Background
Who could have imagined that a virus in the 21st century could so quickly destabilize the world? An economic, health, and social catastrophe spread worldwide in a manner of a few weeks. Starting from a small outbreak in the middle of China, the SARS-CoV-2 Coronavirus is hitting the world hard with 1,863,406 confirmed cases and 115,225 deaths worldwide as of 13 April 2020, and the global curve still seems to be on an exponential upward slope.1
Nonetheless, on 30 January in Geneva, Switzerland, the Director-General of the World Health Organization made public that the outbreak of the new coronavirus 2019 met the criteria of a public health emergency of international concern.2 In spite of this, more than 1 month later, neither in Europe nor in the United States, no clear and coherent response from experts or political leaders on how to deal with this exceptional situation had been reported.
In March 2020, the region of Lombardy, Italy, found itself overwhelmed by the rapid spread of the epidemic.3 , 4 The disaster reported in northern Italy seemed to have awakened the other European countries, each taking similar but nevertheless different measures.
Geneva, Switzerland, 1 Example Among Others
Switzerland has a population of 8.6 million, with Zurich and Geneva as its economic capitals.5 With its agglomeration, Geneva has a population of almost 600,000 and 1.5 million for the Lake Geneva region. Geneva is the center of 23 international organizations including the European headquarters of the United Nations, International Committee of the Red Cross, World Trade Organization, and World Health Organization.6
On 16 March 2020, the Federal Council declared Switzerland to be in an “extraordinary situation” until 19 April; in the context of Art. 7 of the Epidemics Act, the cantons must comply with federal regulations.7 Restaurants, bars, nonessential shops, and places of leisure and entertainment will thus remain closed until at least April 19, which will probably be postponed. Border controls with Germany, France, and Austria will be introduced. The Federal Council is providing up to 8000 military personnel for the health, logistics, and security system until the end of June.
Geneva and Its Neurosurgical Department
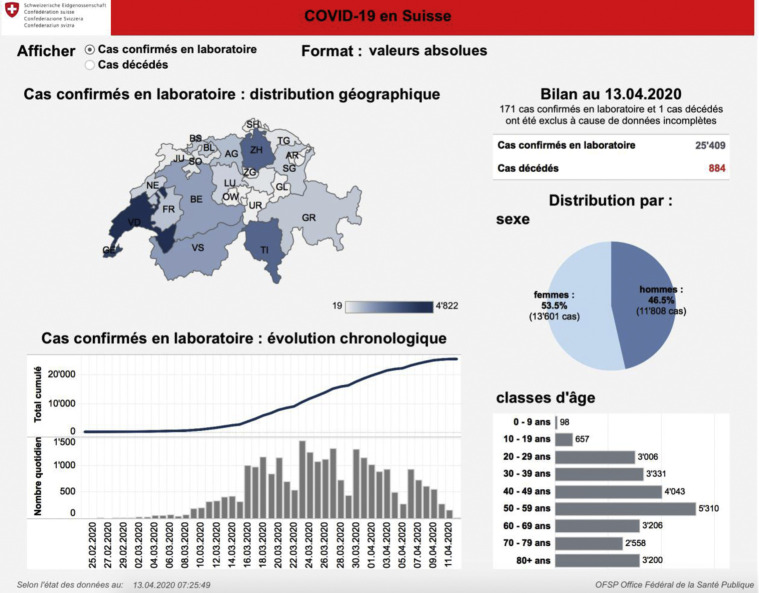
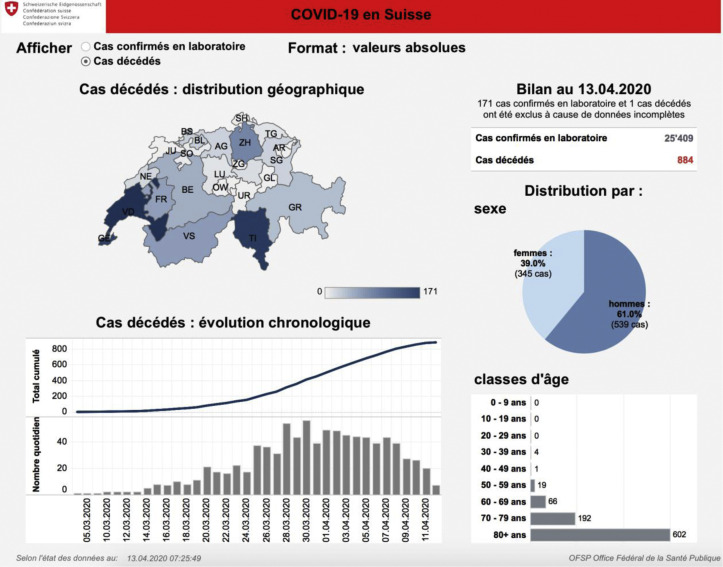
To date, Easter Monday (13 April 2020), more than 25,000 COVID-19−positive cases have been confirmed in laboratories and 884 deaths have been recorded for COVID-19 according to the Federal Office of Public Health (Figures 1 and 2 ), and these numbers are steadily increasing. At its peak, Geneva's university hospitals (in French “Hopitaux Universitaires de Genève” or HUG), had to deal with 500 patients hospitalized for COVID-19, of which 72 comprised intubated patients on the same day.
Figure 1.
Summary of the Situation in Switzerland: COVID-19 Laboratory-Confirmed Cases as of 13 April, 2020, According to the Federal Office of Public Health. Laboratory-confirmed cases, Geographic distribution, Chronologic evolution, Women, Men, and Age groups. From the Federal Office of Public Health.8
Figure 2.
Summary of the Situation in Switzerland: Deceased Cases of COVID-19 as of 13 April, 2020, According to the Federal Office of Public Health. Cases of death, Distribution, Geographic distribution, Chronologic evolution, Women, Men, and Age groups. From the Federal Office of Public Health.8
HUG has also taken drastic measures with the aim of increasing their capacity to deal with the epidemic. Entire surgical units and other departments have been completely modified to accommodate COVID-19 patients only. This also implies a reassignment of medical and nursing staff; for example, 50% of our neurosurgical residents were trained in 48 hours in intensive care management of acute respiratory distress syndrome and then permanently assigned to the crisis unit managing the distribution of physicians for COVID units. Furthermore, the elective operating rooms are completely locked down and general management has imposed the cancellation of all vacations for HUG employees (i.e., 11,730 of them). The neurosurgery department with its high-tech platform is maximally concerned by these institutional efforts (i.e., by the closure of its hybrid vascular operating rooms and of its intraoperative high-field magnetic resonance suite).
Collaboration between private clinics and public hospitals has been established, notably to operate on spinal pathologies. Urgent pathologies that are not COVID positive are redirected to the various private clinics in the canton of Geneva. However, as the technical platform in private clinics does not allow for complex cranial surgery, some of our complex surgeries, such as ruptured arteriovenous cerebral malformations or ruptured aneurysms, had to be transferred to other Swiss university hospitals, which were and are less impacted by the COVID-19 situation.
How to Ensure the Continued Training of Our Residents
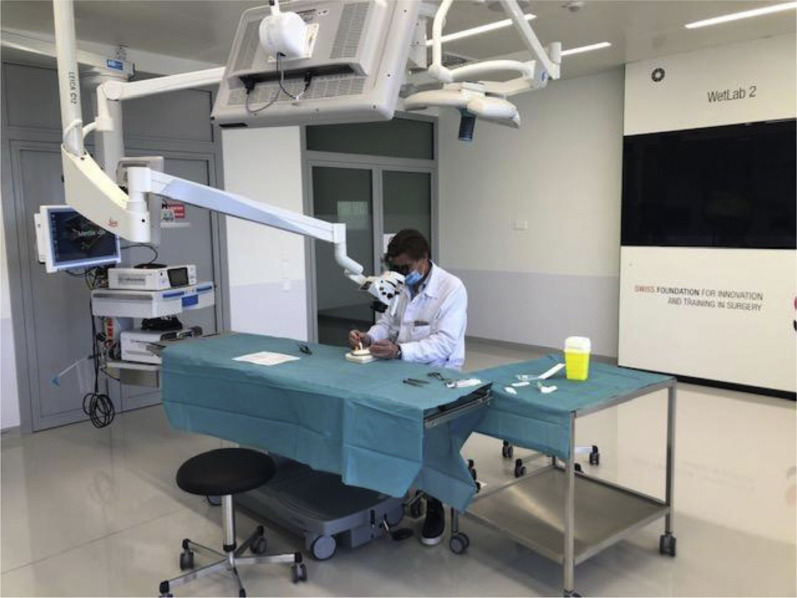
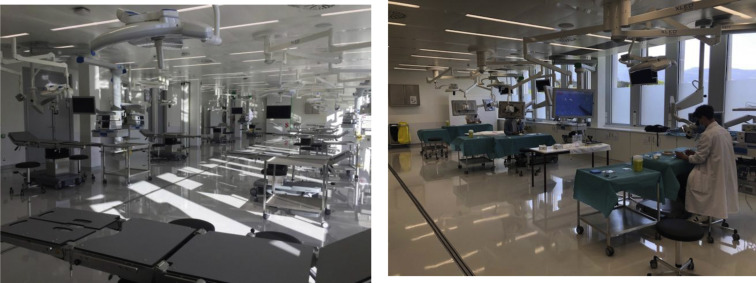
Good morale rhymes with good team spirit. The fact that we have assigned 50% of our residents to COVID-19 units does not prevent us from ensuring that they maintain a minimum level of training. To counter this, we have introduced daily microsurgery courses in our training rooms at the Swiss Foundation for Innovation and Training in Surgery. Of course, this is done in a hygienic way, with 1 resident per table with >3 m distance from each other (Figures 3 and 4 ). A pool of multiple-choice questions has been created to allow the residents to test their knowledge and to guide their reading and learning during this slowed period on their gaps.
Figure 3.
Professor giving microsuture training instructions to residents.
Figure 4.
Course room for surgical training at Swiss Foundation for Innovation and Training in Surgery with respective operating tables and microscopes and the residents practicing.
Is the Remedy Worse Than the Devil?
We have often heard it, “the remedy worse than the devil,” especially from economists and politicians: A deep recession in the coming years could lead to a catastrophe more serious and deadlier than the virus itself. Is the remedy applied in some countries and hospitals likely to prove worse than the disease itself? All elective surgical activity has been stopped in many centers affected by the epidemic, as in HUG in Geneva. Even worse, although sometimes necessary, patients are afraid to go to the hospital and cancel their visit. This same observation has also been relayed by the neurosurgical clinics in Bergamo in Italy and other internationally renowned centers around the world.3 , 4 , 9 , 10
Would it have been a valid alternative to, for example, mount a fully equipped modular COVID-19 center outside the campus of the university medical center, as it is currently done in other cities such as Zagreb or Moscow, to keep free access to the high-quality technical and operating room platform? There are so many speculations around this topic, and we will get answers to those questions long after the current crisis, only when all this has been worked up in detail.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Coronavirus COVID-19 (2019-nCoV) https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Available at:
- 2.Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) Available at:
- 3.Cenzato M., DiMeco F., Fontanella M., Locatelli D., Servadei F. Editorial. Neurosurgery in the storm of COVID-19: suggestions from the Lombardy region, Italy (ex malo bonum) https://doi.org/10.3171/2020.3.JNS20960 [e-pub ahead of print]. J Neurosurg. [DOI] [PMC free article] [PubMed]
- 4.Bernucci C., Brembilla C., Veiceschi P. Effects of the COVID-19 outbreak in Northern Italy: perspectives from the Bergamo neurosurgery department. https://doi.org/10.1016/j.wneu.2020.03.179 [e-pub ahead of print]. World Neurosurg. [DOI] [PMC free article] [PubMed]
- 5.Federal Statistical Office Switzerland's population continued to grow and age in 2019—population change in 2019: provisional results press release. Federal Statistical Office. 2020. https://www.bfs.admin.ch/bfs/fr/home/statistiques/population/effectif-evolution.html Available at:
- 6.Facts and figures about International Geneva. https://www.eda.admin.ch/missions/mission-onu-geneve/en/home/geneve-international/faits-et-chiffres.html Available at:
- 7.RS 818.101.1 Ordinance of 29 April 2015 on the fight against communicable diseases in humans (Ordinance on Epidemics) https://www.admin.ch/opc/fr/classified-compilation/20133212/index.html Available at:
- 8.Office fédéral de la santé publique [Federal Office of Public Health] https://covid-19-schweiz.bagapps.ch/fr-1.html Available at:
- 9.Kondziolka D., Couldwell W.T., Rutka J.T. Introduction. On pandemics: the impact of COVID-19 on the practice of neurosurgery. https://doi.org/10.3171/2020.3.JNS201007 [e-pub ahead of print]. J Neurosurg. [DOI] [PMC free article] [PubMed]
- 10.Perin A., Servadei F., DiMeco F., “Hub and Spoke” Lombardy Neurosurgery Group May we deliver neuro-oncology in difficult times (e.g., COVID-19)? https://doi.org/10.1007/s11060-020-03496-7 [e-pub ahead of print]. J Neurooncol. [DOI] [PMC free article] [PubMed]