Abstract
The COVID-19 pandemic is a devastating catastrophe to the whole world, China is the first country seriously affected. This review shows that it is possible to stop wide-spread infection in the country and to provide good quality oncology services even during this challenging period, through concerted efforts with well-organized actions at all levels (National/Municipal, Hospital and Department). The key strategies leading to successful impacts are summarized for sharing. In addition to making practice changes to cope with the adverse realities, oncologists should also work together to raise pragmatic suggestions to policy makers and be strong advocates to protect our patients from the detrimental effect of delay or compromised treatment.
Keywords: COVID-19, Oncology services, Effective strategies
Since the first reported case of the 2019 novel coronavirus disease (COVID-19) in December 2019 in Wuhan City, Hubei Province in China [1], more than 2.07 million people have been invited world-wide (at 17 April 2020). This pandemic is an unprecedented global ‘tsunami’ for health care.
Many cancer centers face the serious challenging reality of having to reduce service provision due to hospital logistic policy, shortage of manpower, and/or fear of infection for staffs and patients. Top oncology experts world-wide have made urgent efforts to publish practice recommendations to provide pragmatic reference for frontline clinicians, the best exemplary guidelines are the ESTRO-ASTRO consensus statements for major cancers [2], [3]. It will be extremely sad if we have to compromise oncology treatment, especially for patients treated with radical intent, the deleterious effects on survival and long-term toxicities may lead to even more life loss than the acute impact by COVID-19. All efforts should be attempted to maintain good quality treatment as far as possible. Sharing of experience to gather collective wisdom is obviously useful.
China is the first country drastically and widely hit by COVID-19, Shenzhen (a city with over 20 million population adjacent to Hong Kong) suffers the same fate. Like all others, our hospital (an affiliated hospital of the University of Hong Kong) struggles to ensure protection of all staffs and patients from COVID-19 contraction; and our Center struggles to maintain comprehensive good quality oncology services (including radiotherapy, systemic therapy and palliative care) during this difficult period. Our experience shows that is achievable with well-organized supports by national/ municipal policies and hospital management, following is a summary of the key strategies and actions at different levels.
Situation of COVID-19 control and oncology services
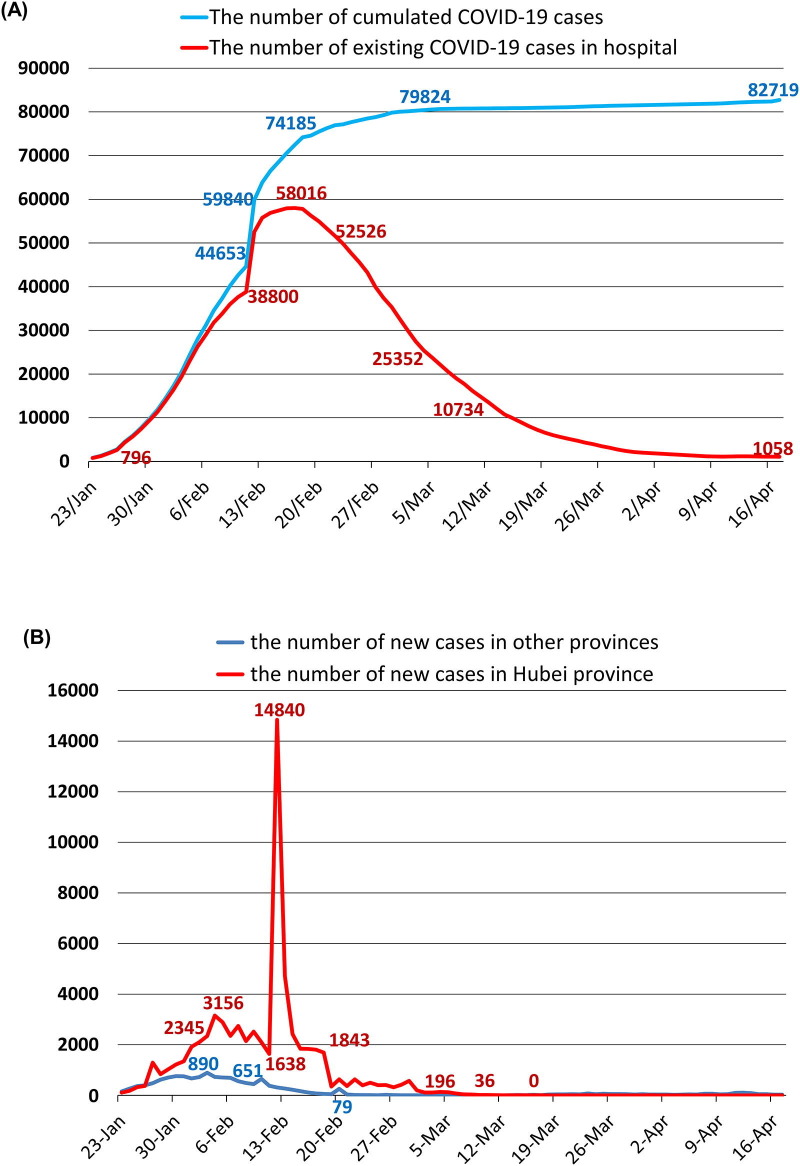
Fig. 1 shows (A) the statistics about COVID-19 infection in the whole of China and (B) the changing pattern of new case detected each day in Hubei as compared with other provinces in China. Of the total of 82,719 patients infected in China, only 17.6% (14,591) occurred outside Hubei. After complete blockade of Wuhan City for 76 days, the strict isolation has been lifted. Furthermore, no new cases were detected in Hubei Province since 3rd April. However, infection control measures are still enforced to stop the risk of new infection by citizens returning from overseas countries and undetected asymptomatic patients in the community. Among the 441 new cases detected in the whole of China during the latest week (11–17 April), only 58 (13.2%) came from local communities, while 383 (86.8%) contracted the virus in other countries.
Fig. 1.
Statistics on COVID-19 epidemics in China (from 23 January to 17 April 2020): (A) Cumulated total number of new cases and existing number in patients in hospital in the whole of China, and (B) the number of new cases detected each day at Hubei Province and the other provinces.
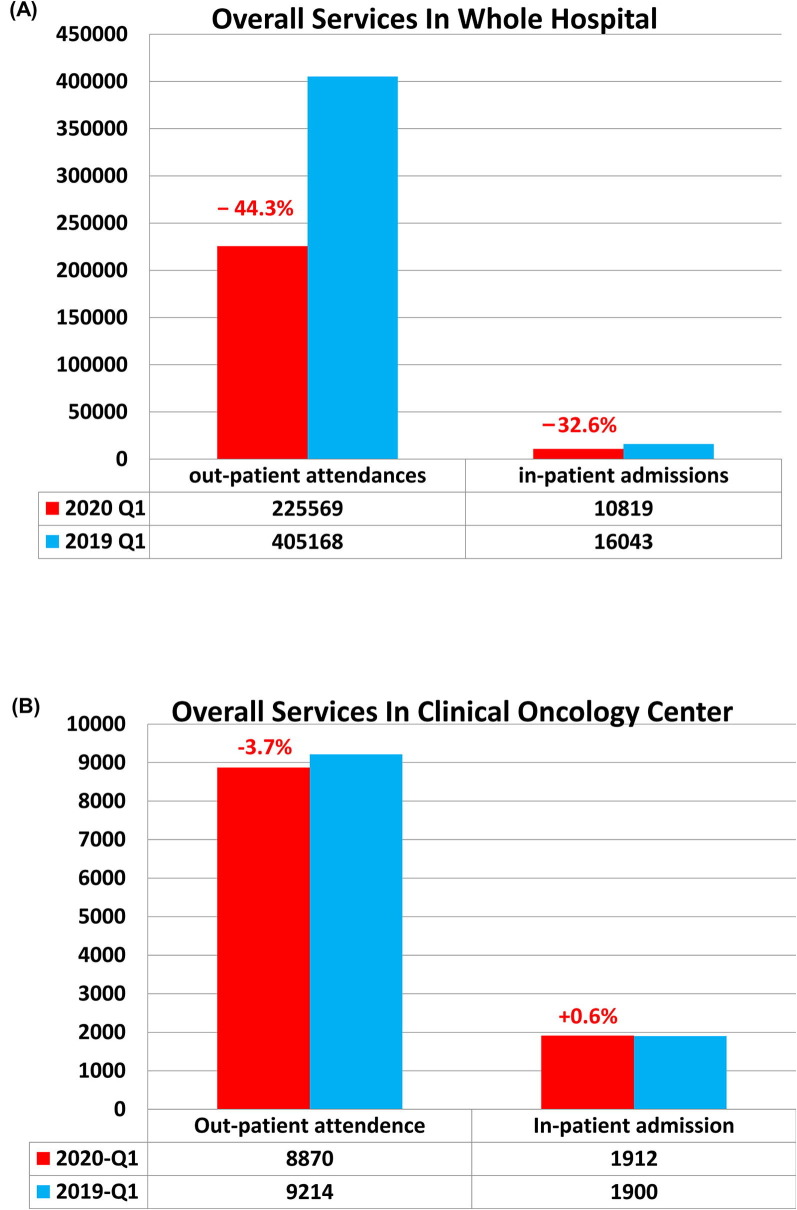
There are 460 confirmed COVID-19 cases in Shenzhen City, Guangdong Province. The first case in Guangdong Province was diagnosed by our hospital on 10 January 2020. Furthermore, our microbiologists were the first to raise serious alert about the high people-to-people contagious rate of this novel virus, as a cluster of 6 members (including children) from the same family were infected [4]. During this period, our hospital had performed 21,138 real time polymerase chain reaction tests (PCR), diagnosed a total of 31 new cases, and provided convalescent care for 101 confirmed COVID-19 patients. Clinical services were inevitably interrupted. During the first quarter (Q1) 2020, the overall out-patient attendances in our hospital dropped by 44.3% and in-patient admissions by 32.6%, as compared with the corresponding quarter 2019 (Fig. 2 A). Fortunately, all patients encountered (a total of 225,569 out-patient attendances and 10,819 in-patient admissions), and all our 3178 staffs have remained free from COVID-19 contraction.
Fig. 2.
Clinical service outputs in terms of out-patient attendances and in-patient admissions during the First Quarter of 2020 as compared with 2019: (A) by the whole University of Hong Kong – Shenzhen Hospital, and (B) the Clinical Oncology Center.
For Clinical Oncology Center, we strived to maintain our services (Fig. 2B). We did not reduce the quota for out-patient appointments, but we encouraged follow-up patients without active diseases to postpone the appointment unless continuation of drug supply is needed, hence the total number of out-patient attendances decreased by 3.7%. For in-patient services, more patients actually requested admission for treatment to minimize the risk incurred by frequent travelling, hence the total number of in-patient admissions even slightly increased (+0.6%). We basically continued to administer systemic therapy (chemotherapy, targeted therapy and/or immunotherapy) in accordance with standard indications.
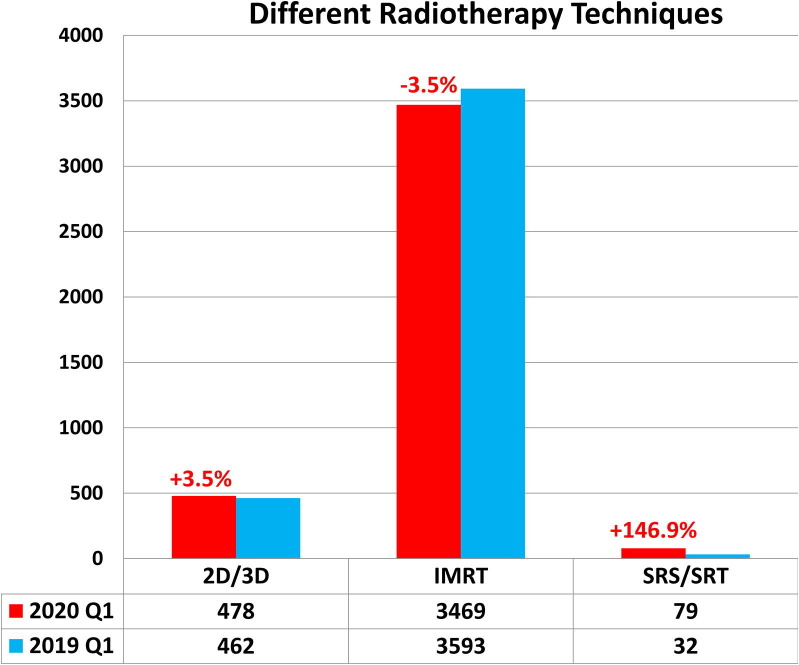
For radiotherapy services, we faced substantial shortage of radiation therapists (15% of manpower) during mid-February to March mainly because of the 14-days quarantine for staffs returning from other provinces after Chinese New Year and the release of pregnant staffs from duties. We had to decrease the number of service hours by linear accelerator from 18 h (6 am to 12 mid-night) to 15.5 h, the median waiting time rose to 45 days at the worst time. Our policy is to give priority to patients treated with radical intent and continue with standard recommendations. With vigorous efforts to increase throughput with available staff and subsequent return of staffs, we managed to maintain radiotherapy outputs – the total number of treatment attendance only decreased by 1.5% in Q1 2020, and the latest median waiting time is 15 days. Furthermore, we managed to maintain high quality radiotherapy without compromise on techniques (Fig. 3 ) and dose fractionation. Altogether, 95% of our patients were irradiated with intensity-modulated radiotherapy (IMRT) or stereotactic radiosurgery/radiotherapy (SRS/SRT); treatment attendance by SRS/SRT even increased in Q1 2020 as compared with 2019 (Fig. 3: +147%). We continued to use optimal fractionation schedule as recommended by international guidelines, but we increasingly changed to single fraction for palliation.
Fig. 3.
The quantity and quality of radiotherapy Service as reflected by the number of treatment attendances by different techniques during the First Quarter of 2020 as compared with 2019: Abbreviations: 2D/3D = 2 dimensional or 3-dimensional conformal, IMRT = intensity-modulated radiotherapy, SRS/SRT = stereotactic radiosurgery or radiotherapy.
Fundamental actions at 3-levels
The prerequisite for providing good quality oncology services during the raging COVID-19 pandemic is a reassuring safe environment for patients and staffs. How does China, Shenzhen, our Hospital and our Center manage to achieve the current control and service provision? Following are the hard lessons that we have learnt and the key strategies/actions at different levels that made effective impact.
National/Municipal government
The fundamental strategy is prevention, early detection, immediate effective isolation and appropriate supportive treatment.
The decisive action by the Central Government, People’s Republic of China (PRC) to order complete blockade of Wuhan City on 23 January and then the whole Hubei Province shortly afterwards was a critical step to prevent the spread of the disease to the rest of the countries. Not only is the cumulated number of COVID-19 patients substantially lower in other provinces, the drop in new cases occurred much earlier (Fig. 1B).
The national message is that every citizen has an important role to play in this war against COVID-19: health workers fighting to save life at the frontline, while common folks must try their best to avoid contracting the virus. In addition to emphasis on personal hygiene and protection by facial masks in crowded areas, there are immediate policies on stopping schools, entertainment/non-essential services and enforcing social distancing. All residential communities and the primary health doctors are responsible to monitor the health status of their local residents; in the unfortunate event of resident diagnosed with COVID-19, the whole residential block and all related contacts will be immediately quarantined for medical observation for 14 days.
The importance of early detection cannot be over-emphasized. Diagnostic PCR test is extensively provided to screen all high-risk cohorts and patients requiring admission and/or aerosol-generating procedures. The government instructions have been repeatedly updated in accordance with the changing need and the recognition of new risks. The key indicators include: (1) all patients with suspicious fever/respiratory symptoms; (2) travel history to any foreign countries, outside regions (including Hong Kong, Macau, Taiwan), Hubei province or any other community infected with COVID-19; and (3) contact with confirmed or asymptomatic COVID-19 patient in the past 2 weeks.
Early hospitalization of confirmed cases is important. We learnt the bitter lesson at Wuhan when patients were asked to stay at home as there were not enough hospital beds at the beginning of the outbreak. This resulted in rapid surge of cross-infection. Effective rectification by installing more than 16 hospitals with 12,000 beds was implemented within 10 days. Although very few hospitals have ideally equipped wards with negative pressure and HEPA filter, a well-ventilated environment is provided for isolation of patients under proper care by health care professionals.
Central assignment of responsibility to different hospitals, basing on available infrastructure and expertise, is another effective step. All confirmed cases are treated in COVID-19 designated hospitals, allowing the other hospitals to continue essential medical services for non-infected patients. The COVID-19 designated hospitals are basically divided into 3 categories – (A) entire hospital for patients with severe symptoms needing intensive care, (B) entire hospital for patients with mild symptoms, and (C) other hospitals with designated isolation wards for recovering patients. This arrangement allows cost-effective assignment of health care workers and rapid accumulation of knowledge.
To provide the rapid increase in manpower needed, central coordination for deploying the required expertise is needed. Over 42,000 health care workers from different provinces have been thus deployed to Hubei Province during the peak period. There is a touching spirit of volunteerism all over China.
Another crucial government policy to ensure full compliance with early detection and hospitalization (if infected) is the waiving of medical expenses on COVID-19 related investigations and treatment. Although 90% of citizens in major Chinese cities are covered by medical insurance, a huge population are inadequately covered. Without such financial assurance, under-privileged suspects/patients may decline the recommended investigations/treatment, seriously affecting the attempts for early isolation.
Hospital management
As a designated hospital responsible for convalescent care of COVID-19 patients and screening of foreign citizens/visitors, special measures are implemented to ensure safety for all staffs and patients, while continuing to provide essential clinical services as far as we can.
For early detection and isolation, 3-check screening has been implemented. First check is set at the hospital entrance – all patients/visitors have to complete a health declaration form (on symptoms, travelling history and contacts), provide contact information and to take body temperature. Patients with both symptom(s) and travelling/contact risk will be escorted to a designated Fever Clinic for exclusion of COVID-19. Patients with either symptom(s) or travelling/contact risk will be escorted to the second check-point where a more detailed history will be taken by a medical doctor to decide whether PCR screening should be performed before patients can proceed to the clinical areas. Temperature check will be repeated at entrance to the Out-Patient Clinic Block and the In-Patient Ward Blocks. The third check is carried out by attending doctor of respective specialty, a Health-Check Form (Part A on history declared by patient and Part B on cross-checking by doctor) will be completed for filing in the medical record. All visitors with suspicious health item(s) will be declined entry to clinical areas.
To ensure cost-effective use of protective gears, clinical areas/procedures are categorized into 3 risk-groups for allocation of gears (Fig. 4 ) in line with the government instructions [5]. Close monitoring is important to ensure adequate stock for all staffs; distribution to individual staffs is regulated to ensure fair supply without inappropriate wastage. Vigorous efforts had been made to source available supplies from other countries at time when China is the only country seriously affected. During the most difficult time when the stock of protective gear was running low and the infection rate in Shenzhen was rising, we had to close departments with high risk and/or high consumption of gears. However, even at the most difficult period, our hospital policy is to continue clinical services for which delay may seriously affect patient survival; priority supports are hence provided for emergency treatment, oncology and obstetrics.
Fig. 4.
Protective gears for clinical areas & procedures with different risk. Abbreviation: AGP = Aerosol-Generating Procedures.
All staffs have to report health status electronically every day. Any staff with abnormal symptoms will be assessed by the Infection Control Team. All staffs who have travelled outside Shenzhen have to be screened by PCR test before returning to work. At the peak infection period, the staff canteen was closed and free meals prepared by the hospital kitchen were delivered to individual staffs at respective work places. Even with recent re-opening of the canteen, dining tables are re-arranged to ensure adequate free space and to minimize face-to-face contact. Group meetings are now conducted mostly in open well-ventilated areas.
Meticulous care is to cordon off high-risk areas (Fever Clinic/Observation Ward and the designated Isolation Wards for COVID-19 patients in convalescence) from public access. Environmental cleanliness with frequent disinfection of all public areas and checking of sewage drainage pipes are strictly supervised.
Department management
With the support by the hospital and all the safety measures in place, the only time when the department had to make painful decision on prioritization of treatment was the period of manpower shortage as described above. Close communication with patients by phone is implemented to encourage patients treated with radical intent to commence/continue treatment and those with disseminated disease but mild symptoms to postpone appointments. This extra step helps to identity patients who intend to default treatment, so that the relieved radiotherapy slots could be used for other patients.
Strict compliance with all the government and the hospital policies are demanded. All staffs are well-trained on diagnosis of suspected cases and proper use of protective gears. Visitors are stringently cross-checked to minimize any risk.
Another unique difficulty faced by our department is the border restriction with 14-days mandatory quarantine for staffs returning to Hong Kong from Shenzhen. The clinical staffs from the University of Hong Kong have to be split into 2 teams, 1–2 professoriate staffs will continue to attend on-site at Shenzhen, while the remaining colleagues provide remote support from Hong Kong. Telemedicine is increasingly used, so all staffs could still continue to lead their respective subspecialty services (including radiotherapy planning).
Conclusions
The COVID-19 pandemic is a devastating catastrophe to the whole world. However, this war against COVID-19 can be won soon if we all learn from each other and work together. Our experience shows that it is possible and safe to provide good quality oncology services even during this challenging period. The required prerequisite is a safe environment for both patients and staffs. This will not be possible without well-organized strategies/actions at all levels (National/Municipal, Hospital and Department). Efforts by oncologists alone to cope with the gross adversities is inadequate to protect our patients from the detrimental effect of delay or compromised treatment. Together we can raise pragmatic suggestions for policy makers and be strong advocates to achieve the common goal of saving more lives.
Declaration of competing interest
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the points reported in this paper.
Funding/Support
None.
Footnotes
The Editors of the Journal, the Publisher and the European Society for Radiotherapy and Oncology (ESTRO) cannot take responsibility for the statements or opinions expressed by the authors of these articles. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. For more information see the editorial “Radiotherapy & Oncology during the COVID-19 pandemic”, Vol. 146, 2020.
References
- 1.Y Cheng, P Hu, Q Huang, et al. Practical strategies for medical staff in large general hospitals during the outbreak of novel coronavirus pneumonia. Chongqing Medicine. http://kns.cnki.net/kcms/detail/50.1097.R.20200325.1245.004.html.
- 2.Guckenberger M, Belka C, Bezjak A, et al. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus statement. Radiother Oncol (in press). [DOI] [PMC free article] [PubMed]
- 3.Thomson DJ, Palma D, Guckenberger M, et al. Practice recommendations for risk-adapted head and neck cancer radiotherapy during the COVID-19 pandemic: an ASTRO-ESTRO consensus statement. Int J. Radiat Oncol Bio Phys (in press). [DOI] [PMC free article] [PubMed]
- 4.Chan J.F.W., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2019;2020 doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The National Health Commission of the People’s Republic of China. The guideline on medical protective gear in the prevention and control of COVID-19. http://www.nhc.gov.cn/yzygj/s7659/202001/e71c5de925a64eafbe1ce790debab5c6.shtml. [DOI] [PMC free article] [PubMed]