Abstract
We report a case of a 59-year-old man with coronavirus disease 2019 (COVID-19). He had visited a hospital for fever and cough and been treated with antibiotics for pneumonia in the right upper lobe. However, he gradually progressed to dyspnea and consulted our hospital. His chest radiographs showed bilateral pneumonia shadows and his CT showed ground glass opacities and consolidation. Although we treated him with broad-spectrum antibiotics, the pneumonia shadow rapidly progressed and mechanical ventilation was administered. We collected sputum from the bronchus using bronchoscopy to detect microorganisms, and RT-PCR tests confirmed COVID-19 pneumonia. He was transferred to a designated hospital.
In order to prevent the occurrence of nosocomial infections, close contacts within the hospital and medical staff were suspended from their work for two weeks. No secondary infection with COVID-19 appeared. This was the first case of COVID-19 occurring as community-acquired pneumonia in Hokkaido, Japan.
Keywords: SARS-CoV-2, New coronavirus pneumonia, Steroid treatment, COVID-19, Nosocomial infection
1. Introduction
Since December 2019, numerous cases of pneumonia with coronavirus disease 2019 (COVID-19) have been reported from Wuhan in the Hubei province in China [1,2]. To date, this novel coronavirus infection has spread widely from China to many countries. On 15 January, 2020, the Ministry of Health, Labour and Welfare, Japan reported the first case of laboratory-confirmed COVID-19, imported from Wuhan [3]. Information is now being updated constantly and more than 1000 patients with COVID-19 had been reported in Japan by March 2020 [3,4]. Several reports describe patients with COVID-19 pneumonia showing clinical symptoms such as fever, fatigue, or dry cough. In many cases, symptoms are mild. However, several reports point to severe cases which developed acute respiratory distress syndrome and life threatening events [5,6].
Here, we report the first case of community-acquired pneumonia due to COVID-19 in the Hokkaido prefecture, Japan. Moreover, in order to prevent nosocomial infections, hospital, and medical stuff who had close contact with the patient were suspended from work for two weeks.
2. Case
A 59-year-old Japanese man visited a hospital with a fever of 37 °C and dry cough for 4 days. He had smoked 20 cigarettes a day between the ages of 20 and 40. He had previously been treated for hypertension, hyperlipidemia, hyperuricemia, diabetes mellitus, and sleep apnea syndrome at this hospital. He did not have a history of recent travel to any foreign countries, including China.
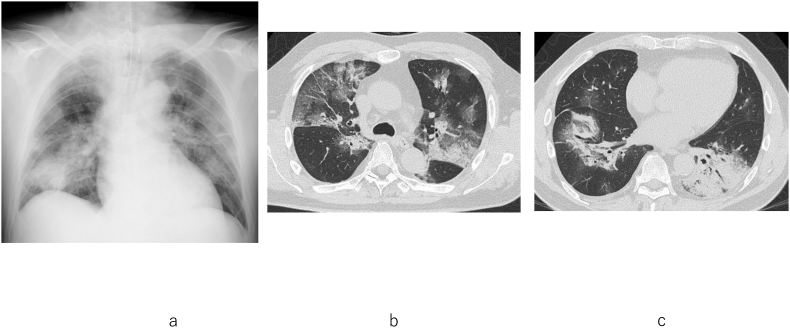
His chest radiograph showed infiltrative shadow in the right upper lung field (Fig. 1a). Computed tomography (CT) imaging showed consolidation and ground glass opacities (GGO) in the central area of the right upper lobe (Fig. 1b). Small GGO (arrow) were found in the subpleural area of the left lower lobe (Fig. 1c). Rapid antigen tests for influenza and mycoplasma were negative. Laboratory data showed normal white blood cell counts with a decrease in the lymphocyte population and an increase in the serum level of C-reactive protein (CRP). He was diagnosed with community-acquired pneumonia and received intravenous administration of 2 g ceftriaxone for a day and 500 mg oral azithromycin for 3 continuous days. Next, 400 mg garenoxacin was administered. As the patient began to suffer from dyspnea and fever, he consulted our hospital 7 days after the first hospital visit.
Fig. 1.
At disease onset, chest radiograph showed consolidation in right upper lung field (a) and CT showed consolidation at the central area of the right upper lobe (b). In addition, there were small ground glass opacities (arrow) at the subpleural area in the left lower lobe (c).
At our hospital, his body temperature was 37.5 °C, blood pressure was 120/53 mmHg, and arterial oxygen saturation was 93% (O2 8L/min, mask). Laboratory data showed increased white blood cell counts with an increase of neutrophils and further increases of serum CRP and lactose dehydrogenase levels (Table 1). His chest radiograph showed bilateral pneumonia shadows (Fig. 2a). The CT showed GGO in both upper lobes and consolidation with air-bronchogram in the left lower lobe and subpleural non-segmental consolidation in the right lower lobe (Fig. 2b and c). Mild contraction was found in the right upper lobe lesions (Fig. 2c). Chest CT findings were markedly deteriorated compared with those taken at the previous hospital.
Table 1.
Laboratory findings.
| On admission | Units | On admission | Units | On admission | |||
|---|---|---|---|---|---|---|---|
| WBC | 11510 | /uL | TP | 6.9 | g/dL | proteinure | 2+ |
| Neut | 92.2 | % | Alb | 3.2 | g/dL | urinary sugar | – |
| AST | 107 | U/L | |||||
| ALT | 106 | U/L | Streptococcus pneumonia antigen | – | |||
| eosino | 0.2 | % | LDH | 635 | U/L | Legionella antigen | – |
| baso | 0.2 | % | CPK | 107 | U/L | Influenza test | – |
| mono | 2.7 | % | BUN | 23.7 | mg/dL | Mycoplasma antigen | – |
| Lym | 4.7 | % | Cr | 1.5 | mg/dL | ||
| RBC | 524 | ×104uL | UA | 3.8 | mg/dL | ANA | – |
| Hb | 15.6 | g/dL | Na | 145 | mEq/L | MPO-ANCA | – |
| Hct | 46.4 | % | K | 4 | mEq/L | PR3-ANCA | – |
| Plt | 21.6 | ×103uL | Cl | 109 | mEq/L | ||
| HbA1c | 6.6 | % | |||||
| CRP | 31.59 | mg/dL | |||||
| BNP | 46.5 | pg/ml |
Fig. 2.
On admission, chest radiograph showed bilateral infiltrative shadows in the lungs (a). Chest CT on admission to our hospital showed extensive ground glass opacities in both lungs and consolidation with air-bronchogram in the left lower lobe and subpleural non-segmental consolidation in right lower lobe (b,c). Mild contraction was found in the right upper lobe lesions (arrow).
We suspected acute interstitial pneumonia, cryptogenic organizing pneumonia, or severe bacterial pneumonia. After admission, intravenous administration of 200 mg/day minocycline, 3 g/day meropenem, and 250 mg methyl prednisolone was initiated. On the second day in hospital, acute respiratory failure developed with a high fever of 38.7 °C. We intubated the patient and started mechanical ventilation, and successfully increased the dose of methyl prednisolone to 1000 mg/day. Although the fever continued, the chest radiograph showed an improvement in the consolidations (Fig. 3). The PaO2/FiO2 ratio gradually improved from 70 to 180. On the fourth day we examined intrabronchial sputum taken by bronchoscopy in order to detect microorganisms, and real-time reverse-transcriptase-polymerase chain reaction (RT-PCR) tests confirmed COVID-19 pneumonia. The patient was transferred to a designated hospital.
Fig. 3.

On the transferred day, the chest radiograph showed an improvement in the consolidations.
In order to prevent nosocomial infection, we checked contacts within our hospital and medical staff and classified them into four levels depending on their extent of contact to the patient as follows:
Level 1: medical staff who assisted with intubation, tracheal suction, or bronchoscopy without a N95 mask and other personal protective equipment (PPE).
Level 2: medical staff who performed oral care or directly took care of the patient without PPE except for Level 1.
Level 3: medical staff who directly touched the patient except for Level 1 and 2.
Level 4: hospital and medical staff who were involved in the patient's care except for Level 1, 2, and 3.
Staff classified as Level 1 were checked with nasal swabs and suspended from work for two weeks, and required to report their general condition, including body temperature and respiratory symptoms, twice a day. Staff classified as Level 2 were suspended from work for two weeks and required to record their general condition twice a day. Staff classified as Level 3 and 4 were able to work but required to record their general condition twice a day. As a result, there were 60 staff judged as contacts; in Level 1, 2, 3 and 4 there were 6, 9, 38, and 7 staff members, respectively. Levels 1 and 2 staff were required to report to the infection control section and Levels 3 and 4 to their director if a fever of ≥37.5 °C or respiratory symptoms appeared. No secondary infections with COVID-19 appeared in our staff after two weeks.
3. Discussion
Today, the outbreak of COVID-19 in Wuhan, Hubei Province, China has spread from a regional epidemic to become a worldwide pandemic in the last three months. Up until March 22, 2020, 162 cases had been diagnosed in Hokkaido [7]. However, only one case had been diagnosed in Hokkaido when this patient presented to our hospital. At that time, patients were suspected as having the new coronavirus infection only when they had stayed in Wuhan or had contact with confirmed cases.
This was the first case of COVID-19 as community-acquired pneumonia in Hokkaido. Based on the results of blood tests, the patient was negative for collagen disease and vasculitis. The causative microorganism of pneumonia could not be identified. However, the patient's lung lesions were rapidly expanding, and testing for novel coronavirus infection was indicated, even without travel history to foreign countries or an identified case contact. Finally, he was treated with mechanical ventilation because of acute respiratory failure. RT-PCR test of intrabronchial sputum confirmed the diagnosis of COVID-19.
CT findings of COVID-19 pneumonia commonly demonstrate GGO, increased crazy-paving pattern, or consolidation [8]. They are known to change rapidly over a short time course. A study of the changes in chest CT findings associated with COVID-19 pneumonia showed that pneumonia mostly worsened approximately 10 days after initial diagnosis [8]. In this case, consolidation and GGO was observed on the right upper lobe on the 5th day after onset, but these lesions extensively spread in both lungs on the 12th day after onset. Chest CT findings of COVID-19 pneumonia are reportedly varied [9,10] and it was thought to be difficult to suspect COVID-19 pneumonia without travel history to foreign countries or apparent contacts with confirmed cases.
Although antibiotics including ceftriaxone, azithromycin, garenoxacin, minocycline, and meropenem were administered for several days, the patient's dyspnea, and hypoxia progressed and respiratory failure worsened. We suspected not only infectious pneumonia but acute interstitial pneumonia, developing to acute respiratory failure. We started high dose methyl prednisolone treatment and supported the patient with mechanical ventilation. His respiratory status and radiography did not worsen after high dose steroid treatment. However, we could not evaluate the efficacy of steroid treatment, because he was transferred to a designated hospital after diagnosis. We believe systemic corticosteroid treatment should not be used for treatment of COVID-19 pneumonia as reported by Russell et al. [11].
At present, treatment for COVID-19 has not been established. We think it important to diagnose moderate to severe cases of COVID-19 in community-acquired pneumonia cases, applying RT-PCR tests for definitive diagnosis and separating them from other people. In addition, differential diagnosis of viral pneumonia by CT images may be useful.
Based on reports that the risk of infection diminishes after 14 days [12], we determined that the patient's close contacts should stop working for 14 days. However, it is unclear that suspension from work for two weeks is adequate to determine infected individuals. Lan et al. [13] reported that recurrent viral activity might occur. Isolation of contacts, asymptomatic carriers, and mild patients from hospital staff is thought to be important to prevent nosocomial transmission of COVID-19.
Declaration of competing interest
No conflict of interest.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet 395(10223),470-473. [DOI] [PMC free article] [PubMed]
- 2.Chan J.F., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 Feb 15;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. PMID 31986261, Epub 2020 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Novel Coronavirus-Japan (ex-China). Geneva: World Health Organaization. https://www.who.int/csr/don/17-january-2020-novel-coronavirus-japan-ex-china/en/ Jan 17,2020.
- 4.WHO Coronavirus disease (COVID-2019) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports situation reports.
- 5.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. Epub 2020 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J. Am. Med. Assoc. 2020 Feb 7 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Outbreak of the New Coronavirus in Hokkaido (Japanese). Community Health Division. Hokkaido Government. http://www.pref.hokkaido.lg.jp/hf/kth/kak/hasseijoukyou.htm
- 8.Pan F., Ye T., Sun P. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 Feb 13:200370. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao D., Yao F., Wang L. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin. Infect. Dis. 2020 Mar 12 doi: 10.1093/cid/ciaa247. pii: ciaa247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei J., Xu H., Xiong J. Novel coronavirus (COVID-19) pneumonia: serial computed tomography findings. Kor. J. Radiol. 2019;21(4):501–504. doi: 10.3348/kjr.2020.0112. Epub 2020 Feb 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Russell C.D., Millar J.E., Baillie J.K. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020 Feb 15;395(10223):473–475. doi: 10.1016/S0140-6736(20)30317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lombardi A., Bozzi G., Mangioni D. Duration of quarantine in hospitalized patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a question needing an answer. Infection. 2020 Mar 6 doi: 10.1016/j.jhin.2020.03.003. pii: S0195-6701(20)30102-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lan L., Xu D., Ye G. Positive RT-PCR test results in patients recovered from COVID-19. J. Am. Med. Assoc. 2020 Feb 27 doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]