Abstract
A novel technique of cultivating autologous blood with gold particles; then separating the gold particles and cells from the serum and injecting the conditioned serum into affected plantar fascia. A first-time report of the safety and efficacy in treatment of recalcitrant plantar fasciosis in an Olympic equestrian. A single patient with clinical signs, symptoms and ultrasound evidence of plantar fasciosis was treated with four intra-ligamentous GOLDIC® injection therapy. The Olympic jumper was evaluated by Visual Analog Scale (VAS), Foot and Ankle Disability Index (FADI), and Global Rating of Change (GRoC) score(s) before injection and at 6-month follow-up. VAS, FADI, and GRoC scores showed substantial and marked improvement clinically. The subject was able to return to sport without limitations after 8 weeks. The initial result demonstrates that the treatment regimen is safe, and efficacious. The subject demonstrated reduction of pain, and improved function that allowed return to high level competition.
Keywords: Plantar fasciitis, Goldic, Intra-ligamentous injection, Pain Relief, Functional Score, PRP, ACS, Regenokine, Orthokine, ACP, Injections, Regenerative medicine, Pain management, Translational medical research, Humans, Fascia pathology, Fascia injuries, Fasciitis. Plantar/etiology, Fasciitis. Plantar/physiopathology
Introduction
The pain located in the plantar aspect of the heel, known as “plantar fasciitis” is one of the most common disorders that cause plantar heel pain [1] and it usually is defined as inflammation of the plantar fascia at its insertion; however, today, we know that there are cases that do not show an evident inflammatory response. A histopathological study has found no cellular signs of inflammation in such cases, but a failed healing response in the structure of the plantar fascia [2] aptly named “plantar fasciosis.”
The prevalence of the plantar fasciosis has not yet been reported, but is estimated that it may affect as much as 10% of the general population at some point [3]. Specific injuries in equestrian athletes are more rarely reported, and the literature demonstrates a paucity of data concerning the prevalence and incidence of plantar fasciitis/fasciosis. It is well established that the leading mechanism of injury in this discipline is falling from the horse, closely followed by being kicked by the horse. Joints are the less frequently injured, accounting for only 0.3%, and up to 7% of injuries. Fractures represent 33.6% of the cases, with more than half involving upper extremities (50.7%), followed by lower limb injuries (22.9%), spine, torso and pelvis [4, 5].
The lack of a consistent nomenclature and accurate definition is probably because the etiology and pathogenesis are not entirely understood [6]; however, it is known that the plantar fasciosis has multifactorial pathology, influenced by both intrinsic and extrinsic risk factors [1, 7]. Case–control studies [8] have demonstrated decreased ankle dorsal flexion, high body mass index, pronated foot posture, and prolonged weight-bearing as independent risk factors for plantar fasciosis. Despite the lack of data of prevalence and incidence of plantar fasciosis among equestrian athletes, we understand that this condition is not common in this discipline and the causes are likely related to an overloading of the whole Achilleo-calcaneal-plantar complex as well as repetitive microtrauma caused by the permanent vibration while in the stirrup. An underlying anatomic/mechanical impairment may also be a possible predisposing factor.
The most common clinical finding is a pain in the plantar aspect of the affected heel, localized to the medial tubercle of the calcaneus [7]. Patients report an exacerbation of pain following resting periods or non-weight-bearing; for example, first steps after waking up from bed that decreases after few steps of initial weight-bearing. Some patients also report increased pain with increased physical activity [1, 9].
Most cases can be managed conservatively, with a very high rate of resolution of symptoms of up to 90% [10]; however, there is no clear consensus about protocols, treatment or strategies for plantar fasciosis.
Case History
Presentation of a 32-year-old female, former Olympic, and current World and Nation’s Cup(s) jumping equestrian who suffered from plantar heel pain for 2 years. Symptoms became worse after fall from the saddle some 9 months previously. The patient reports continuous pain that increases in the morning upon waking, during training, and in the evening after training. The pain was present in both feet previously, but the right sided pain subsided with conservative therapy consisting of manual techniques, eccentric training, stretching of the dorsal muscles of the calf, and orthotics placed in the riding boots. The left foot did not respond. The pain was in the medial plantar left heel, and also mildly under the great toe. She dons riding boots or flip-flops, and uses a custom orthotic in her riding boots.
Clinical examination revealed a slight over-pronation of the right foot, the subtalar axis was displaced medially. Mild supination was noted in the left foot, with the subtalar axis slightly lateralized. Radiographs of the bilateral feet were normal. MRI of the foot demonstrated a small effusion in the left peroneus longus and tibialis posterior tendon sheaths. Ultrasound examination revealed non-homogeneous echogenicity in both plantar fasciae, compatible signs of fascial degeneration, and hypoechogenicity on both fascial insertions, but more prominent on the left side, that suggested a chronic plantar fasciosis, Figs. 1 and 2. Both plantar fascia thickness were considered within average values.
Fig. 1.

Ultrasound image pretreatment of right foot plantar fascia
Fig. 2.
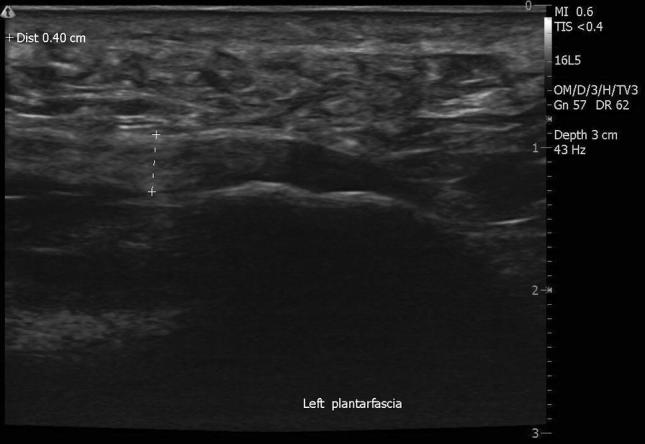
Ultrasound image of pretreatment of left foot plantar fascia
Prior to treatment, the patient was evaluated with 100.00 mm visual analog scale (VAS), Foot and Ankle Disability Index (FADI) at baseline, 6 months, and Global Rating of Change (GRoC) at 6-month follow-up, Table 1. The VAS is a measurement instrument that tries to measure pain range across a continuum of values and cannot easily be directly measured, and in this case perceived pain. The FADI assesses functional limitations related to foot and ankle conditions such as ankle instability and other hind foot conditions. It consists of 26 questions answered by the subject, with a minimum score of 0 points indicating severe disability, to 100 points indicating no disability. The GRoC is a frequently used outcome measure that has been used to independently score self-perceived improvement in a patient and has been used as an anchor method to determine minimal clinically important change scores. The score can range from (− 7) a very great deal worse, to (7) a very great deal better and has 1 question.
Table 1.
GRoC, VAS, and FADI scores before and after GOLDIC Injection (6-month follow-up)
| GRoCa | VASb (mm) | FADIc | |
|---|---|---|---|
| Pre-GOLDIC | n/a | 60.98 | 60.6 |
| Post-GOLDIC | |||
| 6 months | 6 | 14.16 | 91.93 |
Pre-GOLDIC Pre- Gold Induced Cytokines, GRoC Global Rating of Change, VAS Visual Analogue Scale, FADI Foot Ankle Disability Score
aGROC scales ask that a person assess his or her current health status, recall that status at a previous time-point, and then calculate the difference between the two The magnitude of this difference is then scored on a numerical or visual analogue scale. Such scales have been recommended for use as a core outcome measure for chronic pain trials
bVAS: A horizontal line, 100 mm in length) the patient marks on the line the point that they feel represents their perception of their current state of pain
cFADI: FADI consists of 26 questions in two domains; Function, and Pain. Standardized answer options are given (5 Likert boxes) and each question gets a score from 0 to 4. A normalized score (100 indicating no symptoms and 0 indicating extreme symptoms) is calculated for each domain. The result can be plotted as an outcome profile
GOLDIC protocol treatment was proposed and carried out, by performing one series of ultrasound-guided injections in the left plantar fascia origin, with completion of the four injections every other day for 8 days. The first injection was carried out Monday, November 27th, 2017 followed by additional injections as prescribed on November 29th, December 2nd, and finally December 4th 2017. The volume injected was a constant 3.0 cc of autologous conditioned serum in every session for the left foot, using 1.5 in. 25 gauge needle with ultrasound guidance with 16L5 Smart Mark high frequency linear probe, uSmart 3200T, in the longitudinal axis (Terason Inc, Burlington, Massachusetts, USA) with ethylchloride spray cutaneous anesthetic (Walter Ritter GmbH, Hamburg, Germany) performed in the lateral decubitus position with the right side up using gel pad to support, protect, and elevate the lateral malleolus of the left ankle. All injections were tolerated by the patient very well, who was able to depart from the clinic walking immediately without difficulty. No complications of any kind were seen during or after the treatment.
Patient returned to competition 8 weeks after completion of treatment. At final 6-month follow-up, symptoms had largely abated and patient was without limitation, and no further treatment was required.
Discussion
Plantar fasciosis among equestrian athletes is not frequently reported; however, when it occurs it can be even more difficult to manage than in other sports due to the special mechanical and physical requirements and characteristics of horse-riding [11]. This could lead to poor clinical outcomes when applying common treatments as it occurred in the current case being presented. Twenty-eight different conservative modalities and eight different surgical treatments have been described, that could suggest the lack of a concrete solution treating this condition [12]. Combination of different modalities are most commonly applied [8], for example, using a custom-made insole to compensate for a structural-biomechanical foot impairment such as overpronation or utilizing extracorporeal shockwave therapy (ECSWT) [13].
Another widely used treatment for this condition is corticosteroid injections [14]. Randomized controlled trials have demonstrated efficacy in providing fast pain relief [14]; however, there are a number of limitations with this treatment such as the duration of the pain relief and possible complications reported, such as heel pad atrophy and rupture of the plantar fascia [14].
Autologous blood-derived products (ABPs) have also been reported for plantar fascia pathology treatment. A systematic review [14] demonstrated positive outcomes as compared to corticosteroids, and ECWST; finding ABPs just as effective in providing pain relief at 3 months; however, equivalence of ABPs and ECSWT at 6 months, with both modalities superior to corticosteroids.
We have developed a new technique of generating a conditioned serum rich in cytokines (Gold-IC) by utilizing specialized gold particles. The first human clinical trial [15] studied the healing of Achilles tendinopathy, that demonstrated promising MRI and clinical follow-up results. Compared to other blood-based biological methods, only the gold induced cytokine (GOLDIC®) procedure has demonstrated upregulation of plasma gelsolin (pGSN) and granulocyte colony stimulation factor (G-CSF) and both play an important role in tissue regeneration [12]. Considering that plantar fasciosis is a condition of failed healing response, we believe that a regenerative treatment like GOLDIC can provide positive and lasting results.
Acknowledgements
Pam Jackson, Ph.D., for manuscript review.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sergio Nicolas Sardon Melo and William D. Murrell equally contributors.
References
- 1.Singh D, Angel J, Bentley G, Trevino SG. Fortnightly review: plantar fasciitis. BMJ. 1997;19(315):172–175. doi: 10.1136/bmj.315.7101.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (Fasciosis) without inflammation. Journal of the American Podiatric Medical Association. 2003;93:234–237. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 3.DeMaio M, Paine R, Mangine RE, Drez D. Plantar fasciitis. Orthopedics. 1993;16:1153–1163. doi: 10.3928/0147-7447-19931001-13. [DOI] [PubMed] [Google Scholar]
- 4.Young JD, Gelbs JC, Zhu DS, Gallacher SE, Sutton KM, Blaine TA. Orthopaedic injuries in equestrian sports: a current concepts review. Orthopaedic Journal of Sports Medicine. 2015;3:1–7. doi: 10.1177/2325967115603924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCrory P, Turner M. Equestrian injuries, in epidemiology of pediatric sports injuries Individual Sports. In: Caine DJ, Maffulli N, editors. Med Sport Sci. Basel: Karger; 2005. pp. 8–17. [Google Scholar]
- 6.Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP. The pathomechanics of plantar fasciitis. Sport Medicine. 2006;36:585–611. doi: 10.2165/00007256-200636070-00004. [DOI] [PubMed] [Google Scholar]
- 7.Rome K. Anthropometric and biomechanical risk factors in the development of plantar heel pain—a review of the literature. Physical Therapy Reviews. 1997;2:123–134. doi: 10.1179/ptr.1997.2.3.123. [DOI] [Google Scholar]
- 8.Irving DB, Cook JL, Young MA, Menz HB. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskeletal Disorders. 2007;17(8):41. doi: 10.1186/1471-2474-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schepsis AA, Leach RE, Gorzyca J. Plantar fasciitis: etiology, treatment, surgical results, and review of the literature. Clinical Orthopaedics and Related Research. 1991;266:185–196. [PubMed] [Google Scholar]
- 10.Gill LH. Plantar fasciitis: diagnosis and conservative management. Journal of American Academy of Orthopaedic Surgeons. 1997;5:109–117. doi: 10.5435/00124635-199703000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Pugh TJ, Bolin D. Overuse injuries in equestrian athletes. Current Sports Medicine Reports. 2004;3:297–303. doi: 10.1007/s11932-996-0003-6. [DOI] [PubMed] [Google Scholar]
- 12.Atkins D, Crawford F, Edwards J, Lambert M. A systematic review of treatments for the painful heel. Rheumatology. 1999;38:968–973. doi: 10.1093/rheumatology/38.10.968. [DOI] [PubMed] [Google Scholar]
- 13.Rompe JD, Furia J, Weil L, Maffulli N. Shock wave therapy for chronic plantar fasciopathy. British Medical Bulletin. 2007;81–82:183–208. doi: 10.1093/bmb/ldm005. [DOI] [PubMed] [Google Scholar]
- 14.Hsiao MY, Hung CY, Chang KV, Chien KL, Tu YK, Wang TG. Comparative effectiveness of autologous blood-derived products, shock-wave therapy and corticosteroids for treatment of plantar fasciitis: a network meta-analysis. Rheumatology. 2015;54:1735–1743. doi: 10.1093/rheumatology/kev010. [DOI] [PubMed] [Google Scholar]
- 15.Schneider U, Wallich R, Felmet G, Murrell WD. Gold-induced autologous cytokine treatment in Achilles tendinopathy. In: Canata G, d'Hooghe P, Hunt K, editors. Muscle and Tendon Injuries. Berlin, Heidelberg: Springer; 2017. [Google Scholar]


