Abstract
Background
There is evidence that early return to competition post-anterior cruciate ligament (ACL) injury increases risk of re-injury.
Aims
To compare subsequent ACL and other injury risks following ACL reconstruction for Australian Football League (AFL) players returning to competition at different times post-injury.
Methods
AFL players returning from ACL reconstruction in the 1992–2014 seasons were divided into three groups based on return to competition time (< 10, 10–12 and > 12 months). Non-reconstructed injuries and artificial ligament reconstructions were excluded. Subsequent ACL injury rates were calculated based on time since injury and number of return matches played. Risk of other knee and hamstring muscle injuries was also calculated.
Results
There were 233 ACL reconstructions that returned to play in the AFL during the time period under study and met our inclusion criteria. The per-game risk of subsequent ACL injury decreased with a log decay from 1.2 to 0.15% during the first 20 games back (R2 = 0.43). Players returning at > 12 months had higher overall percentage of future career games missed through subsequent ACL injuries (4.8% vs. 2.4%), and through all hamstring and knee injuries combined (12.6% vs. 8.4%) than players who returned at ≤ 12 months (both P < 0.001). Players returning at > 12 months had higher risk of knee cartilage (3.7%) and patella tendon (0.6%) injury than those returning at 10–12 months (1.5%, 0.1%, respectively).
Conclusion
Players returning from ACL reconstruction at greater than 12 months had significantly higher rates of future games missed through both subsequent ACL injuries and through all hamstring and knee injuries combined. It may be true that both early and late return to play lead to suboptimal outcomes compared to average return-to-play times.
Keywords: Anterior cruciate ligament, Return to play, Subsequent injury, Reconstruction
Introduction
Anterior cruciate ligament (ACL) injuries are a common significant injury in Australian footballers [1, 2] and other elite sports [3–6]. ACL injury is second only to hamstring muscle strain injuries as a cause for missed game time in the Australian Football League (AFL) [7].
Return to sport following surgical management of an ACL injury is an important topic in sports medicine and orthopaedic literature [8]; however, the optimal time to return to elite sport following ACL reconstruction remains controversial [9, 10]. In their ACL return-to-sport guidelines, Davies et al. [8] describe the timing of return to sport following ACL reconstruction as ‘one of the most challenging, complex and difficult decisions that may be made by a sports medicine team.’
Return-to-play guidelines for elite athletes following ACL reconstruction often suggest recommended times well under 9 months [9–11]. In an expert opinion survey, a panel of experienced orthopaedic surgeons recommends a period as short as 6–8 months as a return-to-play time for an elite athlete [12]. There is a trend in the literature towards combining completion of functional outcome measures with minimum time frame (post-surgery) as the requirements to clear for return to play [8, 13]. The BJSM guidelines on return to sport following ACL injury describe minimum time to return to play as ‘the standard by which orthopaedic surgeons measure themselves and are measured in sports circles’ [11].
Despite these recommendations, in reality, return-to-play times following ACL reconstruction are variable and differ between sports. A systematic review of 15 studies documenting elite athletes’ return to sport following ACL reconstruction found mean return-to-play times between 6 and 13 months [4].
Multiple studies have provided commentary and guidelines on optimal recovery timeframes post-ACL reconstruction, as well as functional performance measures to facilitate the best outcome upon return to play [4, 8, 11, 14]. However, the only study to quantify the relative risks associated with return to play at different times is that of Grindem et al. This study was a prospective cohort of 106 patients and showed that the risk of ACL injury recurrence is highest with rapid return and continues to fall until return times of 9 months or greater [15].
The aim of this study is to compare outcomes, including risk of ACL re-injury and risk of other subsequent lower limb injury and subsequent career length, for Australian Footballers returning to elite sport at different times post-ACL reconstruction.
Materials and Methods
Data Extraction from AFL Injury Database
Data were obtained from the AFL injury surveillance database, whereby AFL medical staff for all teams prospectively collect all player week exposures during the active season [16]. This database compiles data for each unique player, including match exposures and injury data (pertaining to any illness or injury which resulted in a player missing a game). Thus, this study is a retrospective analysis of prospectively collected injury data documenting all player match exposures in the AFL.
Data Selection: Inclusion and Exclusion Criteria
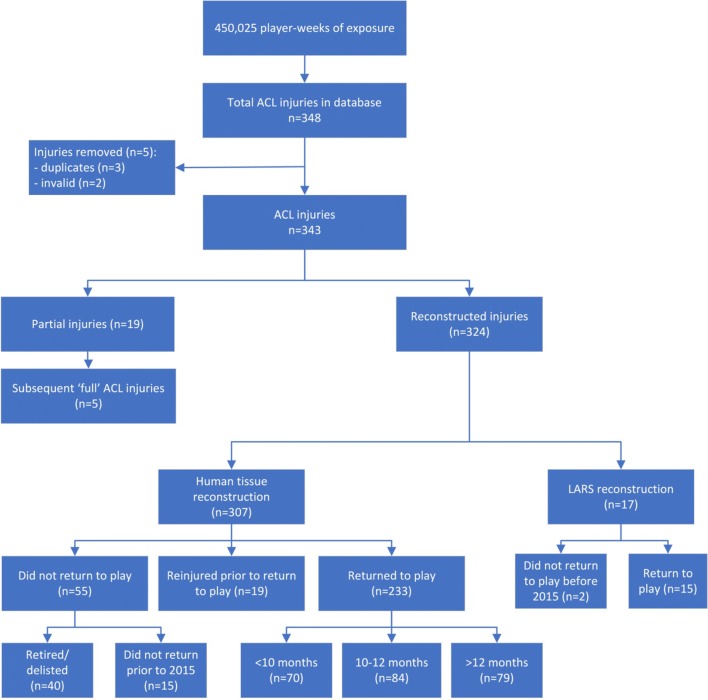
The defined cohort was players who sustained ACL injuries between 1992 and 2014 inclusive, whose injuries were treated with a human tissue reconstruction and then returned to play matches (without further ACL injury prior to return to play) whilst still listed as an AFL player (Fig. 1).
Fig. 1.
Flowchart of all ACL injuries identified in AFL injury database
All injury data for seasons between 1992 and 2014 inclusive were extracted, this timeframe chosen as these were the seasons during which author JWO was the AFL injury surveillance coordinator. All instances of ACL injury during this timeframe were categorised as either initial or subsequent ACL injury (compromising both ipsilateral recurrences and contralateral injuries). Injuries were also categorised as a partial injury or a complete rupture (necessitating ACL reconstruction) and in the surgically managed cases, whether this was a human tissue reconstruction or artificial ligament repair. There was insufficient detail in the database to extract the specific graft choice (i.e. patella tendon vs. hamstring tendon graft).
Partial ACL injuries, where ACL reconstruction was not performed, and reconstructions that were performed using artificial ligaments were excluded from our return-to-sport analysis as these are now known to lead to both early return to play and to have an especially high re-rupture rate [1, 17]. The remaining human tissue reconstruction injuries were split initially into three groups: players who did not return to play whilst AFL-listed, players who were re-injured with a further ACL injury prior to return to play and players who returned to play without further ACL injury. The players who returned to play (coded as having participated in an AFL or other competitive fixture) were the focus of this study.
Duplicates in the database were identified based on the date of injury. In instances where a subsequent ACL injury was recorded within 8 weeks of the primary ACL injury, it was reviewed for the possibility of being a duplicate injury. There were two injuries that were extracted as they missed games in 1992 but then excluded as the injuries were sustained in 1991.
Data Analysis
All players returning from ACL reconstruction who met the inclusion criteria (players with ACL injuries who returned to play following human tissue reconstruction) were divided into three groups based on the time to return to their first competition match after ACL injury. The groups were: players returning in less than 10 months, returning at between 10 and 12 months and returning at greater than 12 months. These cut-off months were chosen to give three groups of roughly equal size.
Data analysis and injury recurrence risk calculations were performed using the Access and Excel programs, 2010 versions (Microsoft, Seattle USA). Comparisons between groups were also done using 2 × 2 contingency tables (GraphPad Prism v7.04, California USA). For correlation coefficients, we used the Evans classification to categorise the relationships as either weak, moderate or strong [18]. The rates of subsequent ACL injury were calculated based on: (1) the time in days since the original injury and (2) the number of return matches played since the injury. The risk of further ACL injury and other lower limb injury per further game were also calculated for each of the three groups. Subsequent time loss injury following ACL reconstruction was analysed for those lower limb injury types considered possibly related to ACL injury, including hamstring muscle strains and other (non-ACL) knee injuries (e.g. cartilage injury, patella tendon injury and patella fracture). The career length subsequent to ACL reconstruction was also measured as an average of the total number of subsequent games played following ACL reconstruction for each of the three return-to-play groups.
Outcomes
The primary outcome was subsequent ACL injuries (either recurrent ipsilateral or contralateral) when comparing the three return-to-play groups.
The major secondary outcomes were risk of subsequent other injuries to hamstring muscles or non-ACL knee structures in the three groups.
Results
Data were extracted for 4871 unique players, participating in a total of 450,025 player weeks during the 23 seasons analysed. Of 348 ACL injuries in the database, five ACL injuries were eliminated from analysis due to being duplicates or invalid (pre-1992 injuries). There were 343 unique ACL injuries identified with match exposure of 322,136 player matches [202,184 AFL player matches and 119,952 ‘other’ (non-AFL) competitive fixtures].
Of the 343 ACL injuries, 19 injuries were found to be ‘partial’ ACL strains (not necessitating graft reconstruction) and were excluded from the analysis. Seventeen synthetic tissue reconstructions using the Ligament Augmentation Reconstruction System (LARS) were excluded, leaving a total of 307 human tissue ACL reconstructions.
Of the 307 human tissue reconstructions, 74 (24%) cases were excluded as they did not return to play in the AFL either at all or prior to 2015, leaving 233 (76%) who returned to play in the AFL (without further ACL injury prior to return) to be split into the three groups.
The final three groups were of: 70 (30%) players that returned at < 10 months, 84 (36%) at between 10 and 12 months and 79 (34%) players at > 12 months post-injury.
Figures 2 and 3 assess the secondary outcomes of subsequent ACL injury in a match plotted against time from initial ACL injury and number of return matches played (in the first 20 matches after return to play).
Fig. 2.
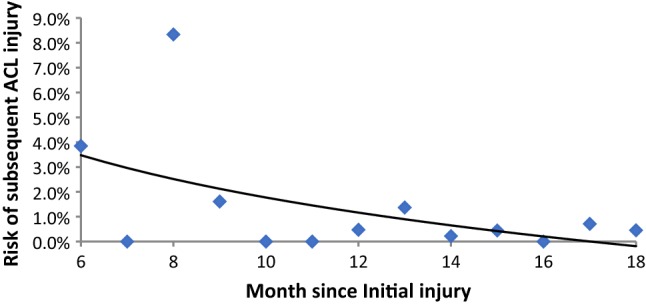
Risk of subsequent ACL injury by month after initial ACL injury
Fig. 3.
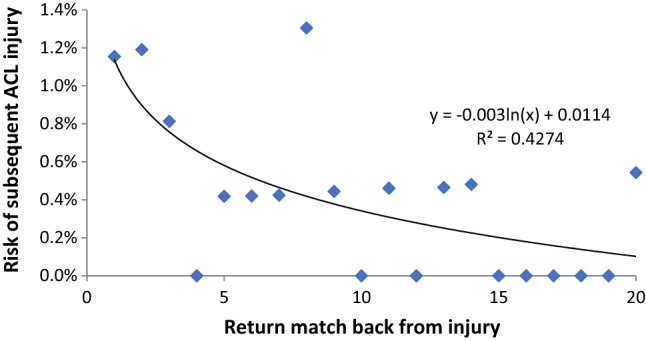
Risk of subsequent ACL injury by return match played after initial ACL injury
We found that there was a weak relationship (R2 = 0.246) between injury risk and time since injury when assessing the risk of ACL injury recurrence per month after the initial injury. Figure 2 shows this risk of re-injury from post-injury month six onwards, where there appears to be a slightly higher risk of injury recurrence between months 6–10.
When focusing on the first 20 matches back from injury (Fig. 3), we found a moderate correlation existed when comparing the number of matches played post-injury with the risk of ACL recurrence. The risk of subsequent injury upon return is approximately 1.2% in the first return game and drops down to plateau of approximately 0.15% risk per game by the 20th game back, following a log decay pattern with R2 = 0.43.
Table 1 shows a comparison of subsequent ACL injury risks relative to the three return-to-AFL groups. We found that the return at 10–12 month group had the lowest ongoing subsequent ACL injury risk (0.20% per game played). Players returning at less than 10 months or greater than 12 months had a higher per-match re-injury risk of 0.29% and 0.35%, respectively. To put this into perspective, the baseline risk of ACL injury per player match in AFL athletes with no prior ACL injury history is 0.06%; therefore, the risks for subsequent injury for returning below 10 months and above 12 months are fivefold higher for all subsequent games than for non-injured players. However, it is only threefold higher for the 10–12 month return group.
Table 1.
Injury risk and subsequent career games per return-to-play groups
| Return to competition | ACL injuries in a match† | Player matches | ACL injury risk per game (%) | Average subsequent career games post-injury |
|---|---|---|---|---|
| No history of previous ACL injury | 186 | 307,048 | 0.06 | N/A |
| Returned to play < 10 months | 12 | 4197 | 0.29 | 60.1 |
| Returned to play 10–12 months | 10 | 4928 | 0.20 | 58.8 |
| Returned to play > 12 months | 15 | 4232 | 0.35 | 53.8 |
†The ‘ACL injuries in a match’ column donates initial ACL injuries in the first row and subsequent ACL injuries for all remaining rows of player groups returning from ACL injury
Of the three groups, the less than 10 month return group played on average the highest number of subsequent return games (60.1) following ACL injury, with the 10–12 month group close behind (58.8). In comparison, AFL athletes returning at greater than 12 months averaged only a further 53.8 career matches.
In addition to varying subsequent ACL injury rates between groups, we also looked for evidence of difference in injury risk for other injury categories potentially related to the ACL injury (Table 2). Players returning at > 12 months had higher overall percentage of future career games missed through subsequent ACL injuries (4.8% vs. 2.4%), and through all hamstring and knee injuries combined (12.6% vs. 8.4%) than players who returned at ≤ 12 months (both P < 0.001). Also, players who return to sport from ACL reconstruction at greater than 12 months have higher risks of further knee cartilage (3.7% prevalence per week) and patella tendon (0.6% prevalence per week) injury, than those who return to play at 10–12 months (1.8% and 0.1%, respectively), both statistically significant outcomes using χ2 tests (P < 0.01). Players who return at greater than 12 months did, however, have a slightly lower prevalence of hamstring injuries than those returning earlier.
Table 2.
Relationship between ACL injured return-to-play groups and prevalence of hamstring and knee injuries per game week
| Return to competition | Hamstring (%) | Knee cartilage (%) | Patella tendon (%) | All other knee injuries (non-ACL) (%) | Subsequent ACL injuries (%) | Total hamstring and knee injury (%) |
|---|---|---|---|---|---|---|
| Returned to play < 10 months | 3.3 | 1.2 | 0.4 | 1.6 | 2.5 | 8.5 |
| Returned to play 10–12 months | 3.6 | 1.8 | 0.1 | 0.8 | 2.2 | 8.4 |
| Returned to play > 12 months | 2.9 | 3.7 | 0.6 | 1.1 | 4.8 | 12.6 |
| All return post human tissue ACL reconstruction | 3.2 | 2.2 | 0.3 | 1.3 | 3.0 | 9.7 |
Discussion
Our study shows that players returning to competition matches at 10–12 months post-injury have better global outcomes than those who returned earlier or later (Tables 1 and 2), when considering the risk of subsequent lower limb injury (ACL recurrence or other injury) and the number of subsequent career games played.
A secondary finding is that there is a higher correlation for risk of subsequent ACL injury between number of return matches played (Fig. 3) than months since original injury (Fig. 2). No matter what the original return month is, the most dangerous period in terms of risk of subsequent ACL injury is the first 8–9 matches of return to play (Fig. 3).
This reinforces the understanding that post-ACL reconstruction deficits persist independent of time following reconstruction [10] and that ACL injury and recurrence risk collates with competition play, as the ACL injury rate is twenty times higher during matches than during training, rather than at any stage of rehabilitation [4].
Return to Sport and Injury Risk Following ACL Reconstruction
ACL reconstruction has relatively high documented rates of return to elite sports (80%) [4], and these outcomes are comparable to those found in AFL-specific studies (74–77%) [1, 4]. Despite a good chance of returning to the elite level, however, medium- and long-term outcomes remain poor, especially when considering injury recurrence [4, 19].
The risk of ACL injury and subsequent re-injury (both ipsilateral graft rupture and contralateral knee ACL injury) in the AFL is high. Within 12 months of reconstruction, there has been shown to be an 11-fold risk of ipsilateral (graft rupture) injury and a fourfold increased risk of contralateral injury [20].
A study looking at the same cohort of AFL athletes (between 1990 and 2000) as used in this study found that 47% of players will either retire from sport as a consequence of their ACL injury or have an ACL injury recurrence further down the track in their career [19]. Furthermore, a 15-year prospective study of elite soccer players showed that only 65% of athletes sustaining an ACL injury continued to play at the top level 3 years post-injury, despite high rates (similar to those reported above) of return to play within a year of reconstruction [21].
Increased Risk of Hamstring and Knee Injury
Our findings that ACL injury is associated with a high risk of subsequent hamstring injury [20, 22] and subsequent other (non-ACL) knee injury [23] are consistent with previous studies in the literature. The larger cohort studied in this paper offers a more precise understanding of the risks involved and association between injury risk and timing of return to sport.
Articular cartilage damage at the time of ACL injury is an important predictor of poor outcomes post-ACL reconstruction [24]; however, it is uncertain how it affects short-term clinical outcomes and whether it is a predictor for delayed return to sport [25]. Our study found that the risk of subsequent knee cartilage injury is significantly higher for athletes returning at greater than 12 months than for those who return earlier, which could be possibly explained by greater knee cartilage damage at time of ACL injury being an associated cause of delayed return to sport. Delay in ACL reconstruction is also shown to be associated with more severe chondral injuries [26]. In this cohort of elite athletes, it can be safely assumed that expedited reconstruction of ACL injury would have been the norm, given the pressures to return to sport.
Early Return from ACL Reconstruction Leads to Increased Risk of Re-injury
Successful early return to play following ACL injury is the key outcome for player and club. To this end, ACL reconstruction as soon as possible is acknowledged as the best option for athletes who are looking to return to elite-level field sport requiring pivot-twisting.
As a consequence of sporting pressures, biomechanical and strength factors, as well as access to optimal rehabilitation facilities, elite athletes return to play earlier than non-elite athletes [27]. Our results show that there is perhaps a ‘sweet spot’ time of 10–12 months for return to matches from ACL injury in order to minimise the risks of injury recurrence and other subsequent injury. Our study shows negative association with delayed return (> 12 months), but previous study has documented increased recurrence with premature return [15].
Given the pressures to return to elite sport as quickly as possible, it could be the case that players who return after 12 months fall into the category of ‘slow responding’ or ‘difficult’ injuries, which could also explain their high injury recurrence risk. This hypothesis is further supported by the evidence of increased correlation of knee cartilage injuries post return to sport in this cohort as discussed previously.
Artificial ligament reconstructions are now known to have quicker return-to-play times but have a much higher re-rupture rate [17]. There is a consensus agreement that optimal graft choice for ACL reconstruction is a locally harvested autograft [28]; however, due to delayed graft failure, this was not widespread knowledge at the time of the prospective data collection. Therefore, surgical management utilising an artificial ligament was excluded from the main analysis study.
Strengths and Limitations of this Study
One of the main benefits of using the AFL injury database is that AFL is a uniquely isolated football league with no clear rival leagues at the elite level of participation. Therefore, it can be assumed that the injury database captures the entire sporting careers of the players in the league and accurately accounts for rates of return to sport, re-injury and retirement, as any retirement from the league is most likely to reflect retirement from elite sport. Furthermore, except for a few players who may have started their careers in the 1980s, entire sporting careers would be captured for most included players during this time frame.
A limitation of this study is that it was based on limited data (extracted from an injury database) that did not contain the full history of each injury, including surgical details (neither time between original ACL injury and surgery nor severity of co-existing findings, like cartilage damage). If there were players who had their reconstruction delayed from the time of injury they may have subsequently returned later post-injury and this may have skewed data. However, it is likely that in this elite sport setting, all patients would have progressed to reconstruction as early as possible.
Perspective
Current literature cites milestone-based progression, assessed through functional testing, as the return-to-sport standard [8]. However, there is no evidence to support the predictive validity of any of the proposed functional performance tests or return-to-sport criteria currently published [29]. Furthermore, recent literature argues that real-world return-to-sport decisions are more founded in psychological factors, such as fear of re-injury, hesitancy and confidence issues [30].
Given the complexities of the post-reconstruction recovery and rehabilitation process, no single measure of functional assessment, nor time from surgery, should be the lone determining factor of return to sport [10]. Ultimately, a multidisciplinary approach considering optimal time post-injury alongside holistic aspects, including psychological, physiological and functional mechanical parameters, is best adopted with these return-to-play decisions [8, 30].
Our findings will help to complement the return-to-play decision-making process by highlighting that delayed return may also be associated with worse outcomes. This study adds the understanding that not only may there be risks from returning too early from ACL reconstruction, but there may also be risks from delaying return for too long, which has not been previously reported.
Acknowledgements
The authors would like to acknowledge the support of the Australian Football League (AFL) Research Board.
Funding
Not externally funded.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
The injury and player match data were extracted from the AFL injury database with all identifying features removed. The study methods were approved by the Human Research Ethics Committee of Sydney University, Sydney, Australia. Protocol Number: 2018/512.
Informed consent
For this type of study, informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lai CCH, Feller JA, Webster KE. Fifteen-year audit of anterior cruciate ligament reconstructions in the Australian Football League from 1999 to 2013: Return to play and subsequent ACL injury. The American Journal of Sports Medicine. 2018;46(14):3353–3360. doi: 10.1177/0363546518803932. [DOI] [PubMed] [Google Scholar]
- 2.Orchard J, Seward H, McGivern J, Hood S. Rainfall, evaporation and the risk of non-contact anterior cruciate ligament injury in the Australian Football League. Medical Journal of Australia. 1999;170(7):304–306. doi: 10.5694/j.1326-5377.1999.tb127782.x. [DOI] [PubMed] [Google Scholar]
- 3.Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish national anterior cruciate ligament register. Arthroscopy. 2014;30(7):803–810. doi: 10.1016/j.arthro.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 4.Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. British Journal of Sports Medicine. 2018;52(2):128–138. doi: 10.1136/bjsports-2016-096836. [DOI] [PubMed] [Google Scholar]
- 5.Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: Epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surgery, Sports Traumatology, Arthroscopy. 2009;17(2):117–124. doi: 10.1007/s00167-008-0654-3. [DOI] [PubMed] [Google Scholar]
- 6.Moses B, Orchard J, Orchard J. Systematic review: Annual incidence of ACL injury and surgery in various populations. Research in Sports Medicine (Print) 2012;20(3–4):157–179. doi: 10.1080/15438627.2012.680633. [DOI] [PubMed] [Google Scholar]
- 7.Saw R, Finch CF, Samra D, et al. Injuries in Australian rules football: An overview of injury rates, patterns, and mechanisms across all levels of play. Sports Health. 2017;10(3):208–216. doi: 10.1177/1941738117726070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies GJ, McCarty E, Provencher M, Manske RC. ACL return to sport guidelines and criteria. Current Reviews in Musculoskeletal Medicine. 2017;10(3):307–314. doi: 10.1007/s12178-017-9420-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2011;27(12):1697–1705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Myer GD, Martin L, Jr, Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: Evidence for objective return-to-sport criteria. The American Journal of Sports Medicine. 2012;40(10):2256–2263. doi: 10.1177/0363546512454656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myklebust G. Return to play guidelines after anterior cruciate ligament surgery. British Journal of Sports Medicine. 2005;39(3):127–131. doi: 10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petersen W, Zantop T. Return to play following ACL reconstruction: Survey among experienced arthroscopic surgeons (AGA instructors) Archives of Orthopaedic and Trauma Surgery. 2013;133(7):969–977. doi: 10.1007/s00402-013-1746-1. [DOI] [PubMed] [Google Scholar]
- 13.Zaffagnini S, Grassi A, Serra M, Marcacci M. Return to sport after ACL reconstruction: How, when and why? A narrative review of current evidence. Joints. 2015;3(1):25–30. [PMC free article] [PubMed] [Google Scholar]
- 14.Webster KE, Feller JA. Return to level I sports after anterior cruciate ligament reconstruction: Evaluation of age, sex, and readiness to return criteria. Orthopaedic Journal of Sports Medicine. 2018;6(8):2325967118788045. doi: 10.1177/2325967118788045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. British Journal of Sports Medicine. 2016;50(13):804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saw R, Finch CF, Samra D, et al. Injuries in Australian Rules Football: An overview of injury rates, patterns, and mechanisms across all levels of play. Sports Health. 2018;10(3):208–216. doi: 10.1177/1941738117726070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iliadis DP, Bourlos DN, Mastrokalos DS, Chronopoulos E, Babis GC. LARS artificial ligament versus ABC purely polyester ligament for anterior cruciate ligament reconstruction. Orthopaedic Journal of Sports Medicine. 2016;4(6):2325967116653359. doi: 10.1177/2325967116653359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans JD. Straightforward statistics for the behavioral sciences. Pacific Grove: Brooks/Cole Pub. Co.; 1996. [Google Scholar]
- 19.Liptak MG, Angel KR. Return to play and player performance after anterior cruciate ligament injury in elite Australian rules football players. Orthopaedic Journal of Sports Medicine. 2017;5(6):2325967117711885. doi: 10.1177/2325967117711885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. The American Journal of Sports Medicine. 2001;29(2):196–200. doi: 10.1177/03635465010290021301. [DOI] [PubMed] [Google Scholar]
- 21.Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: A 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. British Journal of Sports Medicine. 2016;50(12):744. doi: 10.1136/bjsports-2015-095952. [DOI] [PubMed] [Google Scholar]
- 22.Toohey LA, Drew MK, Cook JL, Finch CF, Gaida JE. Is subsequent lower limb injury associated with previous injury? A systematic review and meta-analysis. British Journal of Sports Medicine. 2017;51(23):1670. doi: 10.1136/bjsports-2017-097500. [DOI] [PubMed] [Google Scholar]
- 23.Walden M, Hagglund M, Ekstrand J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. British journal of sports medicine. 2006;40(2):158–162. doi: 10.1136/bjsm.2005.021055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takeda T, Matsumoto H, Fujikawa K. Influence of secondary damage to menisci and articular cartilage on return to sports after anterior cruciate ligament reconstruction. Journal of Orthopaedic Science. 1997;2(4):215–221. doi: 10.1007/BF02489041. [DOI] [Google Scholar]
- 25.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: A systematic review. The American Journal of Sports Medicine. 2009;37(7):1434–1443. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 26.Fok AW, Yau WP. Delay in ACL reconstruction is associated with more severe and painful meniscal and chondral injuries. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21(4):928–933. doi: 10.1007/s00167-012-2027-1. [DOI] [PubMed] [Google Scholar]
- 27.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: Two-thirds of patients have not returned by 12 months after surgery. The American Journal of Sports Medicine. 2011;39(3):538–543. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 28.Tulloch SJ, Devitt BM, Porter T, et al. Primary ACL reconstruction using the LARS device is associated with a high failure rate at minimum of 6-year follow-up. Knee Surgery, Sports Traumatology, Arthroscopy. 2019;27:3626–3632. doi: 10.1007/s00167-019-05478-3. [DOI] [PubMed] [Google Scholar]
- 29.Narducci E, Waltz A, Gorski K, Leppla L, Donaldson M. The clinical utility of functional performance tests within one-year post-ACL reconstruction: A systematic review. International Journal of Sports Physical Therapy. 2011;6(4):333–342. [PMC free article] [PubMed] [Google Scholar]
- 30.Burland JP, Toonstra J, Werner JL, Mattacola CG, Howell DM, Howard JS. Decision to return to sport after anterior cruciate ligament reconstruction. Part I: A qualitative investigation of psychosocial factors. Journal of Athletic Training. 2018;53(5):452–463. doi: 10.4085/1062-6050-313-16. [DOI] [PMC free article] [PubMed] [Google Scholar]