Abstract
This study analyzes the incidence of opioid-associated deaths in cancer survivors vs the general population in the US from 2006 through 2016 using National Center for Health Statistics death certificate data.
More than 40 000 people in the US died owing to opioids in 2016; the epidemic tops public health concerns. Opioids are commonly used for cancer-associated pain, and there has been a call for oncologists to become more aware of opioid-related risks and benefits.1 It is unknown, however, if opioid-related deaths in cancer survivors are rising at the same rate as in the general population.
Methods
Death certificate data were obtained from the National Center for Health Statistics (NCHS). Death certificates contain 1 underlying cause of death, up to 20 contributing causes, and demographic data. All deaths owing to opioids were included from 2006 through 2016; if present, cancer was noted as a contributing cause. Opioid-related death incidence was calculated from the US population and estimated cancer survivor population,2 both via NCHS data. To assess for differences, χ2 and R2 tests were used. Statistical significance was defined as α < .05 on a 2-sided significance level. All statistical analyses were performed with SPSS, version 21 (IBM). The Duke University Medical Center Institutional Review Board provided a waiver (Pro00045337) for this study, given that it is publicly available deidentified data. Informed consent is waived for publicly available, deidentified databases. Data were collected from May through August 2018, and analysis was completed in September 2019.
Results
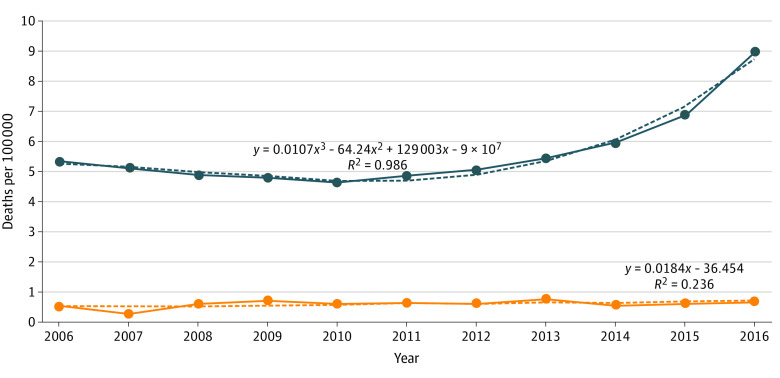
From 2006 through 2016, there were 193 500 deaths owing to opioids in the general population and 895 in the cancer population. The number of opioid-related deaths increased from 5.33 to 8.97 per 100 000 people in the general population (P < .001; R2 = 0.99) and from 0.52 to 0.66 per 100 000 (P < .001; R2 = 0.24) in the cancer population (Figure).
Figure. Opioid-Related Deaths per 100 000.
Deaths per 100 000 in the general population (blue) and in those with cancer as a contributing cause (orange). The solid lines are the data points, and the dashed lines are the best-fit lines for which the equations are listed and the R2 is calculated.
Demographic characteristics of cancer survivors with opioid-related deaths differed from those in the general population including higher education (12.7% vs 6.9% with at least a college degree), more women (38.5% vs 29.2%), fewer white individuals (82.3% vs 84.2%), more non-Hispanic individuals (94.5% vs 90.7%), and fewer single patients (24.2% vs 48.1%) (all P < .001; except race, P = .03) (Table). Cancer survivors also were older (median age, 57 years vs 42 years). The underlying primary cancer for those with opioid-related deaths was lung (22.3%), gastrointestinal (20.9%), head and neck (11.7%), and hematologic (11.3%), among others (Table).
Table. Patient Characteristics.
| Characteristic | No. (%) | P value | |
|---|---|---|---|
| Overdose deaths in the general public (n = 193 500) | Overdose deaths with cancer as contributing cause (n = 895) | ||
| Age, median (IQR) [range] | 42 (31-51) [1-103] | 57 (50-65) [13-98] | <.001 |
| Sex | |||
| Male | 136 988 (70.8) | 550 (61.5) | <.001 |
| Female | 56 512 (29.2) | 345 (38.5) | |
| Race | |||
| White | 163 014 (84.2) | 737 (82.3) | .027 |
| Black | 27 104 (14.0) | 131 (14.6) | |
| Asian | 2107 (1.1) | 18 (2.0) | |
| American Indian | 1275 (0.7) | 9 (1.0) | |
| Ethnicity | |||
| Non-Hispanic | 175 453 (90.7) | 844 (94.3) | <.001 |
| Hispanic | 16 760 (8.7) | 49 (5.5) | |
| Unknown | 1287 (0.7) | 2 (0.2) | |
| Marital status | |||
| Single | 93 020 (48.1) | 217 (24.2) | <.001 |
| Not singlea | 100 426 (51.9) | 678 (75.8) | |
| Education | |||
| At least a college education | 13 352 (6.9) | 114 (12.7) | <.001 |
| Less than a college education | 135 609 (70.1) | 625 (69.8) | |
| Unknown | 44 539 (23.0) | 156 (17.4) | |
| Underlying primary cancer | New diagnoses in USb (n = 1 735 350) | Diagnosis in opioid-related death (n = 895) | |
| Lung | 234 030 (13.5) | 200 (22.3) | NA |
| Gastrointestinal | 319 160 (18.4) | 187 (20.9) | |
| Head and neck | 64 690 (3.7) | 105 (11.7) | |
| Hematologic | 174 250 (10.0) | 101 (11.3) | |
| Prostate/urinary | 326 670 (18.8) | 90 (10.1) | |
| Breast | 268 670 (15.5) | 63 (7.0) | |
| Gynecologic | 92 070 (5.3) | 44 (4.9) | |
Abbreviations: IQR, interquartile range; NA, not applicable.
Including married, widowed, and separated.
Cancer statistics from American Cancer Society, Cancer Facts and Figures 2018.
Discussion
Death from opioids as the primary cause as documented in death certificates is 10 times less likely to occur in cancer survivors vs the general population. In the past decade, there was a slight increase in opioid-related deaths in cancer survivors; however, it was not the sharp growth seen in the general population. These findings confirm prior research showing that opioid-related hospitalizations among patients with cancer are rare but slowly increasing over time.3 This may be because of increased survivorship rates with commensurately higher rates of chronic pain or increased abuse of opioid medications.
Cancer survivors at risk for opioid overdose may be different from people in the general population, including being older with higher educational attainment; these differences may, in part, reflect the diagnosed cancer population. Additionally, some diagnoses may carry higher proportional risk; patients with head and neck cancer represent 12% of opioid-related deaths but less than 4% of new cancer diagnoses (Table).
One-third of patients experience cancer-related pain after curative treatment,4 and prescribing restrictions tied to the opioid epidemic may be reducing access for both long-term survivors and those on active treatment. One study of patients referred to palliative care found that opioid doses decreased by almost half from 2010 to 2015,5 another found that the number of patients with cancer and survivors with opioid prescriptions decreased by more than half from 2016 to 2018, with almost half told that their treatment options were limited by laws, guidelines, or insurance coverage.6
Our study is limited by its dependence on accurate documentation of cancer as a contributing cause when present. It may underestimate the number of opioid-related deaths in those on active cancer treatment if clinicians assume all deaths are owing to cancer as underlying cause; it may also underestimate survivor risk if cancer was a distant diagnosis and not noted at the time of an opioid-related death.
In summary, opioid-related deaths in the cancer population are much rarer than in the general population. Continued care should be taken when treating cancer-related pain.
References
- 1.Fisch MJ, Chang VT. Striving for safe, effective, affordable care for cancer survivors with chronic pain: another kind of moonshot. JAMA Oncol. 2016;2(7):862-864. doi: 10.1001/jamaoncol.2016.0854 [DOI] [PubMed] [Google Scholar]
- 2.de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):561-570. doi: 10.1158/1055-9965.EPI-12-1356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chua IS, Leiter RE, Brizzi KT, et al. US national trends in opioid-related hospitalizations among patients with cancer. JAMA Oncol. 2019;5(5):734-735. doi: 10.1001/jamaoncol.2019.0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18(9):1437-1449. doi: 10.1093/annonc/mdm056 [DOI] [PubMed] [Google Scholar]
- 5.Haider A, Zhukovsky DS, Meng YC, et al. Opioid prescription trends among patients with cancer referred to outpatient palliative care over a 6-year period. J Oncol Pract. 2017;13(12):e972-e981. doi: 10.1200/JOP.2017.024901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Cancer Society Cancer Action Network and Patient Quality of Life Coalition Summary of Opioid Access Research Project. Accessed September 5, 2018. https://www.fightcancer.org/sites/default/files/ACS%20CAN%20PQLC%20Opioid%20Research%20Project%20Key%20Findings%20Summary%20Memo%20FINAL.pdf