Abstract
Objective
To present a low-cost prototype for a barrier enclosure device which can be used during open surgeries such as tracheotomy.
Methods
We provide detailed description of a novel device called COVID-Box, developed by The Surgical Airway Team for COVID-19 Pandemic, a temporary task force formed by Walter Cantídio University Hospital. Safety guidelines for performing tracheotomies in COVID-19 patients are also stated.
Results
Our prototype device provides greater hand mobility than previous barrier devices reported, making it more suitable for airway surgical procedures, such as tracheotomy. The curved shaped format and the customizable access ports provides ergonomics, without compromising safety.
Conclusion
The COVID-Box appears to be an efficient, reproduceable, low-cost barrier enclosure device that can be used for open tracheotomies in ICU patients during the COVID-19 pandemic.
Keywords: COVID-19, SARS-CoV-2, Head and neck surgery, Tracheotomy
1. Introduction
Since December 2019 a number of cases of pneumonia have been reported in Wuhan, China, caused by a novel virus from the coronavirus family [1,2], the SARS-CoV-2 virus. The coronavirus disease 2019 (abbreviated COVID-19), has rapidly swept across the world [3], with the World Health Organization (WHO) declaring it a pandemic on March 11. Since then, the SARS-CoV-2 continues to spread internationally, with 2394,278 of confirmed cases and 164,937 deaths worldwide on April 17 [4]. In Brazil, on the same date, the total confirmed cases were 38,654, with 2462 deceased [4]. In the state of Ceará, located at the northeastern part of Brazil, the more recent official report showed 3306 cases confirmed, with 189 deaths, a mortality rate of 5.7%. That brings Ceará to a preoccupying third place, when comparing other states of Brazil, regarding the number of confirmed cases so far [5].
The main transmission mechanism is via respiratory droplets originated from coughing and sneezing, but aerosol transmission is possible, particularly under the condition of long exposure in a relatively closed environment [2,6]. While respiratory droplets can be spread in a space up to two meters from the source of infection, bioaerosols can travel hundreds of meters [6]. Many procedures involving the airways may generate aerosol, raising the risk of infection of the health care staff [7,8]. Such procedures may include mask ventilation, non-invasive ventilation and tracheotomy [7].
The risk of infection of the health care workers is a major concern. Although head and neck–otolaryngology not being a front-line specialty in dealing with this disease [9], high rates of nosocomial spread were seen amongst otolaryngologists, especially because of the high viral load in the upper respiratory tract [3]. Thus, personal protective equipment (PPE) has become an important subject during the COVID-19 epidemic, which can include fitted high-filtration masks, with its use specially during aerosol generating procedures [10].
Guidelines and recommendations on head and neck evaluation and surgery during the COVID-19 pandemic have been suggested in order to increase safety of health care workers without jeopardizing the care of patients [11]. While the majority of elective surgical head and neck procedures should be postponed, tracheotomy in COVID-19 patients may be considered, especially in patients with prolonged periods of intubation. Tracheotomy is considered a major risk procedure for health care workers, therefore it cannot be overemphasized that barrier precautions are of critical importance [12]. Standard PPEs are essential, but other fundamental aspects include meticulous planning, optimized reduced staff and negative pressure rooms [12].
More recently, a device called “aerosol box” has been suggested to be used as a barrier enclosure during tracheal intubation [13]. It consists of a transparent plastic cube designed to cover a patient's head and that incorporates two circular ports through which the clinician's hands are passed to perform the airway procedure. Despite the fact that it can be easily fabricated, its use for open surgery such as tracheotomy has not yet been reported.
The present work presents a prototype device for a barrier enclosure which can be used during open surgeries such as tracheotomy. This collective protection equipment (CPE) was developed at Walter Cantidio University Hospital at the University of Ceará Medical School, with the purpose of usage at public hospitals in developing countries. We also enumerate some considerations to be performed during tracheotomies in COVID-19 patients.
2. Materials and methods
In this section we describe all steps involved during tracheotomy of COVID-19 patients in our institution, as well as the devices used during the procedure. The barrier enclosure device presented here, called COVID-Box, was developed by the Surgical Airway Team for COVID-19 Pandemic, with collaboration of the Chief Nurse of the Operative Room at Walter Cantidio University Hospital and the Medical Engineering Department of the University of Ceará Medical School. The Surgical Airway Team for COVID-19 Pandemic is a temporary task force formed by Walter Cantidio University Hospital medical staff, consisting of experienced head and neck surgeons, thoracic surgeons and otolaryngologists.
2.1. Setting of surgery and health care staff preparation
The procedure should be performed at bedside in the ICU in order to minimize risks of contamination during transportation. Proper protection of the operative team is paramount during tracheotomy. PPEs for the procedure should include N95 masks, goggles, face shield, surgical gown and double gloves. Surgical team should be limited to two experienced surgeons, with a third person responsible for instrumentation. The removal of the endotracheal tube should be done by ICU staff, also wearing PPEs accordingly.
2.2. COVID-Box description
The COVID-Box consist in two parts: (1) a metallic frame which can be sterilized and (2) a sterile disposable transparent plastic sheet, which is used to cover the metallic structure forming a bottomless box. The latter part consists on a 2 × 2 m transparent polyethylene plastic sheet, with 90 g/m2 grammage. Details of the metallic structure of the COVID-Box are shown in Fig. 1 .
Fig. 1.
COVID-Box metallic frame - structure dimensions.
2.3. Preparation of the patient and surgical field
Patient should have confirmed or suspected COVID-19 disease, and indications of tracheotomy should be accessed by the surgical team. The major indication for tracheotomy is prolonged intubation, for which tracheotomy could be performed up to 21 days after mechanical ventilation has initiated. Tracheotomy before 21 days or other indications should be evaluated individually.
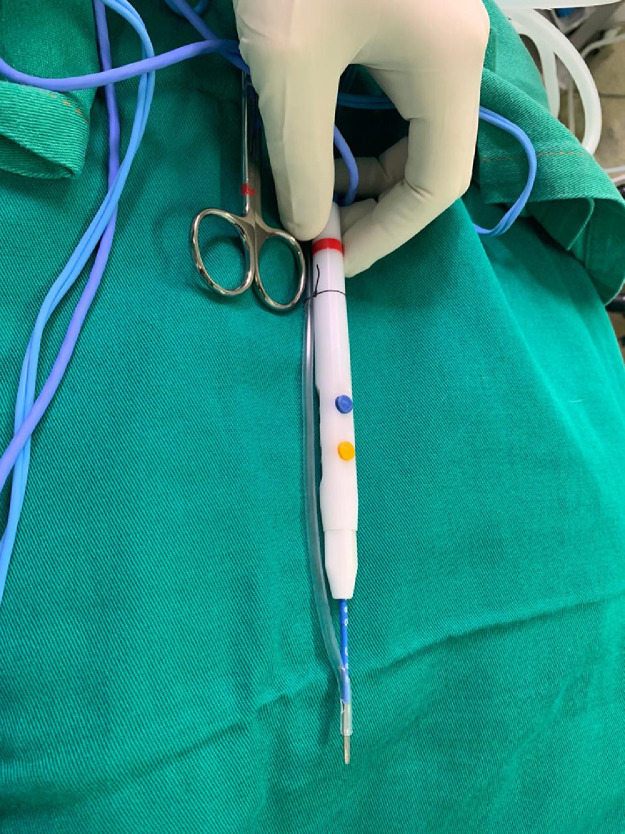
Patient should be adequately positioned in ICU bed, with neck extension when feasible. After skin preparation and positioning of sterile fields, preparation of the COVID-Box follows. Firstly, all suction tubes and electrosurgical equipment are positioned on the top of patient's core, securely placed by towel clamps. We made an adaption on the electrosurgical hand piece, placing the tip of the surgical pencil through a 12Fr disposable PVC suction catheter, in order to continuing aspirate aerosols generated by the electric scalpel (Fig. 2 ). Secondly, the COVID-Box metallic structure (sterilized) is placed on top of the draped patient in the UCI bed, then the sterile plastic sheet is positioned above the metallic structure, forming a box-shaped enclosed device. Sterile towel clamps may be used to tighten up the box outer shape (Fig. 3 a). The access ports on the COVID-Box are then created by cross-shape incisions made at the plastic sheets, two on each side, at the height of surgeon's arms (Fig. 3b). Another extra port should be created on the caudal part of the COVID-Box, which may be used for instrumentation.
Fig. 2.
Adaption on electrosurgical hand piece.
Fig. 3.
(a). Towel clamping. (b). Access port incision making. (c). COVID-Box – head view.
2.4. Intraoperative steps
Patient should be fully paralyzed and adequate sedated throughout the procedure, at the discretion of the intensivist. Minimizing aerosolization during the procedure itself is critical. The use of electrosurgical equipment should be limited to as minimum as possible but must not be used during tracheal incision. Also, ventilation should be paused prior to incision of the trachea [11]. Insertion of tracheotomy tube should be quick, with the cuff immediately inflated and connected to a close circuit, in order to minimize open airway time.
2.5. Postprocedure steps, waste disposal and decontamination
The postprocedure waste disposal and decontamination of equipment need careful consideration to minimize contamination of the environment [12]. Bioaerosols may remain viable in air for up to 3 h [14], therefore removal of the COVID-Box apparatus should be done with caution. After tracheotomy is performed, we recommend leaving the COVID-Box placed on top of the patient for at least 3 h, so it can be removed safely. Even though, extreme care during plastic sheet removal should be taken, with proper disposal afterwards. Drapes, suction tubes, electric scalpel and other disposable items are then removed and discard. The metallic frame of COVID-Box can be sanitized and sterilized for future use. PPE should be worn in the postoperative setting according to the recommendations for enhanced droplet and airborne precautions. It is also recommended to avoid changing the tracheotomy tube until viral load is low or undetectable [11,12].
3. Results and discussion
The COVID-19 pandemic brought new challenges to the medical community. As the disease spreads, the pressure on the global health care work force increases. Health care workers are at high risk of exposure, particularly those who perform procedures within the head and neck region and airway [11]. Moreover, the health system capacity is exceeding its limit, especially in poorer countries, where rationing decisions may need to be made [8,15].
The importance of PPEs during high risk procedures, such as tracheal intubation and tracheotomy, is undoubtable. Although the widespread use of barrier precautions is highly recommended during patients’ care, there is limited availability of N95 masks, respiratory isolation rooms and air-purifying respirators [8]. Such demand is particularly more difficult to manage in a developing country setting. In Brazil, where 74,8% of the population are solely assisted by the public health system, a shortage of ICU beds is expected to occur by the end of April in most major cities [16]. The developing of more affordable strategies to mitigate the spread of the pandemic in such scenarios must be of highest priority.
At our institution with developed an efficient, reproduceable, low cost barrier enclosure device that can be used for open tracheotomies in ICU patients during the COVID-19 pandemic. Its metallic frame is fully autoclavable, as well as the high grammage plastic sheet used to cover it. Different acrylic prototypes have been recommended for use during tracheal intubation [13]. However, restricted hand movement and higher production costs may be a caveat. Also, those devices were not developed for use during surgical procedures. Our prototype, on the other hand, provides greater mobility, since the plastic sheet is more malleable, when comparing to more rigid structures such as acrylic. The metallic frame has also a curved shape on its sides where surgeons can be positioned closer to the patient without compromising safety, therefore preserving ergonomics. Ports are also fully customizable, since they are made by the surgical team right before the beginning of the operation.
There are some limitations of our prototype that need to be addressed. Firstly, the device does not fully enclose the patient. Possible areas of air escape may include the hand ports, as well as the bottom part of the device. Further experiment on aerosol spread while using the COVID-Box is needed, possibly with fluorescent dye [13]. Secondly, the correct time for removal of the device after tracheotomy is uncertain. Previous reports showed that bioaerosols may be in suspension for several hours [6,14]. Therefore, we strongly suggest leaving the box in place after the procedure, removing it only after 3 h or longer. Perhaps, as other airway procedures should be performed after tracheotomy, such as pulmonary toilet, the device might be left positioned for longer periods. Also, a study comparing a regular open tracheotomy and one using the device may be necessary, maybe applying a comprehensive questionnaire to surgeons. Nevertheless, we found that the duration of the operation was not compromised by the use of the apparatus.
Although the COVID-Box was developed for open tracheotomies, other procedures may benefit with the use of the COVID-Box, such as endotracheal intubation, bronchoscopy, upper digestive endoscopy and many others. Some surgical emergencies may also be performed using the device as well, including emergency cricothyroidotomy. Also, cancer patients may have time-sensitive disease with surgical treatments that cannot be postponed for periods longer than a few months. In such cases, we believe that the use of our device could be helpful. Further work should be done to explore the use of COVID-Box for other procedures.
The continuous search for more affordable means of protecting health care workers is highly important. For instance, negative pressure rooms and powered air-purifying respirators are some examples of CPEs that are not always available in many public hospitals in many countries [16]. Thus, the use of barrier devices such as our prototype should be considered to improve collective protection for surgical team during COVID-19 pandemics, especially in the setting of public health institutions in developing countries.
4. Conclusion
The COVID-19 pandemic has spread through the world impacting not only patients, but also health care workers, overwhelming the public health system in many ways. Our institution developed a low cost, reproduceable barrier device that can be used during open tracheotomies in COVID-19 patients. Further tests on efficacy may be necessary.
Acknowledgments
Acknowledgments
The authors would like to thank all staff form Clinical Engineering at Walter Cantidio University Hospital who have helped us building the metallic structure of our prototype device.
Disclosure statement
All authors declare no conflict of interests.
References
- 1.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. NEJM. 2020 Mar 26;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., di Napolli R. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2020. Feature, evaluation and treatment coronavirus (COVID-19) [Internet]https://www.ncbi.nlm.nih.gov/books/NBK554776/?report=classic [cited 2020 Apr 17]. Available from: [PubMed] [Google Scholar]
- 3.Vukkadala N., Qian Z.J., Holsinger F.C., Patel Z.M., Rosenthal E. COVID-19 and the otolaryngologist - preliminary evidence-based review. Laryngoscope. 2020 Mar 26 doi: 10.1002/lary.28672. [DOI] [PubMed] [Google Scholar]
- 4.COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Internet]. 2020 [cited 2020 Apr 18]. Available from:https://coronavirus.jhu.edu/map.html
- 5.Povo R.O. Coronavírus: ceará contabiliza 189 mortes e número de casos confirmados sobe para 3.306 [Internet] J O Povo. 2020 https://www.opovo.com.br/coronavirus/2020/04/19/coronavirus–ceara-contabiliza-19-mortes-em-um-dia-e-numero-de-casos-confirmados-sobe-para-3-108.html [cited 2020 Apr 18] Available from: [Google Scholar]
- 6.Wang J., Du G. COVID-19 may transmit through aerosol. Ir J Med Sci. 2020 Mar 24 doi: 10.1007/s11845-020-02218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook T.M., El-Boghdadly K., McGuire B., McNarry A.F., Patel A., Higgs A. Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia. 2020 Apr 1 doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adams J.G., Walls R.M. Supporting the Health Care Workforce during the COVID-19 Global Epidemic. JAMA Am Med Assoc. 2020 doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 9.Saibene A.M., Allevi F., Biglioli F., Felisati G. Role and management of a head and neck department during the COVID-19 outbreak in Lombardy. Otolaryngol-Head Neck Surg [Internet] 2020 Apr 7 doi: 10.1177/0194599820917914. http://www.ncbi.nlm.nih.gov/pubmed/32255735 Available from: [DOI] [PubMed] [Google Scholar]
- 10.Cook T.M. Personal protective equipment during the COVID-19 pandemic - a narrative review. Anaesthesia. 2020 Apr 4 doi: 10.1111/anae.15071. [DOI] [PubMed] [Google Scholar]
- 11.Givi B., Schiff B.A., Chinn S.B., Clayburgh D., Iyer N.G., Jalisi S. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 Pandemic. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 12.Tay J.K., Khoo M.L.C., Loh W.S. Surgical considerations for tracheostomy during the COVID-19 pandemic: lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg Am Med Assoc. 2020 doi: 10.1001/jamaoto.2020.0764. [DOI] [PubMed] [Google Scholar]
- 13.Canelli R., Connor C.W., Gonzalez M., Nozari A., Ortega R. Barrier enclosure during endotracheal intubation. NEJM. 2020 Apr 3 doi: 10.1056/NEJMc2007589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guzman M.I. Bioaerosol size effect in COVID-19 transmission. Preprints [Internet] 2020 www.preprints.org Available from: [Google Scholar]
- 15.Cavallo J.J., Donoho D.A., Forman H.P. Hospital capacity and operations in the Coronavirus Disease 2019 (COVID-19) Pandemic—Planning for the Nth Patient [Internet] JAMA - Health Forum. 2020 doi: 10.1001/jamahealthforum.2020.0345. https://jamanetwork.com/channels/health-forum/fullarticle/2763353 [cited 2020 Apr 21]. Available from: [DOI] [PubMed] [Google Scholar]
- 16.Castro M.C., Resende De Carvalho L., Chin T., Kahn R., França G.V.A., Macário E.M., et al. Demand for hospitalization services for COVID-19 patients in Brazil. medRxiv [Internet]. 2020; Available from: 10.1101/2020.03.30.20047662. [DOI]