Abstract
Proximal humerus fractures (PHF) are common injuries in the elderly population. Conservative treatment is indicated for undisplaced and stable fractures, which account for almost 80% of the cases. More complex fracture patterns might need surgery, with a wide variety of indication criteria and surgical techniques described in the literature. Surgical treatment should be reserved for patients in good clinical conditions, autonomous in daily living activities and able to adhere to postoperative rehabilitation protocols. In the elderly population with severe osteoporosis, cognitive impairment and clinical comorbidities, the risk of surgical failures is high. In these patients, the choice between surgical and conservative treatment, as well as for the type of procedure, is even more difficult, with no general consensus in the literature. Final indication is usually conditioned by surgeon’s experience and preference. Two independent reviewers (B.H and G.G) independently extracted studies on proximal humeral fractures. All selected studies were screened independently (B.H and G.G) based on title and abstract. Then the full text of any article that either judged potentially eligible was acquired and reviewed again. Any disagreement was resolved by discussing the full text manuscripts. Aim of the present paper is to review the literature about indications and results of osteosynthesis for proximal humerus fragility fractures in the elderly population.
Key words: proximal humerus fractures, osteosynthesis, osteoporosis, fragility fractures, elderly
Introduction
Proximal humerus fractures (PHFs) are the third most common fragility fractures of the appendicular skeleton, after proximal femur and distal radius fractures. These fractures are typically related to low energy trauma in elderly patients affected by osteoporosis. 1,2
Currently, the ideal treatment for these fractures is debated in the literature. Several indications and treatment options have been described without a clear evidence about outcome.3
Nearly 80% of PHFs have a stable configuration. In these cases, excellent results may be achieved with conservative treatment, especially in elderly patients with low functional demands. Conversely, absolute surgical indication for PHFs treatment is rare, representing less than 1% of cases. The remaining cases may benefit from surgical intervention. Whether reduction and fixation or primary shoulder arthroplasty may be better indicated in these cases is still matter of debate.4
Conservative treatment is generally preferred also for displaced or comminuted PHFs in patients older than 85 years of age affected by severe osteoporosis, cognitive impairment or significant comorbidities.4-7
Proper indication for treatment should take into account different factors: the expected outcome (with and without surgical treatment), patient’s functional demand and compliance to treatment protocol, surgeon’s training and experience.8 Ideally, fracture reduction and fixation should be preferred to arthroplasty because of the better clinical results achieved in uncomplicated cases with anatomic reconstruction.9,10 On the other hand, especially in fragility osteoporotic fractures, osteosynthesis is jeopardized by a high rate of complications, that are frequently related to insufficient understanding of risk factors for humeral head avascular necrosis (AVN) and failure of fixation.11,12 Humeral head vascular supply relays on the ascending branches of the axillary artery, with the posterior circumflex artery demonstrated to be dominant (about 64%).13 Hertel et al. identified some PHFs patterns and characteristics strongly related with the risk of AVN of the humeral head. These include a disrupted medial hinge, a calcar segment shorter than 8 mm and a fracture of the anatomical neck. These criteria combined have a predictive positive value of humeral head AVN of 0.97 according to the authors.14 Even though it’s not possible to quantify exactly the risk of failure, internal fixation is not recommended for head splitting fractures or in presence of multiple articular fragments in elderly patients: in these cases, shoulder arthroplasty should be preferred.15
According to the literature, osteosynthesis can be considered as a treatment option for Neer 2-part fractures, Neer 3 and 4-part fractures with tuberosities displaced more than 5 mm, false head split fractures (minimal part of the humeral head attached to the tuberosity fragment), Neer 2-part fractures of the surgical neck, Neer 2, 3, 4-part fractures with angulation of the humeral head in varus or valgus > 30, and for fracture-dislocations with impaction fracture of the humeral head with retained soft-tissue attachment.1,4 On the other hand, the low inteobserver and intraobserver reliability of Neer classification renders the latter criteria of limited clinical value.1 Aim of the present paper is to review the literature about indications and results of osteosynthesis for proximal humerus fragility fractures in the elderly population.
Peculiarities of proximal humerus fragility fractures fixation in the elderly
When facing a patient with a fragility PHF, the intrinsic difficulty of anatomically reducing and fixing with adequate stability the osteoporotic fragments must be considered, beside the general features of the patient and the fracture.
The main technical difficulties arise from the combination of a weak and brittle bone (the humeral head can be conceived as an eggshell) with a comminuted fracture pattern.8
Closed reduction internal fixation (CRIF) and open reduction internal fixation (ORIF) techniques have been developed and commonly used for normal and healthy bone.
Ageing and osteoporosis affect the mechanical properties of the bone, altering both elastic and strength properties.
With osteoporosis cortices become thinner and the trabecular network is altered, making bone prone to mechanical failure particularly in the metaphyseal region.16,17
Conservative versus operative treatment in the elderly patient
Fracture pattern is the first factor that is usually considered to define treatment strategy. 18 Most PHFs are undisplaced or minimally displaced, involving the surgical neck and the greater tuberosity.19,20 In the elderly population, conservative treatment of these fractures is a well consolidated practice, that guarantees a high rate of successful outcomes.3,6,21
There are different immobilization techniques proposed for non-operative treatment of PHFs as a Gilchrist or a Velpeau bandage. Regardless the non-operative method, a close radiological and clinical follow-up is required in these patients.
There is no consensus on non-operative treatment modalities. However, early mobilization is generally recognized as the mainstay of conservative treatment. In unstable fracture patterns with a high risk of displacement progression, a period of immobilization from 3 to 4 weeks (until soft callus formation) is usually preferred.
The choice of the optimal treatment becomes more difficult when PHFs are displaced and more complex. In these cases, fracture morphology, patients’ demands and surgeons experience should be considered. 4,7 Although a large number of studies support operative treatment for displaced 2-part and 3-part PHFs, the most recent literature is not prejudicial to conservative treatment. 6 There is lack of well-designed comparative studies for 2-part displaced PHFs, which account for about 30 – 44% of all PHFs and usually have acceptable clinical outcomes with non-operative treatment. In these fracture patterns conservative treatment should be considered in patients with low demands and poor bone quality, whereas operative treatment should be considered in patients with high demands and good bone quality.3,19-21
Isolated great tuberosity fractures, especially with postero-superior displacement > 5mm, usually require operative treatment in order to avoid subacromial impingement and loss of external rotation.22 Surgical indication is usually considered for young patients, who more often present with isolated displaced greater tuberosity fractures. Clinical data about this specific fracture in the elderly population is lacking, with no evidence about how displacement criteria applied to young patients should be transferred to the elderly population.
Lesser tuberosity fractures are rare injuries produced by muscle contraction (as in seizures), or when the subscapularis muscle forcefully contracts to resist external forces in abduction and external rotation on the shoulder. These fractures typically affect young patients, with significant displacement in most cases. According to these epidemiological and biomechanical data, these injuries should not be considered as fragility fractures.23-25
Three and 4-part fractures account for nearly 11 – 20% of PHFs.20 Operative treatment is usually indicated for young patients with 3 and 4-part PHFs, but conservative management should be considered in elderly patient. In a retrospective study on 125 elderly patients with 4-part valgus impacted PHF, Court-Brown et al. reported good to excellent outcomes with conservative treatment. 26 A meta-analysis of randomized controlled trials (RCT) on operative versus conservative treatment in displaced 3 and 4- part PHFs in the elderly concluded that functional improvement was not significant and complication rate was higher in the operative group.27 Handoll et al. reported no significant difference in the clinical outcome (Oxford Shoulder Score) between conservative and surgical treatment in 3 and 4-part PHFs.28 Several reviews and studies support these data.29-31 A Cochrane review on proximal humeral fractures evaluated 31 randomized controlled trials, of which only 8 studies (involving 567 elderly patients) compared conservative to operative treatment. The authors reported no significant difference in clinical result and quality of life in patient-reported shoulder and upperlimb function at 1 and 2-year follow-up. Even though there was moderate evidence of a higher risk of complications after surgery, the 95% confidence intervals reveled a greater risk of potential complications in the conservative treatment group.3
Conversely, Olerud et al. reported better functional outcomes with locking plate fixation compared to conservative treatment in the elderly population with displaced 3-part PHFs. However, a 30% higher risk of additional surgery in the operative group was noted.32
Many studies suggest that PHFs in the elderly may be treated conservatively with acceptable outcomes, but there are specific fracture patterns and patients that benefit from operative treatment.33 Sabharwal et al. conducted a meta-analysis on 528 patients detected in 7 RCTs comparing operative to conservative treatment of PHFs. Despite there were no differences in functional outcomes comparing conservative and operative treatment of displaced PHFs, some differences in clinical outcome emerged when analyzing specific fracture patterns and surgical techniques.34 The four-part fractures treated surgically had better clinical outcomes and were less likely to result in osteoarthritis, osteonecrosis and malunion. 34 However, these data were heterogeneous and did not reach any statistical significance. Studies aimed on specific fracture patterns and surgical procedures should be performed in order to identify the patients that may benefit from surgery and the type of the procedure that is more adequate in these cases.
Patient’s characteristics like age and associated injuries consistently influence decision making between operative or conservative treatment of displaced PHFs in elderly patients. Many authors argue that conservative treatment in displaced or comminuted PHFs should be preferred in patients older than 85 years old, with cognitive impairment or clinical comorbidity, severe osteoporosis, non-associated fractures, rheumatoid arthritis and concurrent neoplasm.4-7 Clement et al. sustain that factors associated with social independence are more predictive of functional outcomes than age.21 Despite the lower functional outcomes reported with conservative treatment, subjective perception of outcome can be satisfactory if no residual pain is present.4 Although the risk of non-union, malunion and osteonecrosis after conservative treatment is generally accepted, the surgeon should consider that salvage surgery in these cases is more likely to result in worse outcomes compared to primary operative treatment.4,35,36
Percutaneous fixation in the elderly patient
Closed reduction and percutaneous pinning (CRPP) of PHFs was described for the first time in 1962 by Bohler. CRPP may be considered as an alternative to ORIF in specific fracture patterns and in selected patients. Stability achieved with CRPP is mechanically inferior to intramedullary nail and plate fixation.37,38 Pin configuration is a significant factor in order to enhance mechanical stability, that is improved by biplanar fixation and by increasing the number of pins engaging the cortex.
Indications for CRPP include 2-part fractures of the surgical neck, isolated greater tuberosity fractures, 3-part fractures of the surgical neck with involvement of the greater tuberosity and 4-part valgus impacted fractures.1,39,40 Use of CRPP in PHFs is less invasive, allowing respect of soft tissues and blood supply during the surgical procedure. Compared to open reduction and internal fixation (ORIF), CRPP potentially has lower rates of avascular necrosis (AVN), higher union rates, less scar formation at the scapulo-thoracic joint and better cosmetics.39 Different studies reported good outcomes with CRPP.41-43 In a study on 113 patients with 2-part PHFs, Tamimi et al. reported better outcomes with CRPP in patients of all ages and better functional results compared to intramedullary nailing in elderly patients.43
Gupta et al. published a review on 4500 patients, reporting a considerably higher complication rate with CRPP when compared to ORIF, hemiarthroplasty (HA) and reverse shoulder arthroplasty (RSA). Complications observed with CRPP included humeral head necrosis (11.7%), pin migation/breakage (4.1%), superficial infection (4.1%), malunion (3%), neurologic injuries (1.5%), nonunion and deep infection (1%).44
Resch et al., in a study on 27 patients with 3 and 4-part PHFs treated with CRPP, reported that all 3-part fractures had very good functional results and no complications. The valgus impacted 4-part fractures had good functional outcomes and 11% of avascular necrosis (2/18).45
In the study performed by Keener et al. on a total of 27 PHFs (7 two-part, 8 threepart and 12 four-part valgus impacted), a 100% rate of fracture healing was reported, together with good functional outcomes (mean Constant score of 73.9 points) and a low rate of complications after CRPP. Fracture type, age, malunion and osteoarthritis had no influence on outcomes.39 It must be highlighted that clinical series reporting on CRPP do not focus specifically on geriatric osteoporotic fractures.
Ideally, CRPP should be performed when a stable closed reduction can be achieved and in presence of minimal fracture comminution, an intact medial calcar, a good bone stock and a compliant patient.1,39,40 CRPP should not be used in non-optimally reduced PHFs since the quality of fracture reduction directly influences construct stability, hence anatomical and clinical outcomes.40 Fracture comminution and poor bone quality are a relative contraindication to CRPP, that consequently may hardly apply to osteoporotic elderly fractures. Pin migration, loosening and loss of reduction are associated with these factors in different studies.1,39,40,46 On the other hand, some technical advances on the classical CRPP technique, especially with threaded wires engaging the outer cortex and connected as an external fixator, may by-pass these limitations and become a good choice for elderly patients.40,47 Blonna et al. suggested an alternative to the conventional pinning technique, consisting in the use of full threated pins augmented by an external frame. The authors introduced the term “hybrid technique” to describe how this technique includes features of both external and internal fixation. The authors prospectively studied 42 patients treated with conventional pinning (2.5 mm terminally threaded pins) and 49 patients treated with the hybrid technique (2.5 mm pins characterized by a 7 cm thread augmented with external fixator). They observed a significant reduction in complication and revision rates in the hybrid group.48
Intramedullary nail (IMN) fixation in the elderly patient
The goal of nail fixation in PHFs is to provide stability in order to allow early motion of the shoulder and improve functional outcomes compared to conservative treatment.49 From the first nail described by Rush, humeral nailing has undergone important improvements and innovations. 49,50 While first generation nails had no ability to control rotation, second generation nails had the major disadvantage of frequent migration of the proximal interlocking screws.49 In fact, functional outcomes reported with first and second generation nails were disappointing and threatened by frequent complications such as nonunion, hardware migration and chronic shoulder pain.42 Third generation nails have a better locking mechanism of proximal screws, allowing more stable constructs and a medial entry point on the humeral head to preserve the rotator cuff footprint. These improvements have led to better functional outcomes and decreased complication rates.1,42 (Figure 1)
Different authors have reported good clinical outcomes in 2 and 3-part PHFs treated with third generation humeral nails.51-54 In a retrospective study on 38 patients with 2-part surgical neck PHFs treated with locked angular stable intramedullary nail, Hatzidakis et al. reported 100% primary healing, a mean Constant score of 71 points and a mean forward flexion of 132° with little residual shoulder pain.55 However, Nolan et al. reported a high complication rate in 18 patients with 2 and 3-part PHFs treated with Polarus nail.56
In a systematic review including 2155 patients (66 studies) treated with different modalities for PHFs, Lanting et al. reported 11.9% complication rate for IMN. The incidence of nonunion or malunion was 5%, implant loosening or migration 3.2% and osteonecrosis 4.5% (19.2% in 3 and 4-part fractures).57
Intramedullary locked nails for PHFs compared to locked plates should provide the theoretical advantage of improved construct stability, even in case of osteopenic or osteoporotic 3 and 4-part PHFs.58 These data are in discordance with cadaveric biomechanical comparative studies between IMN and locking plates, reporting lower resistance at bending and torsion for nails. The authors hypothesized that the early rate of failure of IMN is correlated to the moment transmitted to the screw-bone interface in the humeral head; this aspect is matter of concern for early postoperative mobilization in osteoporotic bone.59
Recent studies assert that results achieved with IMN (third generation implants) in 2, 3 and 4-part PHFs are comparable to those reported with locking plates.60,61 Furthermore, in a comparative randomized study of 2-part PHFs treated with IMN or plates, Zhu et al. reported complication rates of 4% and 31%, respectively. 62
Age, osteoporosis and 3 or 4-part PHFs appear to affect clinical outcome of IMN.63 Patients older than 65 years have an augmented risk of worse outcome, most likely due to osteoporosis and the consequent decreased grip on bone of the implant. In this scenario, proximal screw cut out, greater tuberosity migration and varus displacement are the most common complications. 64 According to some authors, third generation nails partially overcame these drawbacks.65 Mihara et al. reported satisfactory functional outcomes and no screw cut out with a “pin lock nail system’’ in 19 geriatric patients.66 Boileau et al. proposed a new locked nail design to optimize tuberosity fixation and stable support for the humeral head. The preliminary functional results in 24 patients with a mean age of 64 years were good, with no need for further surgery.67
Some technical tips should be observed when nailing a PHF, especially in osteoporotic bone. The supraspinatus should be split at the lateral edge of the articular surface through the muscle belly instead of splitting the tendon. The entry point must be at the center of the humeral head, so that the stability of the fixation doesn’t rely exclusively on the proximal screws, but is favored by the subchondral bone-nail interface, where the bone remains of better quality in comparison with other areas of the humeral head. The superior resistance to varus forces, obtained with the interference of the nail with the subchondral bone, is particularly important in osteoporotic fragility fractures, in which the weak cancellous bone of the medial calcar cannot ensure a reliable stability of the proximal screws.5,68 If these principles are not respected, a high failure rate should be expected. (Figure 2)
Locking plate osteosynthesis in the elderly patient
According to the literature, locking plate fixation (LPF) is the most widely used osteosynthesis technique for proximal humeral fractures. LPF is indicated for almost all fracture patterns, including humeral head fractures amenable to reconstruction. However, the burden of complications, especially in elderly patients with osteoporosis, is often unacceptably high.4,69
In a study on 27.017 patients surgically treated for PHFs, Zhang et al. reported a higher readmission rate for ORIF (29%) when compared to reverse shoulder arthroplasty (20 %) and hemiarthroplasty (16 %).70
In literature, the mean complication rate reported for ORIF is 30%, with articular screw penetration (primary or secondary to reduction loss) and avascular necrosis of the humeral head accounting for half of cases. The average re-operation rate is about 14%.71-73 In interpreting these data, it must be underlined that LPF is the gold standard for the treatment of more complex fracture patterns and figures about complications and re-operations may be affected by a selection bias.
Jung et al., reporting on 252 patients treated with locking plates, observed a significant correlation with loss of reduction in case of osteoporosis, varus displacement, medial comminution and insufficient medial support.74
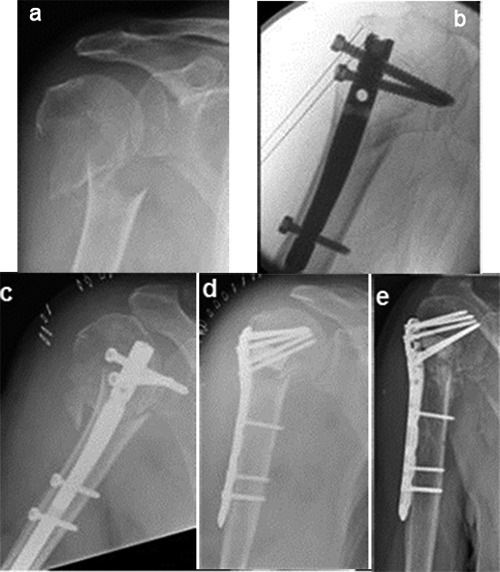
Figure 1.

Right proximal humeral 3-part fracture in a 79-year-old woman treated with IMN: (a) preoperative x-rays; (b) preoperative CT scans respectively in the coronal, axial and sagittal plane; intraoperative fluoroscopy (c) and postoperative x-rays (d) showing a correct medial entry point and proximal screws stabilization of the greater tuberosity; (e) xrays 6 months after surgery showing uneventful healing without secondary displacement.
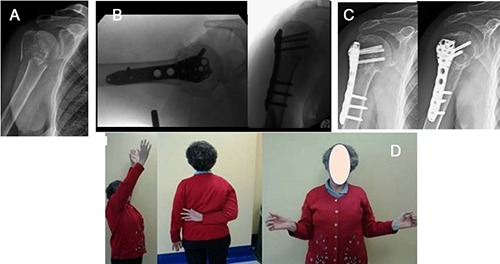
Figure 2.
Right proximal humeral 2-part fracture in a 76-year-old woman affected by moderate dementia: (a) preoperative x-rays; (b) intraoperative fluoroscopy showing a wrong entry point (too anterior and lateral) and an excessively buried nail; (c) x-rays showing secondary displacement 4 days after surgery; (d) revision surgery with a locking plate and synthetic bone substitute to fill the antero-lateral bone defect resulting from nail migration; (e) x-rays 4 months after surgery.
There are several concepts to keep in mind when planning an ORIF with locking plate in osteoporotic bone, because the unreliable fixation of the implant is a major concern. With respect to conventional plates, locking plate systems can stabilize fracture fragments without friction between plate and bone, providing more stability in case of osteoporosis. The correct position of the plate, just inferior to the flare of the greater tuberosity and lateral to the bicipital groove, is important to avoid lateral impingement.75,76
An anatomic reduction is essential to achieve a stable fixation and contributes to increase its longevity. As suggested by Krappinger et al., correct alignment of the medial cortices and anatomic reduction are the most important prognostic factors to avoid secondary displacement.77 (Figure 3)
The reconstruction of the calcar in case of disruption is the first step to achieve. This can be obtained by indirect manipulation or directly through the fracture line. If intact or partially preserved, the medial periosteum allows indirect reduction using ligamentotaxis. Fractures with medial comminution are technically difficult to manage: in this cases, an intended impaction of the humeral head may be the solution.75,78
As suggested by Gardner et al., achieving a mechanical support of the inferomedial region of the proximal humerus for maintaining reduction is fundamental, and locking plate alone are unable to support the humeral head from a lateral position, especially if medial comminution is present.79
Fractures of the proximal humerus with medial comminution treated with locking plates are at risk of varus collapse. In their study on cadaveric humerus fixed with locking plate, Ponce et al. observed that medial comminution decreased the mean load to failure and the mean energy to failure by 48 % and 44 %, respectively.80
When reduction of the medial cortex is performed or a stable impaction of the humeral head is achieved, the placement of a superiorly directed screw in the inferomedial region of the proximal fragment is helpful to support the calcar, increasing the mean load to failure and the mean energy to failure by 31% and 44 %, respectively.80
As suggested by Padegimas et al., the calcar screw should be positioned < 12 mm from the apex of the arc of the calcar or within the bottom 25% of the humeral head. Within these cut-offs, the incidence of fixation failures was significantly reduced in their clinical series.81 (Figure 4)
Reduction of tuberosities is fundamental to lie down the humeral head on a solid cortico-cancellous rim, as stated by Hertel.8 Accepting a non-anatomic reduction or over-reducing the greater tuberosity significantly reduces the stability of the construct. Placing tension band sutures within the rotator cuff is moreover strongly recommended to counteract the traction forces on the tuberosities, to augment their reduction and improve fracture fixation.8,76,82
Another important consideration is that the quality of cancellous bone in the humeral head is heterogeneous, thus influencing proximal screws stability. The medial and superior part of the humeral head should be considered the best location for screw placement, with a divergent or parallel orientation of the screws. This construct has the highest axial pull-out strength compared with convergent orientation.83-88
Other possible tips - not yet supported by strong evidence in literature - to gain better primary stability in osteoporotic bone are represented by cement augmentation (for the head fragment itself, for the head screws or to fill metaphyseal defects) and bone grafts.
Locking plates implanted with cement augmentation are associated with decreased interfragmentary motion, higher failure loads and increased stiffness values compared with locking plates alone. The early experiences with this procedure did not highlight any risk of chondral or osseous damage with cement.75,89
A cortico-cancellous bone graft can be considered if the reduction of a comminuted calcar cannot be achieved; this option should contribute to increase stiffness and varus failure load of the plate-bone complex. 75
Figure 3.
Right proximal humeral 3-part (surgical neck and greater tuberosity) fracture in a 75-year-old woman treated with MIPO technique through a transdeltoid approach: (a) preoperative x-rays; (b) intraoperative fluoroscopy; (c) postoperative x-rays 13 months after surgery, (d) clinical result 13 months after surgery respectively in forward elevation, internal and external rotation.
Figure 4.
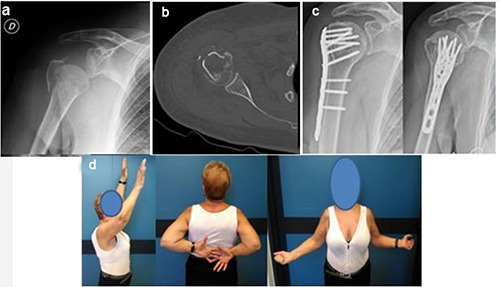
Right proximal humeral 3-part fracture in a 72-year-old woman treated with locking plate through a deltopectoral approach: preoperative x-rays (a) and axial CT scan (b) showing the valgus impacted 3-part fracture pattern and a lesser tuberosity undisplaced fracture; (c) postoperative x-rays 18 months after surgery; (d) clinical results 18 months after surgery respectively in forward elevation, internal and external rotation.
Conclusions
Surgical indication for proximal humeral fragility fractures is still matter of debate. Surgical treatment should be reserved for patients in good clinical conditions, autonomous in daily living activities and able to adhere to postoperative rehabilitation protocols. On the other hand, the surgeon should be able to choose the most suitable procedure, favoring shoulder replacement in patients at high risk for fixation failure. When considering osteosynthesis, specific technical features must be respected in the osteoporotic bone to obtain satisfactory results. CRPP, IMN and LPF are all possible options, with different indications and specific advantages and disadvantages.
Funding Statement
Funding: None.
References
- 1.Kancherla VK, Singh A, Anakwenze OA. Management of acute proximal humeral fractures. J Am Acad Orthop Surg 2017;25:42-52. [DOI] [PubMed] [Google Scholar]
- 2.Passaretti D, Candela V, Sessa P, Gumina S. Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elb Surg 2017;26:2117-24. [DOI] [PubMed] [Google Scholar]
- 3.Haldoll HH, Brorson S. Intervention for treating proximal humeral fractures in adult. Cochrane Db Syst Rev 2015;CD000434. [DOI] [PubMed] [Google Scholar]
- 4.Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Jt Surg Br 2011;93:1-11. [DOI] [PubMed] [Google Scholar]
- 5.Schumaier A, Grawe B. Proximal humerus fractures: evaluation and management in the elderly patient. Geriatr Orthop Surg Rehabil 2018;9:2151458517750516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McLaurin TM. Proximal humerus fractures in the elderly are we operating on too many? Bull Hosp Jt Dis N Y 2004;62:24-32. [PubMed] [Google Scholar]
- 7.Okike K, Lee OC, Makanji H, et al. Factors associated with the decision for operative versus non-operative treatment of displaced proximal humerus fractures in the elderly. Injury 2013;44:448-55. [DOI] [PubMed] [Google Scholar]
- 8.Hertel R. Fractures of the proximal humerus in osteoporotic bone. Osteoporos Int 2005;2:S65-72. [DOI] [PubMed] [Google Scholar]
- 9.Jobin CL, Galdi B, Anakwenze OA, et al. Reverse shoulder arthroplasty for the management of proximal humerus fractures. J Am Acad Orthop Surg 2015; 23:190-201. [DOI] [PubMed] [Google Scholar]
- 10.Gomberawalla MM, Miller BS, Coale RM, et al. Meta-analysis of joint preservation versus arthroplasty for the treatment of displaced 3- and 4-part fractures of the proximal humerus. Injury 2013;44:1532-9. [DOI] [PubMed] [Google Scholar]
- 11.Haasters F, Siebenburger G, Helfen T, et al. Complications of locked plating for proximal humeral fractures - are we getting any better? J Shoulder Elb Surg 2016;25:e295-303. [DOI] [PubMed] [Google Scholar]
- 12.Boileau P, Pennington SD, Alami G. Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elb Surg 2011;20:S47-60. [DOI] [PubMed] [Google Scholar]
- 13.Hettrich CM, Boraiah S, Dyke JP, et al. Quantitative assessment of the vascularity of the proximal part of the humerus. J Bone Jt Surg Am 2010;92:943-8. [DOI] [PubMed] [Google Scholar]
- 14.Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elb Surg 2004;13:427-33. [DOI] [PubMed] [Google Scholar]
- 15.Berkes MB, Little MTM, Lorich DG. Open reduction internal fixation of proximal humerus fractures. Curr Rev Musculoskelet Med 2013;6:47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Von Ruden C, Augat P. Failure of fracture fixation in osteoporotic bone. Injury 2016;S3-10. [DOI] [PubMed] [Google Scholar]
- 17.Yaacobi E, Sanchez D, Maniar H, et al. Surgical treatment of osteoporotic fractures: an update on the principles of management. Injury 2017;S34-40. [DOI] [PubMed] [Google Scholar]
- 18.Neer CS. Displaced proximal humeral fractures. I: classification and evaluation. J Bone Jt Surg 1970;52-A:1077-89. [PubMed] [Google Scholar]
- 19.Bergdahl C, Ekholm C, Wennergren D, et al. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the swedish fracture register. BMC Musculoskelet Disord 2016;17:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand 2001;72:365-71. [DOI] [PubMed] [Google Scholar]
- 21.Clement ND, Duckworth AD, McQueen MM, Court-Brown CM. The outcome of proximal humeral fractures in the elderly: predictors of mortality and function. Bone Joint J 2014;96- B:970-7. [DOI] [PubMed] [Google Scholar]
- 22.Platzer P, Kutscha-Lissberg F, Lehr S, et al. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Injury 2005;36:1185-89. [DOI] [PubMed] [Google Scholar]
- 23.Neer CS, II, Craig EV, Fukuda H. Cufftear arthropathy. J Bone Jt Surg Am 1983;65:1232-44. [PubMed] [Google Scholar]
- 24.Neer CS., 2nd Four-segment classification of proximal humeral fractures: purpose and reliable use. J Shoulder Elb Surg 2002;11:389-400. [DOI] [PubMed] [Google Scholar]
- 25.Tosun B, Kesemenli CC. Isolated avulsion fracture of lesser tuberosity of the humerus: review of the literature and report of two cases. Int J Shoulder Surg 2011;5:50-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Court-Brown CM, Cattermole H, McQueen MM. Impacted valgus fractures (B1.1) of the proximal humerus: the results of non-operative treatment. J Bone Jt Surg Br 2002;84:504-8. [DOI] [PubMed] [Google Scholar]
- 27.Fu T, Xia C, Li Z, Wu H. Surgical versus conservative treatment for displaced proximal humeral fractures in elderly patients: a meta-analysis. Int J Clin Exp Med 2014;7:4607-15. [PMC free article] [PubMed] [Google Scholar]
- 28.Handoll HH, Keding A, Corbacho B, et al. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J 2017;99- B:383-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huttunen TT, Launonen AP, Pihlajamäki H, et al. Trends in the surgical treatment of proximal humeral fractures - a nationwide 23-year study in Finland. BMC Musculoskelet Disord 2012;13:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rabi S, Evaniew N, Sprague SA, et al. Operative vs non-operative management of displaced proximal humerus fractures in the elderly: a systematic review and meta-analysis of randomized controlled trials. World J Orthop 2015;6:838-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Song JQ, Deng XF, Wang YM, et al. Operative vs. nonoperative treatment for comminuted proximal humeral fractures in elderly patients: a current metaanalysis. Acta Orthop Traumatol Turc 2015;49:345-53. [DOI] [PubMed] [Google Scholar]
- 32.Olerud P, Ahrengart L, Ponzer S, et al. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elb Surg 2011;20:747-55. [DOI] [PubMed] [Google Scholar]
- 33.Ghert M, McKee M. To operate or not to operate, that is the question: the proximal humerus fracture. Bone Joint Res 2016;5:490-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabharwal S, Patel NK, Griffiths D, et al. Trials based on specific fracture configuration and surgical procedures likely to be more relevant for decision making in the management of fractures of the proximal humerus. Bone Joint Res 2016;5:470-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poeze M, Lenssen AF, Van Empel JM, Verbruggen JP. Conservative management of proximal humeral fractures: can poor functional outcome be related to standard trans-scapular radiographic evaluation? J Shoulder Elb Surg 2010;19:273-81. [DOI] [PubMed] [Google Scholar]
- 36.Hanson B, Neidenbach P, de Boer P, Stengel D. Functional outcomes after non-operative management of fractures of the proximal humerus. J Shoulder Elb Surg 2009;18:612-21. [DOI] [PubMed] [Google Scholar]
- 37.Wheeler D, Colville MR. Biomechanical comparison of intramedullary and percutaneous pin fixation for proximal humeral fracture fixation. J Orthop Trauma 1997;11:363-7. [DOI] [PubMed] [Google Scholar]
- 38.Koval K, Blair B, Takei R, et al. Surgical neck fractures of the proximal humerus: a laboratory evaluation of ten fixation techniques. J Trauma 1996;40:778–83. [DOI] [PubMed] [Google Scholar]
- 39.Keener JD, Parsons BO, Flatow EL, et al. Outcomes after percutaneous reduction and fixation of proximal humeral fractures. J Shoulder Elb Surg 2007:16:33-8. [DOI] [PubMed] [Google Scholar]
- 40.Calvo E, de Miguel I, de la Cruz JJ, Lopez-Martin N. Percutaneous fixation of displaced proximal humeral fractures: indications based on the correlation between clinical and radiographic results. J Shoulder Elb Surg 2007;16:774-81. [DOI] [PubMed] [Google Scholar]
- 41.Magovern B, Ramsey ML. Percutaneous fixation of proximal humerus fractures. Orthop Clin North Am 2008;39:405-16. [DOI] [PubMed] [Google Scholar]
- 42.Aaron D, Shatsky J, Paredes JC, et al. Proximal humeral fractures: internal fixation. J Bone Jt Surg Am 2012;94:2280-8. [PubMed] [Google Scholar]
- 43.Tamimi I, Montesa G, Collado F, et al. Displaced proximal humeral fractures: when is surgery necessary? Injury 2015;46:1921-9. [DOI] [PubMed] [Google Scholar]
- 44.44. Gupta AK, Harris JD, Erickson BJet al. Surgical management of complex proximal humerus fractures: a systematic review of studies including 4500 patients. J Orthop Trauma 2015;29:54-9. [DOI] [PubMed] [Google Scholar]
- 45.Resch H, Povacz P, Frohlich R, Wambacher M. Percutaneous fixation of three- and four-part fractures of the proximal humerus. J Bone Jt Surg Br 1997;79:295–300. [DOI] [PubMed] [Google Scholar]
- 46.Fenichel I., Oran A, Bursteln G., Perry Pritsch M. Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus: a retrospective study. Int Orthop 2006:30:153-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carbone S, Tangari M, Gumina S, et al. Percutaneous pinning of three- or fourpart fractures of the proximal humerus in elderly patients in poor general condition: MIROS® versus traditional pinning. Int Orthop 2012;36:1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Blonna D, Castoldi F, Scelsi M, et al. The hybrid technique: potential reduction in complications related to pins mobilization in the treatment of proximal humeral fractures. J Shoulder Elb Surg 2010;19:1218-29. [DOI] [PubMed] [Google Scholar]
- 49.Dilisio MF, Nowinski RJ, Hatzidakis AM, Fehringer EV. Intramedullary nailing of the proximal humerus: evolution, technique, and results. J Shoulder Elb Surg 2016;25:e130–8. [DOI] [PubMed] [Google Scholar]
- 50.Rush LV, Rush HC. Intramedullary fixation of the fracture of the humeral shaft by longitudinal pin. Surgery 1950;27,268. [PubMed] [Google Scholar]
- 51.Blum J, Hansen M, Rommens PM. Angle-stable intramedullary nailing of proximal humerus fractures with the proximal humeral nail. Oper Orthop Traumatol 2009;21:296-311. [DOI] [PubMed] [Google Scholar]
- 52.Hessmann MH, Nijs S, Mittlmeier T, et al. Internal fixation of fractures of the proximal humerus with the MultiLoc nail. Oper Orthop Traumatol 2012;24:418-31. [DOI] [PubMed] [Google Scholar]
- 53.Popescu D, Fernandez-Valencia JA, Rios M, et al. Internal fixation of proximal humerus fractures using the T2- proximal humeral nail. Arch Orthop Trauma Surg 2009;129:1239-44. [DOI] [PubMed] [Google Scholar]
- 54.Freynik F, Freynik S, Zenker W, Pflugmacher R. Angular and sliding stable internal fixation of proximal humerus fractures using the “Varion” intramedullary nail. Z Orthop Unfall 2013;151:343-9. [DOI] [PubMed] [Google Scholar]
- 55.Hatzidakis AM, Shevlin MJ, Fenton DL, et al. Angular-stable locked intramedullary nailing of two-part surgical neck fractures of the proximal part of the humerus: a multicenter retrospective observational study. J Bone Jt Surg Am 2011;93:2172-9. [DOI] [PubMed] [Google Scholar]
- 56.Nolan BM, Kippe MA, Wiater JM, Nowinski GP. Surgical treatment of displaced proximal humerus fractures with a short intramedullary nail. J Shoulder Elb Surg 2011;20:1241-7. [DOI] [PubMed] [Google Scholar]
- 57.Lanting B, MacDermid J, Drosdowech D, Faber KJ. Proximal humeral fractures: a systematic review of treatment modalities. J Shoulder Elb Surg 2008;17:42-54. [DOI] [PubMed] [Google Scholar]
- 58.Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults - a systematic review of management. Injury 2011;32:363-72. [DOI] [PubMed] [Google Scholar]
- 59.Edwards SL, Wilson NA, Zhang LQ, et al. Two-part surgical neck fractures of the proximal part of the humerus: a biomechanical evaluation of two fixation techniques. J Bone Jt Surg Am 2006;88:2258-64. [DOI] [PubMed] [Google Scholar]
- 60.Konrad G, Audigé L, Lambert S, et al. Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures. Clin Orthop Relat Res 2012;470:602-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lekic N, Montero NM, Takemoto RC, et al. Treatment of two-part proximal humerus fractures: intramedullary nail compared to to locked plating. HSS J 2012;8:86-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhu Y, Lu Y, Shen J, et al. Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Jt Surg Am 2011;93:159-68. [DOI] [PubMed] [Google Scholar]
- 63.Gradl G, Dietze A, Kaab M, et al. Is locking nailing of humeral head fractures superior to locking plate fixation? Clin Orthop Relat Res 2009;467:2986-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Karataglis D, Stavridis SI, Petsatodis G, et al. New trends in fixation of proximal humeral fractures: a review. Injury 2011;42:330-8. [DOI] [PubMed] [Google Scholar]
- 65.Kitson J, Booth G, Day R. A biomechanical comparison of locking plate and locking nail implants used for fractures of the proximal humerus. J Shoulder Elb Surg 2007;16:362-6. [DOI] [PubMed] [Google Scholar]
- 66.Mihara K, Tsutsui H, Suzuki K, et al. New intramedullary nail for the surgical neck fracture of the proximal humerus in elderly patients. J Orthop Sci 2008;13:56–61. [DOI] [PubMed] [Google Scholar]
- 67.Castoldi F, (Eds.) Simple and complex fractures of the humerus. a guide to assessment and treatment. Springer- Verlag Italia; 2015. [Google Scholar]
- 68.Euler SA, Petri M, Venderley MB, et al. Biomechanical evaluation of straight antegrade nailing in proximal humeral fractures: the rationale of the "proximal anchoring point". Int Orthop. 2017;41:1715-21. [DOI] [PubMed] [Google Scholar]
- 69.Maier D, Jajer M, Strohm PC, Sudkamp NP. Treatment of proximal humeral fractures - a review of current concepts enlightened by basic principles. Acta Chir Othop.et Traum. Čechosl 2012, p.307–16. [PubMed] [Google Scholar]
- 70.Zhang AL, Schairer WW, Feeley BT. Hospital readmissions after surgical treatment of proximal humerus fractures: is arthroplasty safer than open reduction internal fixation? Clin Orthop Relat Res 2014;472:2317-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thanasas C, Kontakis G, Angoules A, et al. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elb Surg 2009;18:837-44. [DOI] [PubMed] [Google Scholar]
- 72.Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury 2011;42:408-13. [DOI] [PubMed] [Google Scholar]
- 73.Kavuri V, Bowden B, Kuman N, Cerynik D. Complications associated with locking plate of proximal humerus fractures. Indian J Orthop 2018;52:108-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jung SW, Shim SB, Kim HM, et al. Factors that influence reduction loss in proximal humerus fracture surgery. J Orthop Trauma 2015;29:276-82. [DOI] [PubMed] [Google Scholar]
- 75.Laux CJ, Grubhofer F, Werner CML, et al. Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res 2017;12:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shukla DR, Mc Anany S, Pean C, et al. The results of tension band rotator cuff suture fixation of locked plating of displaced proximal humerus fractures. Injury 2017;48:474-80. [DOI] [PubMed] [Google Scholar]
- 77.Krappinger Bizzotto N, Riedmann S, et al. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011; 42:1283–8. [DOI] [PubMed] [Google Scholar]
- 78.Kralinger F, Unger S, Wambacher M, et al. The medial periosteal hinge, a key structure in fractures of the proximal humerus – a biomechanical cadaver study of its mechanical properties. J Bone Jt Surg Br 2009;91:973-6. [DOI] [PubMed] [Google Scholar]
- 79.Gardner MJ, Weil Y, Barker JU, et al. The Importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma 2007;21:185–91. [DOI] [PubMed] [Google Scholar]
- 80.Ponce BA, Thompson KJ, Raghava P, et al. The role of medial comminution and calcar restoration in varus collapse of proximal humeral fractures treated with locking plates. J Bone Jt Surg Am 2013;95:e113. [DOI] [PubMed] [Google Scholar]
- 81.Padegimas EM, Zmistowski B, Lawrence C, et al. Defining optimal calcar screw positioning in proximal humerus fixation. J Shoulder Elb Surg 2017;26:1931-37. [DOI] [PubMed] [Google Scholar]
- 82.Badman B, Frankle M, Keating C, et al. Results of proximal humeral locked plating with supplemental suture fixation of rotator cuff. J Shoulder Elb Surg 2011;20:616-24. [DOI] [PubMed] [Google Scholar]
- 83.Frich LH, Jensen NC. Bone properties of the humeral head and resistance to screw cutout. Int J Shoulder Surg 2014;8:21-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bekler H, Bulut G, Usta M, et al. The contribution of locked screw-plate fixation with varying angle configurations to stability of osteoporotic fractures: an experimental study. Acta Orthop Traumatol Turc 2008;42:125-9. [DOI] [PubMed] [Google Scholar]
- 85.Tingart MJ, Lehtinen J, Zurakowski D, et al. Proximal humeral fractures: regional differences in bone mineral density of the humeral head affect the fixation strength of cancellous screws. J Shoulder Elb Surg 2006;15:620-4. [DOI] [PubMed] [Google Scholar]
- 86.Brianza S, Roderer G, Schiuma D, et al. Where do locking screws purchase in the humeral head? Injury, Int. J. Care Injured 2012;43:850-5. [DOI] [PubMed] [Google Scholar]
- 87.Schiuma D, Plecko M, Kloub M, et al. ; Influence of peri-implant bone quality on implant stability. Med Eng Phys. 2013; 35:82-7. [DOI] [PubMed] [Google Scholar]
- 88.Wahnert D, Windolf M, Brianza S., et al. A comparison of parallel and diverging screw angles in the stability of locked plate constructs. J Bone Jt Surg Br 2011;93:1259-64. [DOI] [PubMed] [Google Scholar]
- 89.Schliemann B, Wahnert D, Theisen C., et al. How to enhance the stability of locking plate fixation of proximal humerus fractures? An overview of current biomechanical and clinical data. Injury 2015;46:1207-14. [DOI] [PubMed] [Google Scholar]


