Dear Editor,
We read with great interest the article by Zheng et al. published on 23 April 2020 in your esteemed journal. The authors conducted a meta-analysis to identify risk factors that could predict severe disease and mortality in patients with coronavirus disease 2019 (COVID-19). In their meta-analysis, using data from three studies, the authors reported that having a creatinine level of 133 µmol/L or more was associated with higher odds of having severe disease or mortality.1 Some literature suggests that the risk of acute kidney injury (AKI) in patients with COVID-19 is low. However, when AKI develops, it is usually an indicator of more severe disease and multi-organ dysfunction.
Multiple observational studies have been published that have reported the clinical features of hospitalized COVID-19 patients such as acute respiratory distress syndrome. However, studies that have reported the incidence of AKI are scant. In our study, we take one step further to quantitatively synthesized available literature and performed a single-arm meta-analysis of proportions to report the pooled incidence rate of AKI and renal replacement therapy (RRT) use in hospitalized patients with COVID-19.
The meta-analysis was performed in accordance to the Meta-analysis of Observational Studies in Epidermiology (MOOSE) guidelines. A comprehensive literature search was performed on PubMed, Embase, Scopus and Web of Science to identify articles from 1 Jan 2020 till 20 April 2020. Backward reference searching was also performed. Various combinations and permutations of the following search terms “coronavirus”, “COVID-19″, “SARS-COV-2″, “2019-nCOV”, “acute kidney injury” and “acute renal failure” were used. Two authors (JJN and YL) independently screened the articles and any disagreements were resolved by consensus between all authors. We included observational studies that reported the pooled incidence rates of AKI and RRT use in hospitalized patients with proven COVID-19. We excluded studies that were not peer-reviewed or did not utilize the KDIGO definition for AKI. Relevant data from articles that were included after full-text review were extracted by a single author (KP) and verified by another (JJN). Data such as study design, sample size, patient demographics and incidence of AKI and RRT use were extracted. The Newcastle-Ottawa Scale was used to assess the quality of the included articles.
The primary outcomes in this study are the pooled incidence rates of AKI in an overall hospital and intensive care unit (ICU) setting. The secondary outcomes are the pooled incidence rates of RRT use in an overall hospital and ICU setting. Meta-analysis of proportions was performed using a random-effects model with Freeman-Tukey double arcsine transformation for variance stabilization. All analyses were performed using Stata version 16 (StataCorp, College Station, TX, USA).
A total of nine studies were included (Table 1 )2 – 10. Three studies were prospective in nature, while six were retrospective. Most studies originated from China, except for one study from the United States of America. Seven studies included all patients that were hospitalized, whilst two studies included only patients admitted to an intensive care unit.
Table 1.
Summary of characteristics of included studies.
| Location | Study design | Study Setting | N | Age | Male | DMa | HTNb | CKDc | ICUd Admission | Mortality | AKIe, total | AKI, ICU | RRTf, total | RRT, ICU | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Arentz2, 2020 | USA | ROSg | ICU | 21 | 70i (43–92)l | 11 (52.4%) | 7 (33.3%) | NRi | 10 (47.6%) | NAj | 11 (52.4%)k | NA | 4 (19.1%) | NA | NR |
| Cheng3, 2020 | China | POSh | Hospital | 701 | 63 (50–71) | 367 (52.4%) | 100 (14.3%) | 233 (33.4%) | 14 (2.0%) | 73 (10.4%) | 113 (16.1%) | 36 (5.1%) | NR | NR | NR |
| Guan4, 2020 | China | ROS | Hospital | 1099 | 47 (35–58) | 637 (58.1%) | 81 (7.4%) | 165 (15.0%) | 8 (0.7%) | 55 (5.0%) | 15 (1.4%) | 6 (0.5%) | NR | 9 (0.8%) | NR |
| Huang5, 2020 | China | ROS | Hospital | 41 | 49 (41–58) | 30 (73.2%) | 8 (19.5%) | 6 (14.6%) | NR | 13 (31.7%) | 6 (14.6%) | 3 (7.3%) | 3 (23.1%) | 3 (7.3%) | 3 (23.1%) |
| Shi6, 2020 | China | POS | Hospital | 416 | 64 (21–95)m | 205 (49.3%) | 60 (14.4%) | 127 (30.5%) | 14 (3.4%) | NR | 57 13.7% | 8 (1.9%) | NR | 2 (0.5%) | NR |
| Wang7, 2020 | China | POS | Hospital | 116 | 54 (38–69) | 67 (57.8%) | 18 (15.5%) | 43 (37.1%) | 5 (4.3%) | 11 (9.5%) | 7 (6.0%) | 0 (0%) | NR | 5 (4.3%) | NR |
| Wang #28, 2020 | China | ROS | Hospital | 138 | 56 (42–68) | 75 (54.3%) | 14 (10.1%) | 43 (31.2%) | 4 (2.9%) | 36 (26.1%) | 6 (4.3%) | 5 (3.6%) | 3 (8.3%) | 2 (1.4%) | 2 (5.6%) |
| Yang9, 2020 | China | ROS | ICU | 52 | 59.7l ±13.3n | 35 (67.3%) | 9 (17.3%) | NR | NR | NA | 32 (61.5%)k | NA | 15 (28.8%) | NA | 9 (17.3%) |
| Zhou10, 2020 | China | ROS | Hospital | 191 | 56 (46–67) | 119 (62.3%) | 36 (18.8%) | 58 (30.4%) | 2 (1.0%) | 50 (26.2%) | 54 (28.3%) | 28 (14.7%) | NR | 10 (5.2%) | NR |
| Pooled incidence rate after meta-analysis of proportions (95% confidence intervals) | 3% (1% - 7%) |
19% (9% to 31%) |
2% (1% - 4%) |
13% (4% - 25%) |
|||||||||||
Age is represented in median (interquartile range) unless otherwise specified
aDiabetes mellitus.
Hypertension.
Chronic kidney disease.
Intensive care unit.
Acute kidney injury.
Renal replacement therapy.
Retrospective observational study.
Prospective observational study.
Not reported.
Not applicable.
Intensive care unit specific mortality.
Data represented as mean.
Data represented as range.
Data represented as standard deviations.
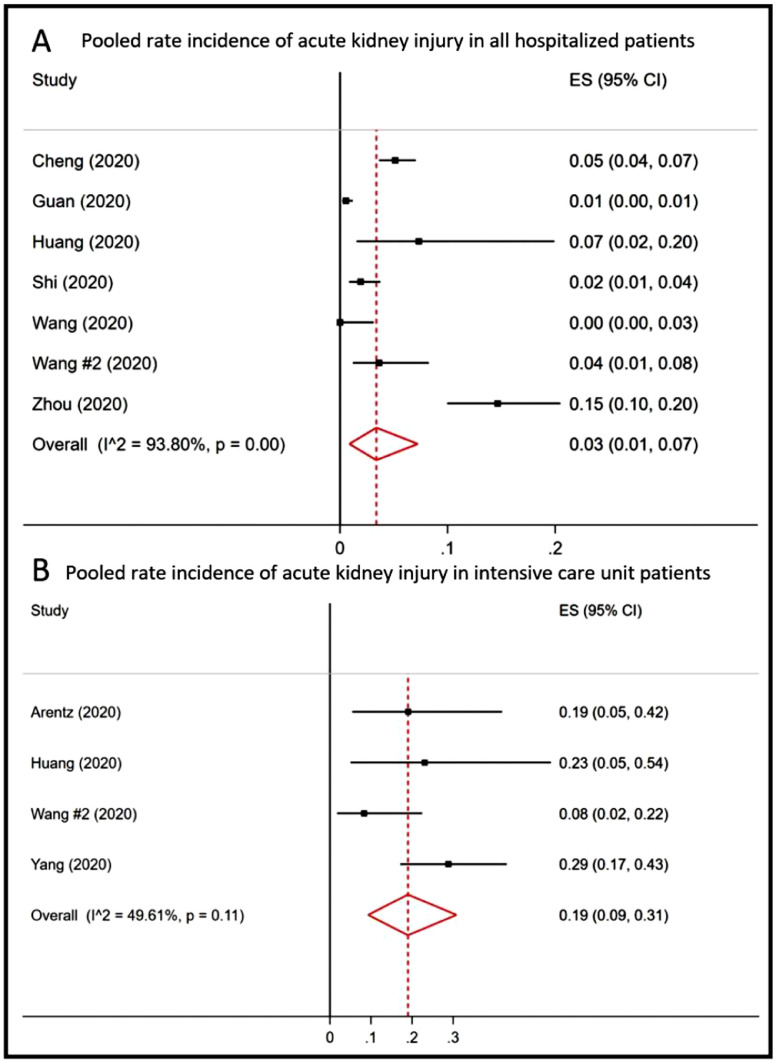
Seven studies reported the incidence of AKI in an overall hospital setting, varying from 0% to 14.7%.3 – 8 , 10 AKI occurred in 86 out of 2702 hospitalized patients. Meta-analysis of proportions revealed a pooled incidence rate of AKI of 3% (95% C.I. 1% - 7%, I2 = 93.8%) in all hospitalized patients (Fig. 1 A). Four studies reported the incidence of AKI in an ICU setting, varying from 8.3% to 28.8%.2 , 5 , 8 , 9 AKI occurred in 25 out of 122 ICU patients. Meta-analysis of proportions revealed a pooled incidence of AKI of 19% (95% C.I. 9% - 31%, I2 = 49.6%) in ICU patients (Fig. 1B).
Fig. 1.
Forest plot showing pooled rate incidences of acute kidney injury in (A) all hospitalized patients and (B) intensive care unit patients after meta-analysis of proportions.
Six studies reported the incidence of RRT use in an overall hospital setting, varying from 0.5% to 7.3%.4, 5, 6, 7, 8 , 10 RRT was used in 31 out of 2001 hospitalized patients. Meta-analysis of proportions revealed a pooled incidence of RRT use of 2% (95% C.I. 1% - 4%, I2 = 80.8%) in hospitalized patients. Only three studies reported the incidence of RRT use in an ICU setting, varying from 5.6% to 23.1%.5 , 8 , 9 RRT was used in 14 out of 101 ICU patients. Meta-analysis of proportions revealed a pooled incidence of RRT use of 13% (95% C.I. 4% - 25%, I2 = 47.5%).
We found that the overall risk of AKI in all hospitalized patients seemed to be low with a pooled incidence rate of 3%. This risk increases to 19% when patients are admitted to the ICU. Correspondingly, we found that the need for RRT in all hospitalized patients to be low with a pooled incidence of 2%. In ICU, the need for RRT increases to 13%. This is the first study that reported the pooled incidence rates of AKI and RRT use in an overall hospital and ICU specific setting. Although we cannot compare the pooled incidence rates of AKI and RRI between a general hospital and ICU setting, there is certainly an association between the development of AKI and ICU admission. Data from this study can potentially help in resource planning as the COVID-19 pandemic continues to affect multiple countries. This study also highlights the paucity of AKI data from the rest of the world as most studies are from mainland China.
There are, however, limitations to this study. A large majority of the included studies are from China and the results of this meta-analysis may not be applicable to other regions of the world. Second, some of the outcomes in this study had a high I2 value signifying significant variability in the effect sizes of the included studies. This may be explained by variations in study design, study population, or even viral genotype. In conclusion, we report the pooled incidences of AKI and the need for RRT in an overall hospital and ICU setting for patients diagnosed with COVID-19. More high-quality data is needed to better understand the risk of AKI and its implication on prognosis and mortality in COVID-19 patients.
Financial support
The authors declare no financial support was provided for the writing of this manuscript
Declaration of Competing Interest
The authors declare no relevant conflicts of interest.
References
- 1.Zheng Z., Peng F., Xu B., Zhao J., Liu H., Peng J. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arentz M., Yim E., Klaff L., Lokhandwala S., Riedo F.X., Chong M. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA. 2020;323(16):1612. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan W.-.J., Ni Z.-.Y., Hu Y., Liang W.-.H., Ou C.-.Q., He J.-.X. Clinical characteristics of coronavirus disease 2019 in China. Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L., Li X., Chen H., Yan S., Li D., Li Y. Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: an Analysis of 116 Hospitalized Patients from Wuhan, China. Am. J. Nephrol. 2020:1–6. doi: 10.1159/000507471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respiratory Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]