To the Editor:
The highly contagious coronavirus that causes COVID-19 disease is affecting daily clinical practice. The anticipated fast growth in cases has led to development of a regional restructuring model to preserve time-sensitive pathologies in northern Italy. On this way, the Lombardy Region Government built up a big hub-and-spoke model to converge treatment of acute coronary syndrome (ACS) in 13 dedicated centres active 24/7 in the region, implementing availability of intensive care unit beds in general hospitals converted to COVID-19 treatment.1 Our institute is one of the 4 selected hubs in Milan for cardiovascular emergences, therefore, to prevent in-hospital infection spread and to proactively minimize in-hospital patients to exposure risk, we set an internal pathway for ACS, allowing all patients to be timely treated and admitted to isolated intensive care unit or ordinary ward beds, according to nasopharyngeal swab result.
Hospital admissions due to ACS of patients living in the hospital area only, were screened between March 8 and April 10, a period of national lockdown, and compared with the same timeframe in 2019.
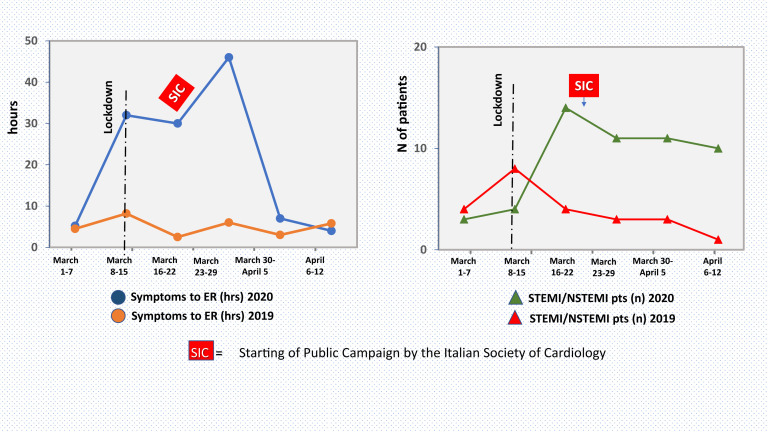
We registered 46 (24 ST-elevation myocardial infarction [STEMI]; 22 non-STEMI [NSTEMI]) admissions compared with 19 (10 STEMI; 9 NSTEMI) in the same 2019 time period, accounting for a 2.5-fold increase in ACS cases (monthly rate 46 vs 18 cases in 2019; Fig. 1 ). A significant delay (> 24 hours) in seeking first medical contact after chest pain onset has been registered in 41% of this year’s STEMI patients (24.8 ± 51 hours) compared with 20% (6.4 ± 6 hours) of last year’s patients, resulting in an in-hospital mortality rate of 38% vs 10%. Among the reasons answering for the late arrival in the emergency room, the fear of being admitted in a potentially infected environment was reported by all of the patients interviewed on admission.
Figure 1.
Left: timing of presentation to emergency room (ER) from chest pain symptom onset during coronavirus 2019 outbreak (blue line) compared with the same time period of 2019 (orange line). Right: number of ST-elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI) cases occurring during coronavirus 2019 outbreak (green line) compared with the same time period of 2019 (red line). hrs, hours; pts, patients; SIC, starting of public campaign by the Italian Society of Cardiology.
Interestingly, after these initial observations, the Italian Society of Cardiology promoted a national campaign to raise public awareness with regard to myocardial infarction symptoms during the outbreak that was followed, at our institute, by a significant decrease in the time from symptoms to emergency room over the past 2 weeks. Additionally, among the NSTEMI cases a higher incidence of myocardial infarction with nonobstructive coronary arteries (45%) was observed compared with 22% in the same timeframe in 2019, reinforcing the inflammatory role of COVID-19 in ACS. Positive nasopharyngeal swab either in COVID-19 symptomatic patients (6 STEMI and 6 NSTEMI) or carriers (10 STEMI and 8 NSTEMI) were observed.
We believe that the hub model planning did not deal with valid apprehension the pandemic triggered and in patients with cardiovascular disease might have led to hesitancy in seeking timely appropriate emergent care. When people’s behaviours are driven by fear, it can lead to decision-making out of line with public health recommendations, thus preventing patients from activating emergency care systems.2 Therefore, on the basis of these observations, we believe an effective strategy in this phase of pandemic outbreak might be the hub-and-spoke model associated with a strong media campaign on the importance of early hospital admission for suspected ACS in a COVID-19-free hospital environment.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy; early experience and forecast during an emergency response. JAMA. 2020;323:1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 2.Antman E.M., Anbe D.T., Armstrong P.W., et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) [erratum in 2005;45:1376] J Am Coll Cardiol. 2004;44:671–719. doi: 10.1016/j.jacc.2004.07.002. [DOI] [PubMed] [Google Scholar]