Highlights
-
•
At least one in five healthcare professionals report symptoms of depression and anxiety.
-
•
Almost four in ten healthcare workers experience sleeping difficulties and/or insomnia.
-
•
Rates of anxiety and depression were higher for female healthcare workers and nursing staff.
-
•
Milder mood symptoms are common and screening should aim to identify mild and sub-threshold syndromes.
Keywords: Coronavirus, COVID-19, Health care workers, Mental health, Depression, Anxiety, Insomnia
Abstract
Background
COVID-19 pandemic has the potential to significantly affect the mental health of healthcare workers (HCWs), who stand in the frontline of this crisis. It is, therefore, an immediate priority to monitor rates of mood, sleep and other mental health issues in order to understand mediating factors and inform tailored interventions. The aim of this review is to synthesize and analyze existing evidence on the prevalence of depression, anxiety and insomnia among HCWs during the Covid-19 outbreak.
Methods
A systematic search of literature databases was conducted up to April 17th, 2020. Two reviewers independently assessed full-text articles according to predefined criteria. Risk of bias for each individual study was assessed and data pooled using random-effects meta-analyses to estimate the prevalence of specific mental health problems. The review protocol is registered in PROSPERO and is available online.
Findings
Thirteen studies were included in the analysis with a combined total of 33,062 participants. Anxiety was assessed in 12 studies, with a pooled prevalence of 23·2% and depression in 10 studies, with a prevalence rate of 22·8%. A subgroup analysis revealed gender and occupational differences with female HCPs and nurses exhibiting higher rates of affective symptoms compared to male and medical staff respectively. Finally, insomnia prevalence was estimated at 38·9% across 5 studies.
Interpretation
Early evidence suggests that a considerable proportion of HCWs experience mood and sleep disturbances during this outbreak, stressing the need to establish ways to mitigate mental health risks and adjust interventions under pandemic conditions.
1. Introduction
Lower respiratory infections remain the communicable disease with the highest mortality worldwide (Murdoch and Howie, 2018). In December 2019, a highly infectious serious acute respiratory syndrome caused by a novel coronavirus (SARS-CoV-2) emerged in Wuhan, China. On March 11th 2020, the World Health Organization (WHO) declared COVID-19 a pandemic (Huang et al., 2020a).
According to previous studies from SARS or Ebola epidemics, the onset of a sudden and immediately life-threatening illness could lead to extraordinary amounts of pressure on healthcare workers (HCWs) (Liu et al., 2012). Increased workload, physical exhaustion, inadequate personal equipment, nosocomial transmission, and the need to make ethically difficult decisions on the rationing of care may have dramatic effects on their physical and mental well-being. Their resilience can be further compromised by isolation and loss of social support, risk or infections of friends and relatives as well as drastic, often unsettling changes in the ways of working. HCWs are, therefore, especially vulnerable to mental health problems, including fear, anxiety, depression and insomnia (Lung et al., 2009, Wu et al., 2009).
Immediate interventions are essential in order to enhance psychological resilience and strengthen the healthcare systems’ capacity (Bao et al., 2020). Clear communication, limitation of shift hours, provision of rest areas as well as broad access and detailed rules on the use and management of protective equipment and specialized training on handling COVID-19 patients could reduce anxiety coming from the perceived unfamiliarity and uncontrollability of the hazards involved. Providing timely and appropriately tailored mental health support through hotline teams, media or multidisciplinary teams, including mental health professionals is also vital (Chen et al., 2020).
Previous reviews have explored the prevalence and factors associated with psychological outcomes in HCWs during past infectious disease outbreaks (Maunder et al., 2004). However, to date, the impact of the current unprecedented crisis on the psychological well-being of medical and nursing staff is yet to be established. The aim of this rapid systematic review and meta-analysis is to examine the emerging evidence of the effects of the COVID-19 outbreak on the mental health of HCW and particularly in relation to the prevalence of anxiety, depression and insomnia.
2. Materials and methods
The systematic review was conducted in accordance with the PRISMA statement (Liberati et al., 2009). The MOOSE (Meta-analyses Of Observational Studies in Epidemiology) Checklist was followed. The review protocol is registered in PROSPERO and is available online (CRD42020180313).
2.1. Research strategy and selection criteria
Our search strategy was generated by consensus among all researchers in the group. Two authors independently identified records published until April 17th 2020 that reported on the prevalence of depression, anxiety, and insomnia in HCWs during the coronavirus pandemic through systematically searching MEDLINE, PubMed and Google Scholar databases. Moreover, due to the rapid dissemination of information during the current pandemic, preprint articles published on Medrxiv and SSRN servers were also included. “Snowball sampling” by searching reference lists and citation tracking was performed in each retrieved article. No language restrictions were applied. If there were queries regarding the methodology or results of the studies under consideration, we attempted to contact the corresponding authors for clarification. Following search terms were used: (“healthcare workers” OR “medical staff” OR “healthcare professionals”) AND (“coronavirus” OR “SARS-COV-2” OR “COVID-19”) AND (“depression” OR “anxiety” OR “insomnia” OR “mental health” OR “psychological”).
The study population group consisted of healthcare workers (medical and non-medical) in COVID-19 affected countries or areas. Only studies evaluating the prevalence rates of depression, anxiety and/or insomnia using validated assessment methods were eligible for inclusion. Broad terms such as ‘psychological distress’ were excluded as they can be difficult to quantify; PTSD was also not excluded as its onset can be delayed.
2.2. Data extraction and quality assessment
The following data were extracted from each article by two reviews independently: study type, total number of participants, participation rate, region, percentage of physicians, nurses and other HCWs screened in the survey, number of male and female participants, assessment methods used and their cut-offs as well as the total number and percentage of participants that screened positive for depression, anxiety or insomnia. If any of this information was not reported, the necessary calculations (e.g. from percentage to number of HCWs) were done, where possible. The accuracy of the extracted or calculated data was confirmed by comparing the collection forms of the two investigators.
In addition, two authors independently evaluated the risk of bias of the included cross-sectional studies using a modified form of the Newcastle-Ottawa scale. Potential disagreements were resolved by a third author. Quality assessment criteria were the following: sample representativeness and size, comparability between respondents and non-respondents, ascertainment of depression, anxiety and insomnia, and adequacy of descriptive statistics. Total quality score ranged between 0 and 5. Studies scoring ≥3 points were regarded as low risk of bias, compared to the studies assessed with <3 points that were regarded as high risk of bias.
2.3. Data synthesis and analysis
For the purposes of the current study, MetaXL (www.epigear.com), an add-in for meta-analysis in Microsoft Excel for Windows was utilized. Due to the fact, that studies with prevalence close to 0 or 1 have affected variance which may lead to a large weight of the study in the meta-analysis, the proportions were transformed using the double arcsine method and then back-transformed for ease of interpretation (Barendregt et al., 2013). Due to the different patient populations, regions, and assessment methods across studies, one true effect size cannot be assumed; therefore, a random effects model (DerSimonian & Laird) was used to extract the pooled prevalence. Substantial heterogeneity was defined as I2 > 75%. Subgroup analysis was done in the following categories: gender, rating scales, severity of depression and anxiety and professional group. Sensitivity analysis was done by subtracting each study and calculating the pooled prevalence of the remaining studies, in order to identify studies which may severely affect the pooled prevalence. Our main outcomes were prevalence (p), confidence intervals (CI) and percentage prevalence (p × 100%).
3. Results
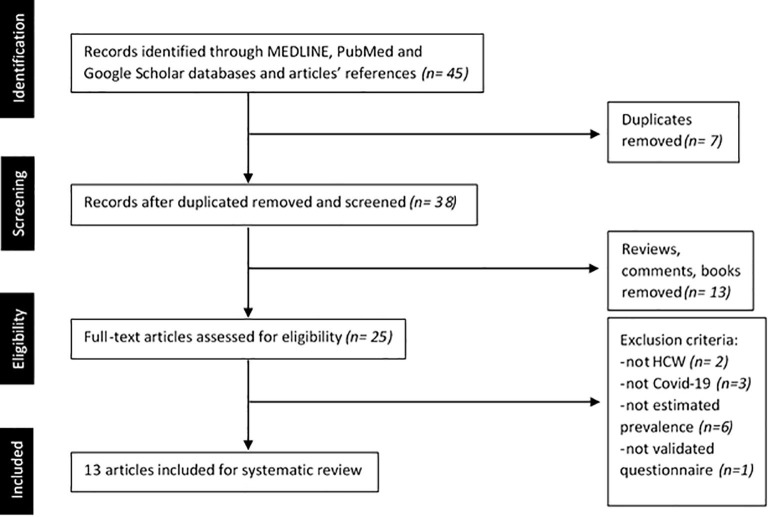
A PRISMA diagram detailing the study retrieval process is shown in Fig. 1 .
Fig. 1.
Flow chart of study selection process.
3.1. Characteristics of included studies
After de-duplication and screening, thirteen studies (Du et al., 2020, Guo et al., 2020, Huang et al., 2020b, Huang and Zhao, 2020, Lai et al., 2020, Liu et al., 2020, Liu et al., 2020, Lu et al., 2020, Qi et al., 2020, Tan et al., 2020, Zhang et al., 2020a, Zhang et al., 2020b, Zhu et al., 2020) with a total of 33,062 participants were included in the analysis. All of the studies were cross-sectional and reported on the prevalence of depression, anxiety or insomnia among HCW during the Covid-19 pandemic. Out of the 13 studies, 12 were undertaken in China, two of which were in Wuhan (Lai et al., 2020, Zhu et al., 2020), while one took place in Singapore (Tan et al., 2020). Median number of individuals per study was 1563 (range 134, 11118) with a median male representation of 18% (281·5/1563) and a median questionnaire participation rate of 85·3% (range 43·2%, 94·88%).
A summary of the characteristics of each study, including the number of participants per study, participation rate, country or region, HCW distribution, male to female ratio and prevalence of each mental health condition are provided in Table 1 . The Newcastle-Ottawa score results for each study are shown in Table 2 . The resulting pooled prevalence of anxiety, depression and insomnia as well as the subgroup analyses are presented below. Notably, I2 was over 75% in the vast majority of the results; if I2 was close to 100% or 0% two decimals were used.
Table 1.
Summary of characteristics of included studies.
| Author | Study Population | Response rate (%) | Region | Health care workers |
Male% | Assessment | Cut-off | Outcomes |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physicians | Nurses | Other | Depression% (n) | Anxiety% (n) | Insomnia% (n) | |||||||
| Du et al. (2020) | 134 | 43·2% | China | 35·1% | 41·0% | 23·9% | 39·6% | BDI-II BAI |
≥14 ≥8 |
12·7% (17) |
20·1% (28) |
N.A. |
| Guo et al. (2020) | 11,118 | N.A. | China | 30·28% | 53·07% | 16·65% | 25·2% | SAS SDS |
≥50 ≥50 |
31·45% (3497) |
17·45% (1940) |
N.A. |
| Huang et al. (2020a) | 230 | 93·5% | Fuyang | 30·4% | 69·6% | 0·0% | 18·7% | SAS | ≥50 | N.A. | 23·04% (53) |
N.A. |
| Huang and Zhao (2020) | 2250 | 85·3% | China | N.A. | N.A. | N.A. | N.A. | CES-D GAD-7 |
≥28 ≥9 |
19·8% (446) |
35·6% (802) |
23·6% (531) |
| Lai et al. (2019) | 1257 | 68·7% | Wuhan | 39·2% | 60·8% | 0·0% | 23·3% | GAD-7 ISI PHQ-9 |
≥5 ≥8 ≥5 |
50·4% (634) |
44·6% (560) |
34% (427) |
| Liu et al. (2020) | 512 | 85·3% | China | N.A. | N.A. | N.A. | 15·4% | SAS | ≥50 | N.A. | 12·5% (64) |
N.A. |
| Liu et al. (2020) | 4679 | N.A. | China | 39·6% | 60·4% | 0·0% | 17·7% | SAS SDS |
≥50 ≥50 |
34·6% (1619) |
16·0% (749) |
N.A. |
| Lu et al. (2020) | 2299 | 94·88% | Fujian | 88·8% | 11·2% | 22·4% | HAMA HAMD |
≥7 ≥7 |
11·7% (268) |
24·7% (569) |
N.A. | |
| Qi et al. (2020) | 1306 | 93·6% | China | N.A. | N.A. | N.A. | 19.6% | AIS PSQI |
>6 >7 |
N.A. | N.A. | 45·5% (594) |
| Tan et al. (2020) | 470 | 94·0% | Singapore | 28·7% | 34·3% | 37·0% | 31·7% | DASS-21 | D > 9 A > 7 |
8·9% (42) |
14·5% (68) |
N.A. |
| Zhang et al. (2020a) | 1563 | N.A. | China | 29·0% | 62·9% | 7·9% | 17·3% | GAD-7 ISI PHQ-9 |
≥5 ≥8 ≥5 |
50·7% (792) |
44·7% (699) |
36·1% (564) |
| Zhang et al. (2020b) | 2182 | N.A. | China | 31·2% | 11·3% | 57·5% | 35·8% | ISI GAD-2 PHQ-2 |
>8 ≥3 ≥3 |
10·6% (232) |
10·4% (228) |
33·9% (739) |
| Zhu et al. (2020) | 5062 | 77·1% | Wuhan | 19·8% | 67·5% | 12·7% | 15% | GAD-7 PHQ-9 |
≥8 ≥10 |
13·45% (681) |
24·06% (1218) |
N.A. |
All studies are cross-sectional; the absolute number of patients for each category is included in the brackets.
Table 2.
Modified Newcastle-Ottawa quality assessment scale and total score of each study.
| Studies | Year | Modified Newcastle-Ottawa quality assessment scale |
Score | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||
| Author | 2020 | – | – | – | * | * | 2 |
| Guo et al. (2020) | 2020 | * | * | – | – | – | 2 |
| Du et al. (2020) | 2020 | – | – | * | * | – | 2 |
| Huang and Zhao (2020) | 2020 | – | * | * | * | * | 4 |
| Lai et al. (2019) | 2020 | * | * | – | * | * | 4 |
| Liu et al. (2020) | 2020 | – | – | * | * | * | 3 |
| Liu et al. (2020) | 2020 | * | * | – | – | * | 3 |
| Lu et al. (2020) | 2020 | – | * | * | * | – | 3 |
| Qi et al. (2020) | 2020 | – | * | * | * | * | 4 |
| Tan et al. (2020) | 2020 | * | – | * | * | * | 4 |
| Zhang et al. (2020a) | 2020 | * | * | – | * | * | 4 |
| Zhang et al. (2020b) | 2020 | – | * | – | * | * | 3 |
| Zhu et al. (2020) | 2020 | – | * | – | * | * | 3 |
1. Representativeness of sample (no HCWs’ subgroup ≥ 65% of total sample); 2. Sample size > 600 HCWs; 3. Response rate > 80%; 4. The study employed validate measurement tools with appropriate cut-offs; 5. Adequate statistics and no need for further calculations.
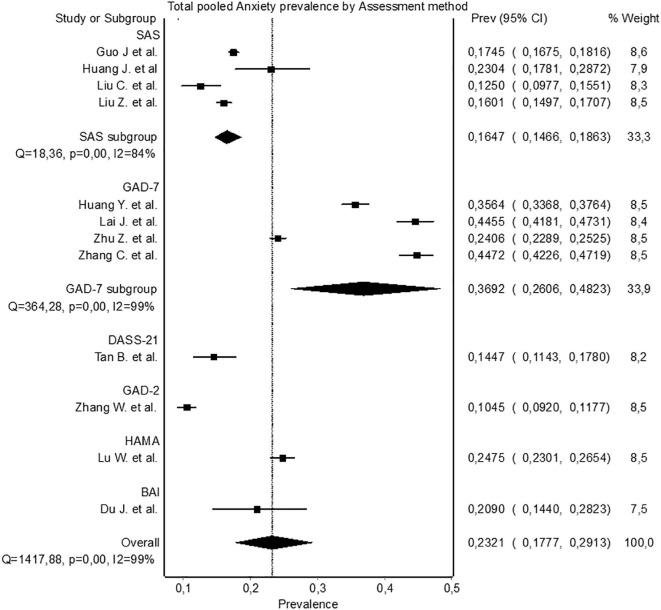
3.2. Anxiety prevalence
Anxiety was estimated in 12 studies (Du et al., 2020, Guo et al., 2020, Huang et al., 2020b, Huang and Zhao, 2020, Lai et al., 2020, Liu et al., 2020, Liu et al., 2020, Lu et al., 2020, Tan et al., 2020, Zhang et al., 2020a, Zhang et al., 2020b, Zhu et al., 2020). The pooled prevalence was 23·21% (95% CI 17·77-29·13, I2 = 99%) as presented in Fig. 2 . In sensitivity analysis, no study affected the pooled prevalence by over 2% when excluded. Furthermore, low risk of bias studies (n = 9) revealed a total pooled anxiety prevalence of 24·06% (95% CI 16·84-32·09, I2 = 99%).
Fig. 2.
Pooled anxiety prevalence by assessment method.
Regarding assessment methods, four studies (Guo et al., 2020, Huang et al., 2020b, Liu et al., 2020, Liu et al., 2020)used the Zung Self-Rating Anxiety Scale (SAS) with a pooled prevalence of 16·47% (95% CI 14·66-18·63, I2 = 84%) and four studies (Huang and Zhao, 2020, Lai et al., 2020, Zhang et al., 2020a, Zhu et al., 2020) used the GAD-7 scale with a pooled prevalence of 36·92% (95% CI 26·06-48·23, I2 = 99%). Each of the four remaining studies used a different questionnaire.
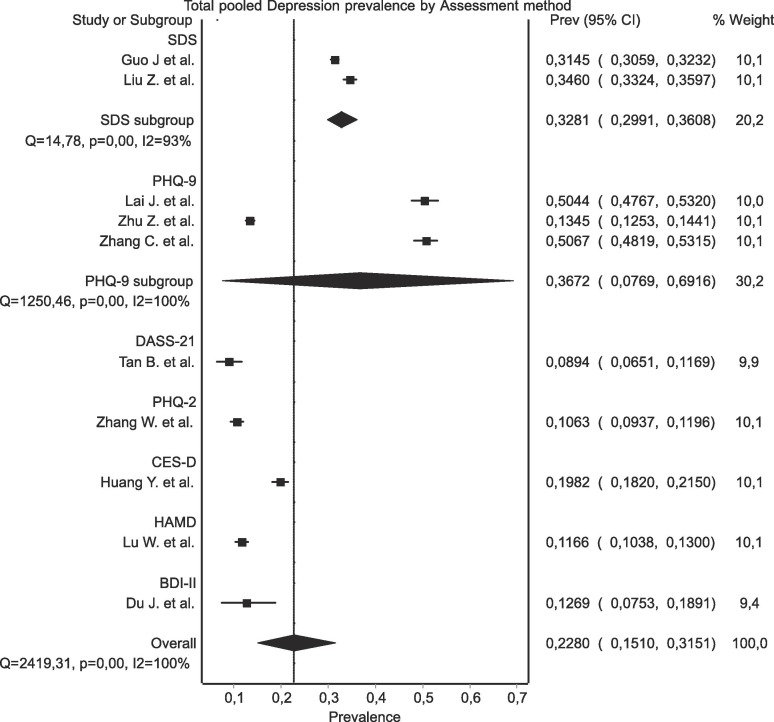
3.3. Depression prevalence
Depression was assessed in 10 (Du et al., 2020, Guo et al., 2020, Huang and Zhao, 2020, Lai et al., 2020, Liu et al., 2020, Lu et al., 2020, Tan et al., 2020, Zhang et al., 2020a, Zhang et al., 2020b, Zhu et al., 2020) out of 13 studies, with a calculated pooled prevalence of 22·8% (95% CI 15·1-31·51, I2 = 99·62), as shown in Fig. 3 . None of the other studies affected the outcome by over 2%, except Lai et al. (2020) and Zhang et al. (2020a); when both were excluded, the recalculated pooled prevalence was 16·94% (95% CI, 10·38-24·67, I2 = 99·56%). Among low risk of bias studies (n = 8) the pooled prevalence was 22·93% (95% CI 13·16–34·38).
Fig. 3.
Pooled depression prevalence by assessment method.
Two studies (Guo et al., 2020, Liu et al., 2020) used the Zung Self-Rating Depression Scale (SDS) with a pooled prevalence of 32·81 (95% CI 29·91–36·08, I2 = 93%). Three (Lai et al., 2020, Zhang et al., 2020a, Zhu et al., 2020) studies used the PHQ-9 score for which the pooled prevalence was 36·72 (95% CI 7·69–69·16, Ι2 = 100%); although Zhu et al. (2020) applied a significantly higher-cut off score (10 compared to 5 used by Zhang et al. (2020a) and Lai et al. (2020). The remaining studies used a variety of different tools.
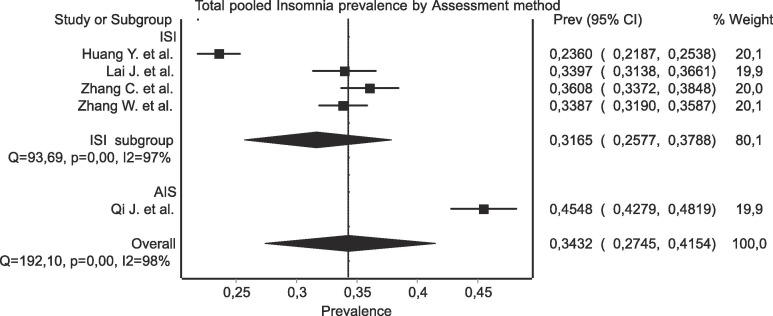
3.4. Insomnia prevalence
Insomnia prevalence was estimated in five (Huang and Zhao, 2020, Lai et al., 2020, Qi et al., 2020, Zhang et al., 2020a, Zhang et al., 2020b) out of the 13 retrieved studies (Fig. 4 ). The pooled prevalence was calculated as 34·32% (95% CI 27·45–41·54, I2 = 98%). In sensitivity analysis, no study affected the pooled prevalence by over 3% when excluded. The risk of bias was deemed as low for all five studies.
Fig. 4.
Pooled insomnia prevalence by assessment method.
3.5. Subgroup analysis
A subgroup analysis of the prevalence of anxiety and depression by gender, severity and professional group was further conducted and summarized in Table 3 .
Table 3.
Subgroup analysis of Anxiety and Depression Prevalence.
| Anxiety | Depression | ||
|---|---|---|---|
| Gender |
Female |
29·06% 95% CI 20·21-38·78 I2 = 99% |
26·87% 95% CI 15·39-40·09 I2 = 99·56% |
| Male |
20·92% 95% CI 11·86-31·65 I2 = 98% |
20·34% 95% CI 11·57-30·75 I2 = 98% |
|
| Severity | Mild |
17·93% 95% CI 11·33-25·62 I2 = 99% |
24·60% 95% CI 16·65 – 33·51 I2 = 99% |
| Moderate/severe |
6·88% 95% CI 4·39-9·87 I2 = 97% |
16·18% 95% CI 12·80-19·87 I2 = 97% |
|
| HCW group | Doctors |
21·73% 95% CI 15·27-28·96 I2 = 97% |
25.37% 95% CI 16·63-35.20 I2 = 98% |
| Nurses |
25·80% 95% CI 19·20-33·00, I2 = 98% |
30.30% 95% CI 18·24-43.84 I2 = 99·52% |
|
For anxiety, gender data were available in six studies, with a pooled prevalence of 20.92% for males and 29·06% for females (Du et al., 2020, Guo et al., 2020, Huang and Zhao, 2020, Lai et al., 2020, Liu et al., 2020, Liu et al., 2020). In doctor and nurse groups, prevalence could be calculated in six studies, with respective values of 21·73%and 25·80% (Du et al., 2020, Guo et al., 2020, Lai et al., 2020, Liu et al., 2020, Liu et al., 2020, Lu et al., 2020). Regarding the severity of the anxiety, data were available in six studies with a pooled prevalence of 17·93% for mild anxiety and 6·88% for moderate/severe (Du et al., 2020, Lai et al., 2020, Liu et al., 2020, Lu et al., 2020, Qi et al., 2020, Tan et al., 2020). Furthermore, in five studies men had a pooled depression prevalence of 20·34% whereas in women the respective value was 26·87% (Du et al., 2020, Guo et al., 2020, Huang and Zhao, 2020, Liu et al., 2020, Liu et al., 2020). Between doctors and nurses, in the five studies with available data on depression, the pooled prevalence was calculated as 30.30% for nurses and 25.37% for doctors (Du et al., 2020, Guo et al., 2020, Liu et al., 2020, Liu et al., 2020, Lu et al., 2020). Prevalence of depression by severity could be calculated in four (Du et al., 2020, Liu et al., 2020, Lu et al., 2020, Tan et al., 2020)studies, with respective values for mild and moderate/severe of 24·60% and 16·18%.
For insomnia, a subgroup analysis was not performed due to the limited data available.
4. Discussion
A recent position paper in The Lancet (Holmes, 2020), called for high-quality data on the mental health effects of the COVID-19 pandemic across the whole population and vulnerable groups such as health care professionals.
This timely rapid systematic review and meta-analyses of 13 cross-sectional studies and a total of 33,062 participants provides early evidence that a high proportion of healthcare professionals experience significant levels of anxiety, depression and insomnia during COVID-19 pandemic. We are mindful that mental health research in times of crisis, such as COVID-19 outbreak, is a sensitive topic and would like to believe that all the studies included were given due ethical consideration (Townsend et al., 2020).
The prevalence rates of anxiety and depression (23·2% and 22·8% respectively) of HCWs during COVID-19 are broadly comparable to the respective rates, ranging between 22·6%-36·3% for anxiety and 16·5%-48·3% for depression, reported for the general population in China during the same period, which shows the considerable effect of the crisis on the whole of the population (Wang et al., 2020, Gao et al., 2020, Wang et al., 2020). Our results are also at the lower end of the outcomes previously reported among HCWs during and after the MERS and SARS epidemics where high rates of depression and anxiety as well as post-traumatic stress disorder (PTSD) and moral injury were observed (Lancee et al., 2008, Tam et al., 2004, Lee et al., 2018, Koh et al., 2005). Potential differences, however, between these outbreaks and the COVID-19 pandemic could be explained on the basis of the extremely high infectious potential and mortality rate of the former but also the experience acquired in the interim in these areas.
Although, the different scales and cut-off scores adopted by each survey possibly introduced great between-study heterogeneity, it appears that the majority of the HCWs experienced mild symptoms both for depression and anxiety, while moderate and severe symptoms were less common among the participants. In our view this emphasizes the need for early detection and the importance of picking up and effectively treating the milder clinical mood symptoms or sub-threshold syndromes before they evolve to more complex and enduring psychological responses.
Furthermore, our sub-analysis revealed potentially important gender and occupational differences. The prevalence rate of anxiety and depression appeared to be higher in females, which probably reflects the already established gender gap for anxious and depressive symptoms (Albert, 2015). Again, nursing staff exhibited higher prevalence estimates both for anxiety and depression compared to doctors. These results may be partly confounded by the fact that nurses are mostly female but could be also attributed to the fact they may face a greater risk of exposure to COVID-19 patients as they spend more time on wards, provide direct care to patients and are responsible for the collection of sputum for virus detection (Liu et al., 2020). Moreover, due to their closer contact with patients they may be more exposed to moral injury pertaining to suffering, death and ethical dilemmas.
Although they were not suitable for inclusion in this review, a number of other studies published in recent weeks provide emerging evidence that COVID-19 is severely affecting the wellbeing of healthcare professionals. In Hong Kong, medical and nursing staff were found vulnerable to burnout, anxiety and mental exhaustion (Cheung et al., 2020) and in Germany doctors reported high levels of anxious and depressive symptoms (Bohlken et al., 2020). Moreover, the psychological impact of the crisis is not only felt by frontline respiratory and intensive care physicians and nurses but also by HCW of other specialties including, for example, surgeons and anesthesiologists (Xu et al., 2020). Sadly, there have been also reports of suicides, as health care professionals are faced with accumulated psychological pressure and intense fear of dying (Montemurro, 2020, Papoutsi et al., 2020); this is particularly alarming given the fact that physicians are already at an increased risk of suicide compared to the general population (West et al., 2018). A study exploring factors related to HCWs’ psychological difficulties found that infection of colleagues, infection of family members, protective measures and medical violence (Dai et al., 2020, Liu et al., 2020) were among the main concerns of HCWs in COVID-19 affected areas. Unsurprisingly, level of social support was found to positively correlate with self-efficacy and sleep quality and negatively with anxiety and stress (Xiao et al., 2020).
To this end, early, targeted interventions should be considered. Of relevance, another study performed in the original center of the epidemic, Wuhan, showed that a large proportion of HCW in Wuhan were affected and that mental health support was necessary even for mild psychological reactions (Kang et al., 2020). Indeed, much can be offered in the current context, such as virtual clinics, remotely delivered psychological therapies and psycho-education, chat lines, digital phenotyping and technologies monitoring risk. Finally, alongside infected patients and HCWs, suspected cases, who are home isolated, and families and friends of affected people have to be supported, too (The Lancet Psychiatry, 2020).
Nevertheless, there are several strenghts and key limitations to our review. To our knowledge, this is the first systematic review and meta-analysis to examine the pooled prevalence of depression, anxiety and insomnia on HCW during the COVID-19 outbreak. Although, the number of studies per se included in our meta-analysis was as expected in the early stages of the pandemic still relatively low, the majority of studies comprised a considerable number of participants. Furthermore, our subgroup analysis of anxiety and depression based on gender, professional group and severity provided additional valuable insights of potential particular vulnerabilities.
One major drawback that merits consideration is the inherent heterogeneity across studies. Different assessment scales were utilized for population screening and different cut offs set even though several studies used the same tests. Thus, threshold criteria for case definition varied with some investigators intentionally using more lenient criteria in order to capture milder or subsyndromal cases; hence our subgroup analysis by severity. Another limitation is that several studies might have included the same population as they were broadly conducted in the same region/country. Again, as the majority of studies were conducted in China, the generalizability of our findings may be limited. Having said that, generalizing this type of results could pose severe flaws as healthcare systems vary greatly between countries. Nevertheless, considering the fact that China was severely affected, they provide a reliable indication of the potential of COVID-19 pandemic to affect the mental health of HCWs. Furthermore, the studies included in our meta-analysis were all cross-sectional, thus the long-term implications of COVID-19 pandemic on HCW’s mental health warrant further research.
In conclusion, our systematic review and meta-analysis provide a timely and comprehensive synthesis of the existing evidence highlighting the high prevalence rates of depression, anxiety and insomnia of healthcare professionals. Findings can help to quantify staff support needs and inform tiered and tailored interventions under pandemic conditions that enhance resilience and mitigate vulnerability.
Contributors
PK, SP, EP, VGG, VN and TG designed the study.
PK, SP, EP, VGG, VN and TG did the literature search.
VGG and EP have done the systematic review analysis
VGG, EP, VN, and TG created the first draft of the manuscript.
SP and PK suggested improvements
SP created the second draft and reviewed the manuscript
EP, VN and TG created the tables
PK supervised the publication and reviewed the manuscript
SP and VN contributed equally to this work
Declaration of interests
SP and PK report grants and personal fees outside the submitted work.
VN, TG, VGG, EP have nothing to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbi.2020.05.026.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Albert P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015;40:219–221. doi: 10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barendregt J.J., Doi S.A., Lee Y.Y., Norman R.E., Vos T. Meta-analysis of prevalence. J. Epidemiol. Commun. Health. 2013;67:974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- Bohlken J., Schömig F., Lemke M.R., Pumberger M., Riedel-Heller S.G. COVID-19 pandemic: stress experience of healthcare workers – a short current review. Psychiatr. Prax. 2020;47:190–197. doi: 10.1055/a-1159-5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung T., Fong T.K.H., Bressington D. COVID-19 under the SARS Cloud: Mental Health Nursing during the Pandemic in Hong Kong. J. Psychiatr. Ment. Health Nurs. 2020:jpm.12639. doi: 10.1111/jpm.12639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Y., Hu G., Xiong H., Qiu H., Yuan X. Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. medRxiv. 2020 2020.03.03.20030874. [Google Scholar]
- Du J., Dong L., Wang T. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatry. 2020 doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Liao L., Wang B. Psychological effects of COVID-19 on hospital staff: a national cross-sectional survey of china mainland. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3550050. [DOI] [Google Scholar]
- Holmes E.A. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y, Zhao, N., 2020. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 epidemic in China: a web-based cross-sectional survey 2 3. doi:10.1101/2020.02.19.20025395. [DOI] [PMC free article] [PubMed]
- Huang J.Z., Han M.F., Luo T.D., Ren A.K., Zhou X.P. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:E001. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh D., Meng K.L., Sin E.C. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: What can we learn? Med. Care. 2005;43:676–682. doi: 10.1097/01.mlr.0000167181.36730.cc. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee W.J., Maunder R.G., Goldbloom D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008;59:91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339 doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Han B., Jiang R. Mental health status of doctors and nurses during COVID-19 epidemic in China. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3551329. [DOI] [Google Scholar]
- Liu X., Kakade M., Fuller C.J. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry. 2012;53:15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Yang J., Liu Q. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Heal. 2020 doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Yang Y., Zhang X.M., Xu X., Dou Q.-L., Zhang W.-W. The prevalence and influencing factors for anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. medRxiv. 2020 doi: 10.1017/S0950268820001107. 2020.03.05.20032003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lung F.W., Lu Y.C., Chang Y.Y., Shu B.C. Mental symptoms in different health professionals during the SARS attack: a Follow-up study. Psychiatr. Q. 2009;80:107–116. doi: 10.1007/s11126-009-9095-5. [DOI] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Rourke S. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004;66:938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- Montemurro N. The emotional impact of COVID-19: From medical staff to common people. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murdoch D.R., Howie S.R.C. The global burden of lower respiratory infections: making progress, but we need to do better. Lancet Infect. Dis. 2018;18:1162–1163. doi: 10.1016/S1473-3099(18)30407-9. [DOI] [PubMed] [Google Scholar]
- Papoutsi, E., Giannakoulis, V., Ntella, V., Pappa, S., Katsaounou, P., 2020. Global burden of COVID-19 pandemic on healthcare workers. ERJOR (accepted). [DOI] [PMC free article] [PubMed]
- Qi J., Xu J., Li B. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. medRxiv. 2020 doi: 10.1016/j.sleep.2020.05.023. 2020.03.06.20031278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam C.W.C., Pang E.P.F., Lam L.C.W., Chiu H.F.K. Severe acute respiratory syndrome (SARS) in Hongkong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34:1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- Tan B.Y.Q., Chew N.W.S., Lee G.K.H. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020 doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet Psychiatry Isolation and inclusion. Lancet Psychiatry. 2020;7:371. doi: 10.1016/S2215-0366(20)30156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend E., Nielsen E., Allister R., Cassidy S.A. Key ethical questions for research during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:381–383. doi: 10.1016/S2215-0366(20)30150-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West C.P., Dyrbye L.N., Shanafelt T.D. Physician burnout: contributors, consequences and solutions. J. Intern. Med. 2018;283:516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- Wu P., Fang Y., Guan Z. The psychological impact of the SARS epidemic on hospital employees in china: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009 doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Xu Q.hui, Wang C.ming, Wang J. Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W., Wang K., Yin L. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020:1–9. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Yang L., Liu S. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z., Xu S., Wang H. COVID-19 in Wuhan: immediate psychological impact on 5062 health workers. medRxiv. 2020;02(20):20025338. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.