To the Editor: The recent letter by Shah et al1 highlighting the epidemiology of COVID-19 infection and the impact on African American populations captivated our attention. As the world continues to battle this global pandemic, it is important that we acknowledge vulnerable populations and address the needs in these populations to minimize mortality and morbidity. As Shah et al1 noted, ethnic minority groups may have a greater risk of infection due to comorbidities.
In this letter, we want to emphasize the need to assess racial and ethnic disparities in the COVID-19 pandemic and also bring attention to the potential risk of COVID-19 infection in patients with hidradenitis suppurativa (HS). HS is a chronic inflammatory skin condition that disproportionately affects African Americans2 and has several comorbidities that are also risk factors for severe COVID-19 infection.
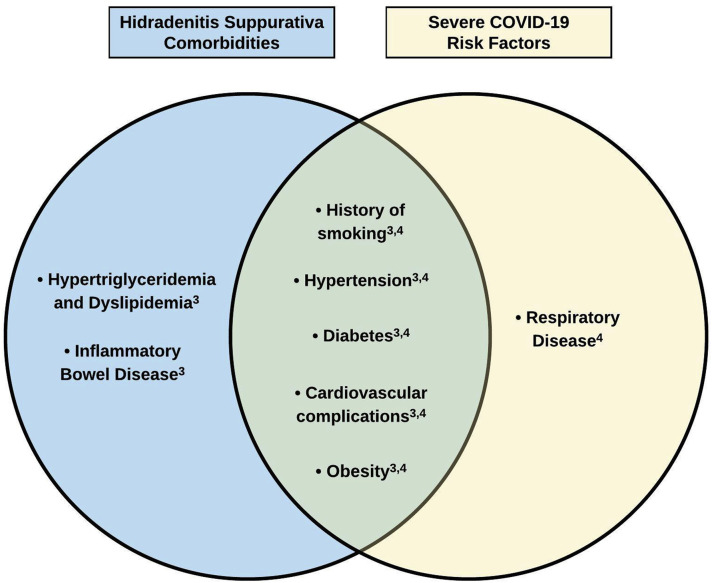
Recent studies have shown that comorbidities associated with HS include smoking history, metabolic syndrome (including hypertension), obesity, cardiovascular complications, hypertriglyceridemia, dyslipidemia, and inflammatory bowel disease.3 Some of these comorbidities, such as smoking and obesity, have even been implicated as risk factors or pathogenic triggers. In addition to COVID-19 infection disproportionately affecting racial and ethnic minorities, emerging data demonstrate that risk factors for severe COVID-19 infection are strikingly similar to HS comorbidities3 , 4 (Fig 1 ). Obesity, cardiovascular conditions, diabetes, hypertension (or metabolic syndrome in HS), and smoking history are all comorbidities or risk factors, or both, in both diseases.3 , 4 In addition, many patients with HS are treated with various immunomodulators or immunosuppressants, and whether immunomodulator or immunosuppressant use increases the risk of severe COVID-19 infection is still unclear.
Fig 1.
Overlap of comorbidities associated with hidradenitis suppurativa and risk factors of severe COVID-19 infection.
Price et al5 recently commented on how immunosuppressant and immunomodulator use in dermatology patients may increase susceptibility, persistence, and possible reactivation of viral infections, especially when broad immunosuppressants across multiple cytokine axes are used. Currently, there is no clear recommendation on withdrawing or modifying immunomodulator or immunosuppressant therapies in patients with HS, but it should be considered when determining the risk of severe COVID-19 infection in patients with both HS and COVID-19 infection.
Our depiction of the comorbidities of HS and the risk factors for severe COVID-19 infection shows a striking overlap. Multiple comorbidities could result in greater challenges in the treatment of patients with HS with COVID-19 infection and may also impact decisions on whether to withdraw or modify current therapy for patients with HS.
The overlapping comorbidities of HS and risk factors for severe COVID-19 infection should highlight the need for patients with HS to exercise caution during this pandemic. Patients with HS should follow guidelines from the Centers for Disease Control and Prevention and should discuss with their dermatologist or general practitioner whether more rigid guidelines for precautions, such as social distancing, are warranted. Whether patients with HS are at a greater risk of contracting COVID-19 or are more likely to develop more severe disease is still unknown, but the substantial overlap in risk factors or comorbidities, or both, is certainly worth further consideration and may warrant counseling of these patients.
Footnotes
Authors Seltzer and Okeke contributed equally.
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
Reprints not available from the authors.
References
- 1.Shah M., Sachdeva M., Dodiuk-Gad R.P. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83(1):e35. doi: 10.1016/j.jaad.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vlassova N., Kuhn D., Okoye G.A. Hidradenitis suppurativa disproportionately affects African Americans: a single-center retrospective analysis. Acta Derm Venereol. 2015;95(8):990–991. doi: 10.2340/00015555-2176. [DOI] [PubMed] [Google Scholar]
- 3.Tzellos T., Zouboulis C.C. Review of comorbidities of hidradenitis suppurativa: implications for daily clinical practice. Dermatol Ther (Heidelb) 2020;10(1):63–71. doi: 10.1007/s13555-020-00354-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng Z., Peng F., Xu B., et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.021. [e-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Price K.N., Frew J.W., Hsiao J.L., Shi V.Y. COVID-19 and immunomodulator/immunosuppressant use in dermatology. J Am Acad Dermatol. 2020;82(5):e173–e175. doi: 10.1016/j.jaad.2020.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]