300 [DOI] [PubMed] [Google Scholar]
- 16.Waziry R, Jawad M, Ballout RA, Al Akel M, Akl EA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2017;46(1):32–43. doi: 10.1093/ije/dyw021 [DOI] [PubMed] [Google Scholar]
- 17.Wang TW, Asman K, Gentzke AS, et al. Tobacco Product Use Among Adults — United States, 2017. Morb Mortal Wkly Rep. 2018;67(44):1225–1232. doi: 10.15585/mmwr.mm6744a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Breland A, Soule E, Lopez A, Ramôa C, El-Hellani A, Eissenberg T. Electronic cigarettes: what are they and what do they do? Ann N Y Acad Sci. 2017;1394(1):5–30. doi: 10.1111/nyas.12977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McMillen RC, Gottlieb MA, Shaefer RMW, Winickoff JP, Klein JD. Trends in Electronic Cigarette Use Among U.S. Adults: Use is Increasing in Both Smokers and Nonsmokers. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2015;17(10):1195–1202. doi: 10.1093/ntr/ntu213 [DOI] [PubMed] [Google Scholar]
- 20.King BA, Gammon DG, Marynak KL, Rogers T. Electronic Cigarette Sales in the United States, 2013–2017. JAMA. 2018;320(13):1379–1380. doi: 10.1001/jama.2018.10488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooper M, Loukas A, Harrell MB, Perry CL. College students’ perceptions of risk and addictiveness of e-cigarettes and cigarettes. J Am Coll Health J ACH. 2017;65(2):103–111. doi: 10.1080/07448481.2016.1254638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soule EK, Rosas SR, Nasim A. Reasons for electronic cigarette use beyond cigarette smoking cessation: A concept mapping approach. Addict Behav. 2016;56:41–50. doi: 10.1016/j.addbeh.2016.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel D, Davis KC, Cox S, et al. Reasons for current E -cigarette use among U.S. adults. Prev Med. 2016;93:14–20. doi: 10.1016/j.ypmed.2016.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saddleson ML, Kozlowski LT, Giovino GA, et al. Risky behaviors, e-cigarette use and susceptibility of use among college students. Drug Alcohol Depend. 2015;149:25–30. doi: 10.1016/j.drugalcdep.2015.01.001 [DOI] [PubMed] [Google Scholar]
- 25.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association Between Initial Use of e-Cigarettes and Subsequent Cigarette Smoking Among Adolescents and Young Adults: A Systematic Review and Meta-analysis. JAMA Pediatr. 2017;171(8):788–797. doi: 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Primack BA, Shensa A, Sidani JE, et al. Initiation of Traditional Cigarette Smoking after Electronic Cigarette Use Among Tobacco-Naïve US Young Adults. Am J Med. 2018;131(4):443.e1–443.e9. doi: 10.1016/j.amjmed.2017.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barrington-Trimis JL, Kong G, Leventhal AM, et al. E-cigarette Use and Subsequent Smoking Frequency Among Adolescents. Pediatrics. 2018;142(6). doi: 10.1542/peds.2018-0486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berry KM, Fetterman JL, Benjamin EJ, et al. Association of Electronic Cigarette Use With Subsequent Initiation of Tobacco Cigarettes in US Youths. JAMA Netw Open. 2019;2(2):e187794–e187794. doi: 10.1001/jamanetworkopen.2018.7794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheney MK, Harris LW, Gowin MJ, Huber J. Smoking and membership in a fraternity or sorority: a systematic review of the literature. J Am Coll Health J ACH. 2014;62(4):264–276. doi: 10.1080/07448481.2014.891595 [DOI] [PubMed] [Google Scholar]
- 30.Scott-Sheldon LAJ, Carey KB, Carey MP. Health Behavior and College Students: Does Greek Affiliation Matter? J Behav Med. 2008;31(1):61–70. doi: 10.1007/s10865-007-9136-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sidani JE, Shensa A, Primack BA. Substance and hookah use and living arrangement among fraternity and sorority members at US colleges and universities. J Community Health. 2013;38(2):238–245. doi: 10.1007/s10900-012-9605-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peretti-Watel P, Guagliardo V, Verger P, Pruvost J, Mignon P, Obadia Y. Sporting activity and drug use: alcohol, cigarette and cannabis use among elite student athletes. Addiction. 2003;98(9):1249. [DOI] [PubMed] [Google Scholar]
- 33.Yusko DA, Buckman JF, White HR, Pandina RJ. Alcohol, Tobacco, Illicit Drugs, and Performance Enhancers: A Comparison of Use by College Student Athletes and Nonathletes. J Am Coll Health J ACH. 2008;57(3):281–290. doi: 10.3200/JACH.57.3.281-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martinsen M, Sundgot‐Borgen J. Adolescent elite athletes’ cigarette smoking, use of snus, and alcohol. Scand J Med Sci Sports. 2014;24(2):439–446. doi: 10.1111/j.1600-0838.2012.01505.x [DOI] [PubMed] [Google Scholar]
- 35.Lisha NE, Sussman S. Relationship of high school and college sports participation with alcohol, tobacco, and illicit drug use: A review. Addict Behav. 2010;35(5):399–407. doi: 10.1016/j.addbeh.2009.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Primack BA, Fertman CI, Rice KR, Adachi-Mejia AM, Fine MJ. Waterpipe and Cigarette Smoking Among College Athletes in the United States. J Adolesc Health. 2010;46(1):45–51. doi: 10.1016/j.jadohealth.2009.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soule EK, Barnett TE, Curbow BA. Keeping the night going: the role of hookah bars in evening drinking behaviours. Public Health. 2012;126(12):1078–1081. doi: 10.1016/j.puhe.2012.06.010 [DOI] [PubMed] [Google Scholar]
- 38.Kates FR, Salloum RG, Thrasher JF, Islam F, Fleischer NL, Maziak W. Geographic Proximity of Waterpipe Smoking Establishments to Colleges in the U.S. Am J Prev Med. 2016;50(1):e9–e14. doi: 10.1016/j.amepre.2015.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dai H, Hao J. Geographic density and proximity of vape shops to colleges in the USA. Tob Control Lond. 2017;26(4):379. doi: 10.1136/tobaccocontrol-2016-052957 [DOI] [PubMed] [Google Scholar]
- 40.Seo DC, Macy JT, Torabi MR, Middlestadt SE. The effect of a smoke-free campus policy on college students’ smoking behaviors and attitudes. Prev Med. 2011;53(4–5):347–352. doi: 10.1016/j.ypmed.2011.07.015 [DOI] [PubMed] [Google Scholar]
- 41.Lee JG, Fanney LM, Goldstein AO. Cigarette butts near building entrances: what is the impact of smoke-free college campus policies? Tob Control. 2013;22(2):107–112. doi: 10.1136/tobaccocontrol-2011-050152 [DOI] [PubMed] [Google Scholar]
- 42.Weaver SR, Kim H, Glasser AM, et al. Establishing consensus on survey measures for electronic nicotine and non-nicotine delivery system use: Current challenges and considerations for researchers. Addict Behav. 2018;79:203–212. doi: 10.1016/j.addbeh.2017.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vallone DM, Bennett M, Xiao H, Pitzer L, Hair EC. Prevalence and correlates of JUUL use among a national sample of youth and young adults. Tob Control. October 2018:tobaccocontrol-2018–054693. doi: 10.1136/tobaccocontrol-2018-054693 [DOI] [PubMed] [Google Scholar]


