This cohort study analyzes the association between postsurgical hyposmia and/or anosmia and a variety of patient, disease, and treatment factors among patients with primary sellar lesions.
Key Points
Question
What are demographic, comorbidity, cephalometric, intraoperative, histological, and postoperative risk factors for patient-reported olfactory dysfunction after endoscopic transsphenoidal hypophysectomy?
Findings
In this cohort study of 147 patients with primary sellar lesions who underwent endoscopic transsphenoidal hypophysectomy, smoking history, acute angle between the planum sphenoidale and face of the sella turcica on sagittal imaging, and abdominal fat grafting were associated with patient-reported olfactory dysfunction. Increased number of months after the surgical procedure was associated with patient-reported normosmia.
Meaning
These findings suggest that smoking cessation counseling, cephalometric measurements of preoperative imaging, and judicious use of abdominal fat grafting may improve patient-reported olfactory outcomes after a transsphenoidal surgical procedure.
Abstract
Importance
Iatrogenic olfactory dysfunction after endoscopic transsphenoidal hypophysectomy (ETSH) is an overlooked complication without elucidated risk factors.
Objective
To assess the independent prognostic role of demographic, comorbidity, cephalometric, intraoperative, histological, and postoperative parameters in patient-reported postoperative olfactory dysfunction, and to explore the association between anatomical measurements of the skull base and sinonasal cavity and postoperative olfactory dysfunction.
Design, Setting, and Participants
This retrospective cohort study in a tertiary care medical center enrolled consecutive patients with primary sellar lesions who underwent ETSH between January 1, 2015, and January 31, 2019. Patients were excluded if they underwent multiple sinonasal surgical procedures, presented with a sellar malignant neoplasm, required an expanded transsphenoidal approach, had nasal polyposis or a neurodegenerative disease, or sustained traumatic brain injury. After undergoing medical record review and telephone screening, patients were asked to participate in a 3-item telephone survey.
Main Outcomes and Measures
The primary outcome was the Clinical Global Impressions change in smell rating, a validated transitional patient-reported outcome measure. Patients rated their change in smell before and after ETSH on a 7-point Likert scale, with the following response options: (1) much better, (2) somewhat better, (3) slightly better, (4) neither better nor worse, (5) slightly worse, (6) somewhat worse, or (7) much worse. Responses of slightly worse, somewhat worse, and much worse were surrogates for postoperative olfactory dysfunction status. Patient medical records, preoperative imaging scans, operative notes, and pathology reports were reviewed.
Results
Of the 147 patients (mean [SD] age, 54 [15] years; 79 women [54%]) who responded to the telephone survey, 42 (29%) reported olfactory dysfunction after ETSH. Median (interquartile range [IQR]) time between the ETSH completion and survey response was 31.1 (21-43) months. On multivariable analysis, abdominal fat grafting (adjusted relative risk [aRR], 2.95; 95% CI, 1.89-4.60) was associated with postoperative olfactory dysfunction, whereas smoking history (aRR, 1.54; 95% CI, 0.95-2.51) demonstrated a clinically meaningful but imprecise effect size. A more obtuse angle between the planum sphenoidale and face of the sella turcica on sagittal imaging was protective (aRR, 0.98; 95% CI, 0.96-0.99). Increased number of months after the ETSH was associated with patient-reported normosmia (aRR, 0.93; 95% CI, 0.91-0.95). In contrast, other comorbidities; intraoperative variables such as turbinate resection, nasoseptal flap, and mucosal or bone grafting; histological variables such as pathology and proliferative index; and postoperative variables such as adjuvant radiotherapy were not associated with postoperative olfactory dysfunction.
Conclusions and Relevance
This study found that abdominal fat grafting, acute skull base angle, and smoking history appeared to be clinically significant risk factors for patient-reported postoperative olfactory dysfunction. Increased time after ETSH may be associated with better olfactory outcomes.
Introduction
Sellar lesions account for 17% of all central nervous system neoplasms.1 About 85% of the pathology is pituitary adenoma, and the other 15% includes Rathke cleft cysts, craniopharyngioma, meningioma, chordoma, distant metastases, and lymphoma.2,3 Historically, the sella turcica was approached transcranially, which required large incisions, craniectomies, bone flaps, and physical retraction of brain tissue to adequately expose the sella.4 The current standard-of-care treatment has evolved to an endoscopic transsphenoidal approach to limit patient morbidity and mortality.
Although the endoscopic endonasal approach is less invasive, olfactory dysfunction is a known complication that may be attributed to the direct disruption of olfactory neuroepithelium by the anterior skull base, superior nasal septum, and portions of the superior and middle turbinate; obstruction from packing; and/or inflammation.5,6 According to the literature, 18% to 38% of patients reported a decreased subjective sense of smell at 3 months after undergoing endoscopic transsphenoidal hypophysectomy (ETSH); about 10% of the hyposmia was moderate or severe.7,8,9 Meanwhile, objective psychophysical testing revealed a similar 8% to 35% incidence of postoperative moderate-to-severe hyposmia, a wide range that underscored the inconsistency of the methods used and results reported in previous studies.10,11,12 A recent meta-analysis of studies that used only validated objective measures of olfaction revealed no differences in olfaction before and after the procedure but also highlighted the high heterogeneity of the included studies.13
Despite the nontrivial rate of postoperative olfactory deficits, both self-reported and measured by psychophysical testing, postoperative olfactory dysfunction may still be an overlooked complication. In large epidemiological studies, olfactory impairment was shown to have implications for the quality of life of affected individuals, such as decreased appetite, poor hygiene, frequent exposure to environmental hazards, and higher rates of mood disturbances.14,15,16,17,18 Olfactory dysfunction was also found to be associated with increased mortality in older adults independent of nutritional status, cognitive function, mental health, smoking status, alcohol abuse, and frailty.19 Beyond the numbers were anecdotal reports of individuals living with an invisible disability as if they were “living a life in a plastic bag.”16(p16)
Many risk factors for olfactory dysfunction exist in the general population. Demographic and comorbidity risk factors include older age, male sex, non-white race/ethnicity, smoking history, alcohol abuse, diabetes, asthma, and septal deviation.20,21,22,23,24 Risk factors specific to postoperative olfactory dysfunction include intraoperative variables, such as nasoseptal flap (NSF) harvest, and histological variables, such as nonpituitary pathologies.8,11,12,25 However, no study has explored the association between postoperative olfactory dysfunction and a comprehensive list of demographic, comorbidity, cephalometric, intraoperative, histological, and postoperative features. Thus, the goal of this study was to evaluate the independent prognostic role of all of these parameters in patient-reported postoperative olfactory dysfunction and to explore the association between postoperative olfactory dysfunction and various anatomical measurements of the anterior skull base and sinonasal cavity.
Methods
We conducted a single-center retrospective cohort study of consecutive patients with primary sellar lesions who underwent ETSH between January 1, 2015, and January 31, 2019. This study received institutional review board approval from Washington University School of Medicine in St Louis before medical record review and data collection commenced. All participants provided verbal informed consent on the telephone.
All patients at the tertiary care medical center who underwent ETSH during this time frame were identified using Current Procedural Terminology codes. Exclusion criteria included patients who (1) underwent a sinonasal or an anterior skull base surgical procedure, (2) presented with a sellar malignant neoplasm, (3) required an expanded transsphenoidal approach involving resection of the planum sphenoidale, (4) had nasal polyposis, (5) had a neurodegenerative disease, or (6) previously sustained traumatic brain injury that required hospitalization.
All eligible patients, after undergoing medical record review and telephone screening, were asked to participate in a 3-item telephone survey. The first question was formatted according to the Clinical Global Impressions severity scale, a validated static patient-reported outcome measure26: Overall, please rate your sense of smell now. Response options included (1) excellent, (2) very good, (3) good, (4) fair, (5) poor, or (6) absent. The second question was formatted according to the Clinical Global Impressions change scale, a validated transitional patient-reported outcome measure26: Compared to your sense of smell before surgery, how would you rate your smell now? Response options were (1) much better, (2) somewhat better, (3) slightly better, (4) neither better nor worse, (5) slightly worse, (6) somewhat worse, or (7) much worse. The third question asked, If you experienced a change in smell since surgery, are there any other events that you believe may have changed your sense of smell? If so, please list.
The primary outcome was the Clinical Global Impressions change in smell rating. Patients were asked to rate their change in sense of smell before and after ETSH on a 7-point Likert scale. Responses of slightly worse, somewhat worse, and much worse were surrogates for postoperative olfactory dysfunction status. Demographic and comorbidity data in the medical record, including age, sex, race/ethnicity, smoking status, current alcohol abuse, chronic rhinosinusitis, septal deviation, diabetes, hypothyroidism, asthma, obstructive sleep apnea, supplemental oxygen use (including positive airway pressure), stroke, and family history of neurodegenerative disease, were reviewed. Overall severity of comorbidities was calculated using the Adult Comorbidity Evaluation-27 instrument (score range: 0-3, with the highest score indicating severe comorbidity burden).27
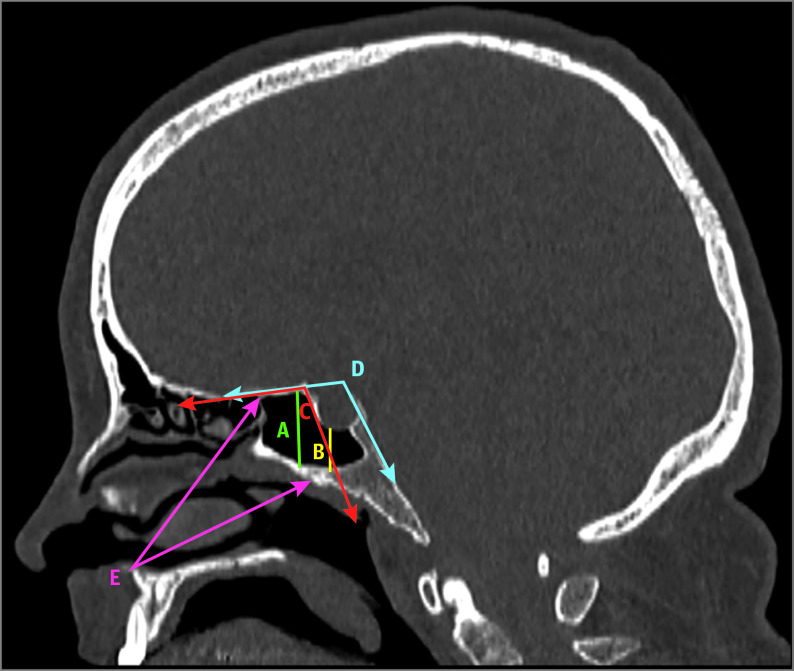
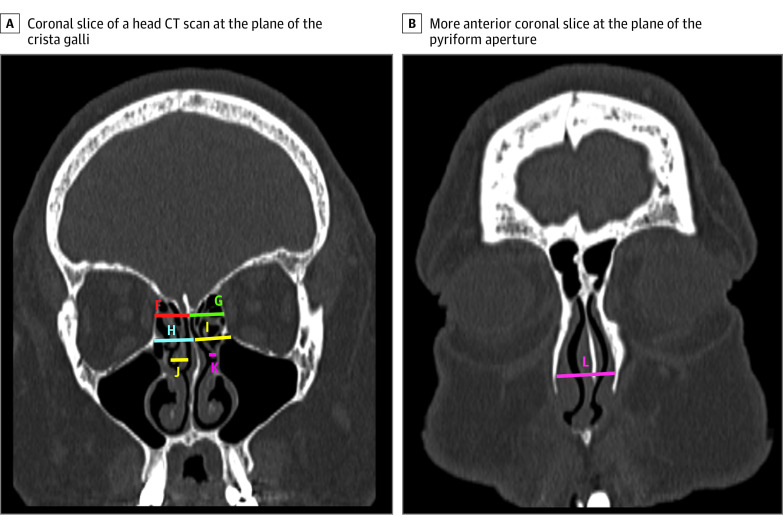
Cephalometric measurements of preoperative computed tomography (CT) and magnetic resonance imaging (MRI) scans were also performed. All patients underwent 1-mm thin-cut CT and MRI for preoperative planning and intraoperative navigation. Maximal tumor diameter was measured from the MRI. Using sagittal CT bone windows centered on the midline of the sella turcica, we measured the vertical distances between the floor of the sphenoid sinus and planum sphenoidale as well as between the floor of the sphenoid sinus and base of the sella turcica (Figure 1). Using the same sagittal slice, we measured different angles of the skull base and the cephalocaudal transsphenoidal working angle. In a coronal plane through the crista galli, different widths of the nasal cavity, middle turbinate widths, and olfactory fossa depth were measured bilaterally (Figure 2A). On a more anterior coronal slice, the maximum width of the pyriform aperture was measured (Figure 2B).
Figure 1. Sagittal Slice of a Head Computed Tomography Scan Centered at the Midline of the Sella Turcica of a Study Patient.
A indicates vertical distance between the sphenoid sinus floor and planum sphenoidale; B, vertical distance between the sphenoid sinus floor and base of the sella turcica; C, angle between the line along the planum sphenoidale and line along the anterior face of the sella turcica; D, angle between the line along the planum sphenoidale and line along the clivus; and E, angle between the line from the anterior nasal spine to the most superior aspect of the anterior wall of the sphenoid sinus and line from the anterior nasal spine to the anteroinferior portion of the sphenoid sinus face.
Figure 2. Coronal Slices of a Head Computed Tomography (CT) Scan for Nasal Cavity Width Measurements .
F indicates horizontal distance between the superior limit of the right lamina papyracea and midline cribriform plate; G, horizontal distance between the superior limit of the left lamina papyracea and midline cribriform plate; H, horizontal distance between the right orbital strut and nasal septum; I, horizontal distance between the left orbital strut and nasal septum; J, width of the right middle turbinate; K, width of the left middle turbinate; and L, maximum width of the pyriform aperture. Not shown are the right and left olfactory fossa depth measurements.
One of us (J.J.L.) performed cephalometric measurements on all patients while blinded to olfactory outcomes. Our board-certified neuroradiologist (H.L.P.O.) concurrently performed cephalometric measurements on a randomly selected sample of 30 patients. Interrater reliability of the measurements of these 30 patients was calculated with intraclass correlation coefficient (ICC) using a 2-way mixed-effects model for absolute agreement. The ICC was greater than 0.75 for all measures (median [range], 0.81 [0.76-0.98]), except for the pyriform aperture width (ICC, 0.65), indicating good-to-excellent reliability.28 All cephalometric measurements reported were generated by one of us (J.J.L.).
Intraoperative data, which were assessed from the operative notes, included middle and superior turbinate resection (including partial), anterior septoplasty to correct septal deviation, use of an ultrasonic aspirator (Sonopet; Stryker), free mucosal or bone grafting, NSF harvest, abdominal fat grafting, and cerebrospinal fluid leak. Histological variables from the pathology reports were also collected, which included pathological diagnosis, tumor functioning status based on immunostaining, mitotic index, Ki-67 index, presence of Crooke hyaline changes, and apoplexy or necrosis. An elevated proliferative index was classified as Ki-67 index greater than 3.0%.
In addition, postoperative events, including diabetes insipidus (DI), adrenal insufficiency, acute sinusitis requiring antibiotics, and adjuvant radiation therapy, were recorded. Adrenal insufficiency and DI were considered persistent if the patient still required medical management at the time of the telephone survey. Adjuvant radiation therapy included Gamma Knife, fractionated radiotherapy, and proton beam therapy. The number of months between the ETSH and the telephone survey was also calculated.
Statistical Analysis
Descriptive statistics were used to explore the distribution of all characteristics of the study cohort. Univariate logistic binomial regression with robust SEs was used to calculate the relative risk (RR) and 95% CI of postoperative olfactory dysfunction as a function of each variable. A forward stepwise multivariable regression model with α = .10 for variable entry was used to avoid overfitting the model. Adjusted RR (aRR) and 95% CIs were then reported. Statistical calculations were performed with SPSS, version 25 (IBM Corp), and Stata, version 15 (StataCorp LLC).
Results
In total, 202 patients with primary sellar lesions who underwent ETSH were eligible. Of these patients, 147 (mean [SD] age, 54 [15] years; 79 women [54%]) responded to the survey. The rate of patient-reported postoperative olfactory dysfunction was 29% (42 of 147 patients). Median (interquartile range [IQR]) time between the ETSH completion and survey response was 31 (21-43) months. Median global rating of sense of smell at the time of the survey was 3.0 or good (IQR, 2.0 or fair to 4.0 or very good). Baseline characteristics and results from univariate logistic binomial regression separated by postoperative olfactory dysfunction and normosmia are presented in Table 1. Univariate analysis revealed that smoking history (RR, 2.17; 95% CI, 1.27-3.69), asthma (RR, 1.69; 95% CI, 0.93-3.05), NSF harvest (RR, 1.76; 95% CI, 1.06-2.90), abdominal fat grafting (RR, 2.35; 95% CI, 1.28-4.30), and time since ETSH in months (RR, 0.93; 95% CI, 0.91-0.95) demonstrated large and precise point estimates for RR of developing postoperative olfactory dysfunction.
Table 1. Association Between Postoperative Olfactory Dysfunction and Baseline Characteristics of the Study Population.
| Variable | Normosmia (n = 105) | Postoperative olfactory dysfunction (n = 42) | RR (95% CI)a |
|---|---|---|---|
| Age, median (range), y | 56 (21-85) | 55 (19-82) | 0.99 (0.98-1.01) |
| Sex | |||
| Men | 48 (46) | 20 (48) | 1 [Reference] |
| Women | 57 (54) | 22 (52) | 0.95 (0.57-1.58) |
| Race/ethnicity | |||
| White | 83 (79) | 32 (76) | 1 [Reference] |
| Black | 19 (18) | 9 (21) | 1.16 (0.62-2.14) |
| Other | 3 (3) | 1 (3) | 0.90 (0.16-5.06) |
| Smoking history | 37 (35) | 26 (62) | 2.17 (1.27-3.69) |
| CRSsNP | 7 (7) | 3 (7) | 1.05 (0.39-2.83) |
| Deviated septum | 48 (46) | 19 (45) | 0.99 (0.59-1.65) |
| Diabetes | 30 (29) | 9 (21) | 0.76 (0.40-1.43) |
| Hypothyroidism | 58 (55) | 25 (60) | 1.13 (0.67-1.92) |
| Asthma | 10 (10) | 8 (19) | 1.69 (0.93-3.05) |
| OSA | 24 (23) | 9 (21) | 0.94 (0.50-1.77) |
| Supplemental oxygen | 16 (15) | 5 (12) | 0.81 (0.36-1.83) |
| Family history of dementia | 8 (8) | 3 (7) | 0.95 (0.35-2.60) |
| ACE-27 score | |||
| None/mild | 63 (60) | 28 (67) | 1 [Reference] |
| Moderate/severe | 42 (40) | 14 (33) | 0.81 (0.47-1.41) |
| Intraoperative variables | |||
| Right MT resection | 98 (93) | 39 (93) | 0.95 (0.35-2.55) |
| Right ST resection | 83 (79) | 34 (81) | 1.08 (0.56-2.11) |
| Left MT resection | 66 (63) | 26 (62) | 0.97 (0.57-1.65) |
| Left ST resection | 62 (59) | 23 (55) | 0.88 (0.53-1.48) |
| 4-turbinate resection | 58 (55) | 22 (52) | 0.92 (0.55-1.54) |
| Anterior septoplasty | 18 (17) | 8 (19) | 1.10 (0.57-2.09) |
| Sonopet | 66 (63) | 24 (57) | 0.84 (0.50-1.41) |
| Free mucosal/bone graft | 21 (20) | 9 (21) | 1.06 (0.57-1.98) |
| NSF harvest | 26 (25) | 18 (43) | 1.76 (1.06-2.90) |
| Abdominal fat graft | 3 (3) | 5 (12) | 2.35 (1.28-4.30) |
| CSF leak | 34 (32) | 16 (38) | 1.19 (0.71-2.01) |
| Histologic variables | |||
| Pathological diagnosis | |||
| Pituitary adenoma | 97 (92) | 36 (86) | 1 [Reference] |
| Otherb | 8 (8) | 6 (14) | 1.58 (0.81-3.09) |
| Functioning tumor | 63 (60) | 20 (48) | 0.70 (0.42-1.17) |
| Ki-67, median (range), % | 2.0 (0.0-13.4) | 1.8 (0.0-20.0) | 1.00 (0.89-1.13) |
| Elevated proliferative index | 24 (23) | 7 (17) | 0.71 (0.35-1.45) |
| Crooke hyaline change | 7 (7) | 1 (2) | 0.42 (0.07-2.72) |
| Apoplexy | 6 (6) | 3 (7) | 1.18 (0.45-3.09) |
| Postoperative variables | |||
| Time since ETSH, mo | 36.9 (13.9-54.1) | 22.3 (5.0-36.5) | 0.93 (0.91-0.95) |
| Persistent DI | 8 (8) | 6 (14) | 1.58 (0.81-3.09) |
| Persistent AI | 23 (22) | 13 (31) | 1.38 (0.81-2.37) |
| Acute sinusitis | 14 (13) | 8 (19) | 1.34 (0.72-2.50) |
| Adjuvant XRT | 15 (14) | 1 (2) | 0.20 (0.03-1.36) |
Abbreviations: ACE-27, Adult Comorbidity Evaluation 27-item instrument (score range: 0-3, with the highest score indicating severe comorbidity burden); AI, adrenal insufficiency; CRSsNP, chronic rhinosinusitis without nasal polyposis; CSF, cerebrospinal fluid; DI, diabetes insipidus; ETSH, endoscopic transsphenoidal hypophysectomy; MT, middle turbinate; NSF, nasoseptal flap; OSA, obstructive sleep apnea; RR, relative risk; ST, superior turbinate; XRT, radiation therapy.
RR with 95% CI calculated using univariate robust logistic binomial regression.
Includes Rathke cleft cyst (n = 11), craniopharyngioma (n = 2), and meningioma (n = 1).
The definitions and distribution of the 15 cephalometric measurements between the normosmia and postoperative olfactory dysfunction (hyposmic or anosmic) groups are presented in Table 2. The only measure with a large and precise point estimate of effect size was skull base angle No. 1 (RR, 0.98; 95% CI, 0.96-1.00), defined as the angle between the line along the planum sphenoidale and line along the anterior face of the sella turcica on sagittal imaging. Median (IQR) skull base angle No. 1 was 93.5° (81.4°-93.5°). The ICC for skull base angle No. 1 measurements between 2 of us (J.J.L., H.L.P.O.) was 0.87 (95% CI, 0.73-0.94), indicating good-to-excellent interrater reliability. Other measures of skull base height, angle, and nasal cavity width had small and/or imprecise effect sizes.
Table 2. Association Between Preoperative Cephalometric Characteristics and Postoperative Olfactory Dysfunction.
| Variable | Definition | Median (range) | RR (95% CI)a | |
|---|---|---|---|---|
| Normosmia (n = 105) | Postoperative olfactory dysfunction (n = 42) | |||
| Maximal tumor diameter, cm | NA | 2.24 (0.25-4.72) | 2.37 (0.24-4.72) | 1.02 (0.76-1.38) |
| Skull base height No.1, cm | Vertical distance between the sphenoid sinus floor and planum sphenoidale | 2.21 (0.00-3.55) | 2.21 (0.00-3.01) | 0.82 (0.48-1.38) |
| Skull base height No.2, cm | Vertical distance between the sphenoid sinus floor and base of the sella turcica | 0.96 (0.00-2.10) | 1.00 (0.00-1.85) | 0.96 (0.62-1.48) |
| Skull base angle No.1, ° | Angle between the line along the planum sphenoidale and line along the anterior face of the sella turcica | 96.44 (64.91-130.64) | 85.76 (60.34-126.02) | 0.98 (0.96-1.00) |
| Skull base angle No.2, ° | Angle between the line along the planum sphenoidale and line along the clivus | 106.97 (85.36-130.89) | 106.79 (92.26-142.16) | 1.00 (0.97-1.03) |
| Working angle, ° | Angle between the line from the anterior nasal spine to the most superior aspect of the anterior wall of the sphenoid sinus and line from the anterior nasal spine to anteroinferior portion of sphenoid sinus face | 24.45 (14.75-33.73) | 25.42 (16.98-33.31) | 1.02 (0.96-1.09) |
| Right superior nasal cavity width, cm | Horizontal distance between the right lamina papyracea and midline of the cribriform plate | 1.16 (0.78-1.74) | 1.17 (0.89-1.71) | 1.29 (0.36-4.65) |
| Right middle nasal cavity width, cm | Horizontal distance between the right orbital strut and nasal septum | 1.32 (0.76-1.99) | 1.36 (0.92-1.89) | 1.69 (0.56-5.11) |
| Right middle turbinate width, cm | NA | 0.67 (0.27-1.45) | 0.70 (0.40-1.10) | 1.08 (0.33-3.56) |
| Left superior nasal cavity width, cm | Horizontal distance between the left lamina papyracea and midline of the cribriform plate | 1.19 (0.82-2.01) | 1.22 (0.84-1.62) | 0.99 (0.26-3.71) |
| Left middle nasal cavity width, cm | Horizontal distance between the left orbital strut and nasal septum | 1.37 (0.95-2.20) | 1.39 (1.01-2.00) | 1.44 (0.50-4.12) |
| Left middle turbinate width, cm | NA | 0.67 (0.24-1.28) | 0.63 (0.22-1.20) | 0.58 (0.12-2.83) |
| Right olfactory fossa depth, cm | NA | 0.61 (0.21-1.11) | 0.55 (0.25-1.16) | 0.40 (0.08-1.98) |
| Left olfactory fossa depth, cm | NA | 0.61 (0.18-1.13) | 0.57 (0.20-1.10) | 0.47 (0.13-1.77) |
| Pyriform aperture width, cm | NA | 2.41 (1.86-2.94) | 2.36 (2.10-2.81) | 0.64 (0.24-1.71) |
Abbreviations: NA, not applicable; RR, relative risk.
RR with 95% CI calculated using univariate robust logistic binomial regression.
In the multivariable model, abdominal fat grafting (aRR, 2.95; 95% CI, 1.89-4.60) was associated with postoperative olfactory dysfunction and demonstrated the largest point estimate of effect size (Table 3). Increased skull base angle No. 1 (aRR, 0.98; 95% CI, 0.96-0.99) and number of months since ETSH (aRR, 0.93; 95% CI, 0.91-0.95) were associated with postoperative patient-reported normosmia. That is, when controlling for the other variables in the model, each additional degree to skull base angle No. 1 decreased the risk of postoperative olfactory dysfunction by 2% so that an increased angle was protective; a 10° increase in skull base angle No. 1 decreased the risk of postoperative olfactory dysfunction by 21% as demonstrated by its large point estimate of effect size (aRR, 0.79; 95% CI, 0.68-0.92). Each additional month since ETSH decreased the risk of olfactory dysfunction at that time by 7%, whereas each additional year since ETSH decreased the risk by 58% (aRR, 0.42; 95% CI, 0.32-0.54). In addition, smoking history likely had a clinically meaningful association with developing postoperative olfactory dysfunction as it demonstrated a large point estimate of effect size (aRR, 1.54; 95% CI, 0.95-2.51).
Table 3. Multivariable Analysis of Comorbidity, Cephalometric, Intraoperative, and Postoperative Variables and Olfactory Dysfunction.
| Variable | aRR (95% CI) |
|---|---|
| Smoking history | 1.54 (0.95-2.51) |
| Skull base angle No. 1 | 0.98 (0.96-0.99) |
| Abdominal fat grafting | 2.95 (1.89-4.60) |
| Time since ETSH, mo | 0.93 (0.91-0.95) |
Abbreviations: aRR, adjusted relative risk; ETSH, endoscopic transsphenoidal hypophysectomy.
A sensitivity analysis also excluded patients who responded to the third question by reporting other events since ETSH that may have contributed to smell loss. Seven of the 42 patients (17%) who reported olfactory dysfunction listed other events, including 4 with postoperative uncomplicated acute sinusitis that resolved with oral antibiotics and saline irrigations, 2 with persistent nasal crusting and drainage, and 1 with an infected implant (MEDPOR TSI; Stryker) that required surgical removal. Univariate and multivariable results were similar to the results of the entire cohort as fat grafting (aRR, 3.49; 95% CI, 1.99-6.13), skull base angle No. 1 (aRR, 0.98; 95% CI, 0.96-0.99), and number of months since ETSH (aRR, 0.93; 95% CI, 0.91-0.95) still demonstrated large point estimates of effect size. Although not as strong of a risk factor, smoking history still demonstrated a rather large association (aRR, 1.45; 95% CI, 0.84-2.52).
Another sensitivity analysis of risk factors for severe postoperative olfactory dysfunction, defined as patient-reported much worse sense of smell, was performed. Of the 42 patients with postoperative olfactory dysfunction, 15 (36%) reported much worse sense of smell, 13 (31%) reported somewhat worse sense of smell, and 14 (33%) reported slightly worse sense of smell. Variables with large point estimates of RR for severe postoperative olfactory dysfunction on univariate analysis included smoking history (RR, 2.00; 95% CI, 0.75-5.35), asthma (RR, 3.58; 95% CI, 1.38-9.33), NSF (RR, 2.05; 95% CI, 0.79-5.32), and persistent DI (RR, 2.38; 95% CI, 0.76-7.45). Abdominal fat grafting (RR, 1.24; 95% CI, 0.18-8.35), skull base angle No. 1 (RR, 0.99; 95% CI, 0.96-1.03), and time since ETSH (RR, 0.97; 95% CI, 0.94-1.01) were not associated with severe postoperative olfactory dysfunction.
Discussion
The aim of this cohort study was to comprehensively assess and identify multiple demographic, comorbidity, cephalometric, intraoperative, histological, and postoperative risk factors for iatrogenic olfactory dysfunction. Univariate analysis of demographic and comorbidity variables revealed that history of smoking and asthma were clinically meaningful risk factors for postoperative olfactory dysfunction. Notable comorbidities previously associated with general olfactory dysfunction that were not found to be associated with postoperative olfactory dysfunction in this sample include chronic rhinosinusitis, septal deviation, diabetes, and hypothyroidism.20,22,23,24 Univariate analysis of intraoperative variables illustrated that NSF harvest and abdominal fat grafting for reconstruction were also risk factors for postoperative olfactory dysfunction. Among the remaining variables, both nonpituitary adenoma pathology and persistent DI demonstrated an RR higher than 1.5, but the point estimate was imprecise as demonstrated by the wide 95% CI; thus, definitive conclusions cannot be made.
Using preoperative CT and/or MRI, we also identified cephalometric measurements associated with postoperative olfactory dysfunction risk. Fifteen discrete measurements of tumor size, skull base height, skull base angle, and nasal cavity width were taken for each patient. An increased angle between the planum sphenoidale and anterior face of the sella turcica on sagittal imaging was protective. A more obtuse angle may be seen with anterior skull bases that are sloped more superiorly from the planum sphenoidale to cribriform plate. Presumably, this increased slope would position the olfactory bulb superiorly and farther away from the operative field during ETSH, thereby decreasing the risk of trauma to the olfactory neuroepithelia. Although the effect size for a 1° increase was relatively small and close to 1.0, the effect size for a 10° increase was much larger and clinically meaningful (aRR, 0.79; 95% CI, 0.68-0.92). Given the wide range of skull base angle No. 1 measurements (range, 60.3°-130.6°), differences of 10° or greater were numerous in this cohort and likely represented common anatomical variability. This protective property was not seen for skull base angle No. 2, defined as the angle between the planum and clivus, possibly because of the more variable angle of the clivus.
On univariate analysis, the increased number of months since ETSH was associated with patient-reported normosmia. That is, patients who were further removed from their surgical procedure date were more likely to report unchanged olfactory function from preoperative levels. Previous studies have reported transient postoperative olfactory dysfunction that spontaneously improved over time in this population, which may be present in this sample.10,29 However, patients in earlier studies appeared to recover olfactory function within 6 months. In the present sample, all patients were evaluated at least 5 months after ETSH, and only 1% of patients (2 of 147) were surveyed within 12 months. Long-term olfactory recovery that extends beyond 12 months may exist, but over time, patients with postoperative olfactory dysfunction are more likely to gradually adjust to their disability until they reach the point at which they either no longer notice their olfactory limitations or no longer remember their sense of smell before undergoing ETSH.
Risk factors for severe postoperative olfactory dysfunction were also explored. Although smoking history, asthma, NSF harvest, and persistent DI had large point estimates of effect size, the precision was low, as evident by the wide 95% CI owing to a small case size (n = 15). Fat grafting, skull base angle No. 1, and time since ETSH were not associated with severe postoperative olfactory dysfunction. Multivariable analysis could not be performed because of the risk of overfitting the model, and definitive conclusions of severe postoperative olfactory dysfunction risk factors cannot be made without a larger subsample size.
In multivariable analysis, abdominal fat grafting demonstrated almost a 3-fold increased risk of postoperative olfactory dysfunction after other variables in the model were adjusted. The need for a fat graft may be a surrogate marker for large intracranial defect size after resection. However, fat grafting still demonstrated a large effect size when controlling for maximal tumor diameter. An alternative explanation is that fat may undergo liquefaction and produce an oily transudate that remains in the skull base area, thereby promoting inflammation that damages nearby olfactory nerve fibers.30 Fat grafting was not associated with severe postoperative olfactory dysfunction, suggesting that fat graft may instead be associated with milder degrees of smell loss. Smoking history demonstrated a 50% higher risk of postoperative olfactory impairment, which was likely clinically meaningful but not definitive because of the imprecision of the point estimate of RR. Greater skull base angle No. 1 and increased number of months after ETSH were still protective. After controlling for smoking history, abdominal fat grafting, skull base angle No. 1, and time since ETSH, we found that asthma and NSF harvest were no longer associated with postoperative olfactory dysfunction.
Subjective olfactory dysfunction after ETSH was reported in the literature in 18% to 38% of patients,7,8,9 a rate that is consistent with this study’s rate of 29%. Risk factors specific to postoperative olfactory dysfunction identified in previous studies included NSF harvest,12,25 nonpituitary adenoma diagnosis,8 and bigger tumor size,31 but even those traits were debated or unconfirmed.32,33 For instance, in this sample, NSF harvest appeared to be strongly associated with postoperative olfactory dysfunction on univariate analysis, but after the multivariable model was used to control for confounders, the strong association was diminished. To our knowledge, additional demographic, comorbidity, intraoperative, and postoperative risk factors have not been described, and no group has yet defined cephalometric measurements according to routine preoperative imaging and their association with postoperative olfactory dysfunction.
We believe it is important to emphasize the use of validated patient-reported outcome measures for olfaction. Although this study did not use psychophysical olfactory testing, such as the UPSIT (University of Pennsylvania Smell Identification Test; Sensonics International) or Sniffin’ Sticks (Burghart), it assessed olfactory impairment using a patient-reported change in olfaction symptom measure modified from a widely used and validated generic measure of change.26 Capturing patient-reported smell change was clinically meaningful and was of utmost importance to the patient. Psychophysical testing is presumed to generate objective olfaction data, but these tests are not purely objective and reflect the patient’s subjective interpretation of each odor. Meaningful patient-reported data can provide valuable information.34
Findings from this study, although they still require validation in large prospective studies, may already have clinical utility. They underscore the importance of preoperative counseling to smoking cessation. A history of smoking likely leads to inflammatory changes to the respiratory sinonasal mucosa, which may predispose these patients to more severe decrements in olfaction after additional insults, such as iatrogenic trauma. Because it is difficult to discern baseline sinonasal inflammation in patients without clinical or radiographic signs of chronic rhinosinusitis, this preoperative inflammatory state may be subclinical.
In addition, this study has shown that performing various measurements of skull base positioning and nasal cavity width is feasible, reliable, and replicable in a large number of patients. If validated, skull base angle can be measured and used to risk-stratify patients for more personalized counseling. In patients with a history of smoking and with acutely angled skull bases who have no intraoperative cerebrospinal fluid leak or a low-to-medium flow leak, surgeons may want to consider alternative reconstructive techniques to fat grafting, such as autologous substitutes like free mucosal or bone graft or nonautologous material.
For validation, these findings require a large prospective cohort study that would measure both patient-reported and psychophysical olfactory outcomes before and after ETSH. Other future directions may include a prospective descriptive study on long-term olfaction results beyond 12 months in patients who report postoperative olfactory dysfunction, a prospective cohort study on the association between NSF size and postoperative olfactory dysfunction, and a pilot randomized clinical trial of olfactory outcomes after a corticosteroid or placebo pretreatment in patients who underwent ETSH to better delineate the implication of preoperative inflammation for postoperative olfaction.
Strengths and Limitations
This study has strengths that separate it from other studies. These strengths include a wide-ranging assessment of demographic, comorbidity, intraoperative, histological, and postoperative variables; proof of concept of novel cephalometric measurements of the skull base and nasal cavity anatomy; and identification of decreased skull base angle as a risk factor of postoperative olfactory dysfunction.
This study has several limitations. First, as with any retrospective study, we relied on clinician notes, operative summaries, and pathology reports when assessing the risk factors, which may be incomplete or biased. Second, the retrospective design of the study precluded formal preoperative olfactory testing and postoperative testing at prespecified intervals. Third, recall bias may have been introduced given that patients were surveyed a median (IQR) of 31 (21-43) months after ETSH, and there may have been confounding events, such as viral upper respiratory infections, inflammatory conditions, or trauma, that have since resulted in olfactory changes. We attempted to gather and control for any confounding events with the third question of the survey, which asked patients about any other events that may have changed their sense of smell. Fourth, there was a potential referral bias where more complex ETSH procedures were overrepresented at the tertiary care institution. We also attempted to control for this limitation by including only those patients with sellar lesions. Fifth, there may be volunteer bias where survey respondents may be different from the 55 eligible patients (27%) who did not respond to the survey.
Conclusions
This study’s findings suggest that iatrogenic olfactory dysfunction after ETSH may have a profound and permanent role in patients’ quality of life. Increased number of months after surgery was associated with better olfactory outcomes. Abdominal fat grafting and smoking history were clinically significant risk factors for patient-reported postoperative olfactory dysfunction, whereas a more obtuse angle between the planum sphenoidale and face of the sella turcica measured on sagittal imaging appeared to be protective. Measurement of skull base positioning on preoperative imaging may enable further stratification of postoperative olfactory dysfunction risk in all patients.
References
- 1.Ostrom QT, Gittleman H, Liao P, et al. CBTRUS Statistical Report: Primary brain and other central nervous system tumors diagnosed in the United States in 2010-2014. Neuro Oncol. 2017;19(suppl_5):v1-v88. doi: 10.1093/neuonc/nox158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Dahmani K, Mohammad S, Imran F, et al. Sellar masses: an epidemiological study. Can J Neurol Sci. 2016;43(2):291-297. doi: 10.1017/cjn.2015.301 [DOI] [PubMed] [Google Scholar]
- 3.Saeger W, Lüdecke DK, Buchfelder M, Fahlbusch R, Quabbe HJ, Petersenn S. Pathohistological classification of pituitary tumors: 10 years of experience with the German Pituitary Tumor Registry. Eur J Endocrinol. 2007;156(2):203-216. doi: 10.1530/eje.1.02326 [DOI] [PubMed] [Google Scholar]
- 4.Liu JK, Das K, Weiss MH, Laws ER Jr, Couldwell WT. The history and evolution of transsphenoidal surgery. J Neurosurg. 2001;95(6):1083-1096. doi: 10.3171/jns.2001.95.6.1083 [DOI] [PubMed] [Google Scholar]
- 5.Patel ZM, DelGaudio JM. Olfaction following endoscopic skull base surgery. Curr Opin Otolaryngol Head Neck Surg. 2016;24(1):70-74. doi: 10.1097/MOO.0000000000000216 [DOI] [PubMed] [Google Scholar]
- 6.Thompson CF, Kern RC, Conley DB. Olfaction in endoscopic sinus and skull base surgery. Otolaryngol Clin North Am. 2015;48(5):795-804. doi: 10.1016/j.otc.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 7.Dusick JR, Esposito F, Mattozo CA, Chaloner C, McArthur DL, Kelly DF. Endonasal transsphenoidal surgery: the patient’s perspective-survey results from 259 patients. Surg Neurol. 2006;65(4):332-341. doi: 10.1016/j.surneu.2005.12.010 [DOI] [PubMed] [Google Scholar]
- 8.Gallagher MJ, Durnford AJ, Wahab SS, Nair S, Rokade A, Mathad N. Patient-reported nasal morbidity following endoscopic endonasal skull base surgery. Br J Neurosurg. 2014;28(5):622-625. doi: 10.3109/02688697.2014.887656 [DOI] [PubMed] [Google Scholar]
- 9.Kiraz M, Gunaldi O, Tanriverdi O, et al. Comparison of sinonasal complications of microscopic and endoscopic approaches for transsphenoidal hypophyseal surgery: prospective study. Turk Neurosurg. 2018;28(6):915-922. [DOI] [PubMed] [Google Scholar]
- 10.Kahilogullari G, Beton S, Al-Beyati ES, et al. Olfactory functions after transsphenoidal pituitary surgery: endoscopic versus microscopic approach. Laryngoscope. 2013;123(9):2112-2119. doi: 10.1002/lary.24037 [DOI] [PubMed] [Google Scholar]
- 11.Rotenberg BW, Saunders S, Duggal N. Olfactory outcomes after endoscopic transsphenoidal pituitary surgery. Laryngoscope. 2011;121(8):1611-1613. doi: 10.1002/lary.21890 [DOI] [PubMed] [Google Scholar]
- 12.Tam S, Duggal N, Rotenberg BW. Olfactory outcomes following endoscopic pituitary surgery with or without septal flap reconstruction: a randomized controlled trial. Int Forum Allergy Rhinol. 2013;3(1):62-65. doi: 10.1002/alr.21069 [DOI] [PubMed] [Google Scholar]
- 13.Yin LX, Low CM, Puccinelli CL, et al. Olfactory outcomes after endoscopic skull base surgery: A systematic review and meta-analysis. Laryngoscope. 2019;129(9):1998-2007. doi: 10.1002/lary.28003 [DOI] [PubMed] [Google Scholar]
- 14.Deems DA, Doty RL, Settle RG, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991;117(5):519-528. doi: 10.1001/archotol.1991.01870170065015 [DOI] [PubMed] [Google Scholar]
- 15.Hummel T, Nordin S. Olfactory disorders and their consequences for quality of life. Acta Otolaryngol. 2005;125(2):116-121. doi: 10.1080/00016480410022787 [DOI] [PubMed] [Google Scholar]
- 16.Keller A, Malaspina D. Hidden consequences of olfactory dysfunction: a patient report series. BMC Ear Nose Throat Disord. 2013;13(1):8. doi: 10.1186/1472-6815-13-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neuland C, Bitter T, Marschner H, Gudziol H, Guntinas-Lichius O. Health-related and specific olfaction-related quality of life in patients with chronic functional anosmia or severe hyposmia. Laryngoscope. 2011;121(4):867-872. doi: 10.1002/lary.21387 [DOI] [PubMed] [Google Scholar]
- 18.Santos DV, Reiter ER, DiNardo LJ, Costanzo RM. Hazardous events associated with impaired olfactory function. Arch Otolaryngol Head Neck Surg. 2004;130(3):317-319. doi: 10.1001/archotol.130.3.317 [DOI] [PubMed] [Google Scholar]
- 19.Pinto JM, Wroblewski KE, Kern DW, Schumm LP, McClintock MK. Olfactory dysfunction predicts 5-year mortality in older adults. PLoS One. 2014;9(10):e107541. doi: 10.1371/journal.pone.0107541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brämerson A, Johansson L, Ek L, Nordin S, Bende M. Prevalence of olfactory dysfunction: the skövde population-based study. Laryngoscope. 2004;114(4):733-737. doi: 10.1097/00005537-200404000-00026 [DOI] [PubMed] [Google Scholar]
- 21.Liu G, Zong G, Doty RL, Sun Q. Prevalence and risk factors of taste and smell impairment in a nationwide representative sample of the US population: a cross-sectional study. BMJ Open. 2016;6(11):e013246. doi: 10.1136/bmjopen-2016-013246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murphy C, Schubert CR, Cruickshanks KJ, Klein BE, Klein R, Nondahl DM. Prevalence of olfactory impairment in older adults. JAMA. 2002;288(18):2307-2312. doi: 10.1001/jama.288.18.2307 [DOI] [PubMed] [Google Scholar]
- 23.Schubert CR, Cruickshanks KJ, Klein BE, Klein R, Nondahl DM. Olfactory impairment in older adults: five-year incidence and risk factors. Laryngoscope. 2011;121(4):873-878. doi: 10.1002/lary.21416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vennemann MM, Hummel T, Berger K. The association between smoking and smell and taste impairment in the general population. J Neurol. 2008;255(8):1121-1126. doi: 10.1007/s00415-008-0807-9 [DOI] [PubMed] [Google Scholar]
- 25.Soyka MB, Serra C, Regli L, Meier E, Holzmann D. Long-term olfactory outcome after nasoseptal flap reconstructions in midline skull base surgery. Am J Rhinol Allergy. 2017;31(5):334-337. doi: 10.2500/ajra.2017.31.4463 [DOI] [PubMed] [Google Scholar]
- 26.Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4(7):28-37. [PMC free article] [PubMed] [Google Scholar]
- 27.Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL Jr. Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA. 2004;291(20):2441-2447. doi: 10.1001/jama.291.20.2441 [DOI] [PubMed] [Google Scholar]
- 28.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. doi: 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hart CK, Theodosopoulos PV, Zimmer LA. Olfactory changes after endoscopic pituitary tumor resection. Otolaryngol Head Neck Surg. 2010;142(1):95-97. doi: 10.1016/j.otohns.2009.09.032 [DOI] [PubMed] [Google Scholar]
- 30.Taha AN, Almefty R, Pravdenkova S, Al-Mefty O. Sequelae of autologous fat graft used for reconstruction in skull base surgery. World Neurosurg. 2011;75(5-6):692-695. doi: 10.1016/j.wneu.2011.01.023 [DOI] [PubMed] [Google Scholar]
- 31.Kim DH, Hong YK, Jeun SS, et al. Can tumor size be a predictive factor of olfactory dysfunction after endoscopic endonasal trans-sphenoidal approach? J Craniofac Surg. 2018;29(3):543-546. doi: 10.1097/SCS.0000000000004193 [DOI] [PubMed] [Google Scholar]
- 32.Chaaban MR, Chaudhry AL, Riley KO, Woodworth BA. Objective assessment of olfaction after transsphenoidal pituitary surgery. Am J Rhinol Allergy. 2015;29(5):365-368. doi: 10.2500/ajra.2015.29.4206 [DOI] [PubMed] [Google Scholar]
- 33.Hanson M, Patel PM, Betz C, Olson S, Panizza B, Wallwork B. Sinonasal outcomes following endoscopic anterior skull base surgery with nasoseptal flap reconstruction: a prospective study. J Laryngol Otol. 2015;129(suppl 3):S41-S46. doi: 10.1017/S002221511500047X [DOI] [PubMed] [Google Scholar]
- 34.Feinstein AR. Clinical biostatistics. XLI. Hard science, soft data, and the challenges of choosing clinical variables in research. Clin Pharmacol Ther. 1977;22(4):485-498. doi: 10.1002/cpt1977224485 [DOI] [PubMed] [Google Scholar]