Abstract
BACKGROUND/OBJECTIVES:
The American College of Cardiology (ACC) Geriatric Cardiology Section Leadership Council recently outlined 4 key domains (which are composed of 14 subdomains) that are important to assess in older adults with heart failure (HF). We sought to determine which geriatric domains/subdomains are routinely assessed, how they are assessed, and how they impact clinical management in the care of ambulatory older adults with HF.
DESIGN:
Survey.
SETTING:
Ambulatory.
PARTICIPANTS:
Fifteen active ACC member physicians from the geriatric cardiology community.
MEASUREMENTS:
Electronic survey assessing which domains/subdomains are currently assessed in these selected real-world practices, how they are assessed, and how they are incorporated into clinical management.
RESULTS:
Of 15 clinicians, 14 responded to the survey. The majority routinely assess 3 to 4 domains (median, 3; interquartile range, 3–4) and a range of 4 to 12 subdomains (median, 8; interquartile range, 6–11). All respondents routinely assess the medical and physical function domains, 71% routinely assess the mind/emotion domain, and 50% routinely assess the social domain. The most common subdomains included comorbidity burden (100%), polypharmacy (100%), basic function (93%), mobility (86%), falls risk (71%), frailty (64%), and cognition (57%). Sensory impairment (50%), social isolation (50%), nutritional status (43%), loneliness (7%), and financial means (7%) were least frequently assessed. There was significant heterogeneity with regard to the tools used to assess subdomains. Common themes for how the subdomains influenced clinical care included informing prognosis, informing risk-benefit of pharmacologic therapy and invasive procedures, and consideration for palliative care.
CONCLUSIONS:
While respondents routinely assess multiple domains and subdomains and view these as important to clinical care, there is substantial heterogeneity regarding which subdomains are assessed and the tools used to assess them. These observations provide a foundation that inform a research agenda with regard to providing holistic and patient-centered care to older adults with HF.
Keywords: frailty, heart failure, polypharmacy
The prevalence of heart failure (HF) rises sharply with increasing age.1 Consequently, the majority of the HF population is older than 75 years and typically contends with age-related medical conditions and challenges, such as cognitive impairment and frailty. The complexity of caring for older adults with HF was the subject of a recent review article by the American College of Cardiology (ACC) Geriatric Cardiology Section Leadership Council.2 In this review, the council proposed a “domain management” approach that outlined four key domains that warrant routine assessment in older adults with HF—medical, mind and emotion, physical function, and social environment (Figure 1).
Figure 1.
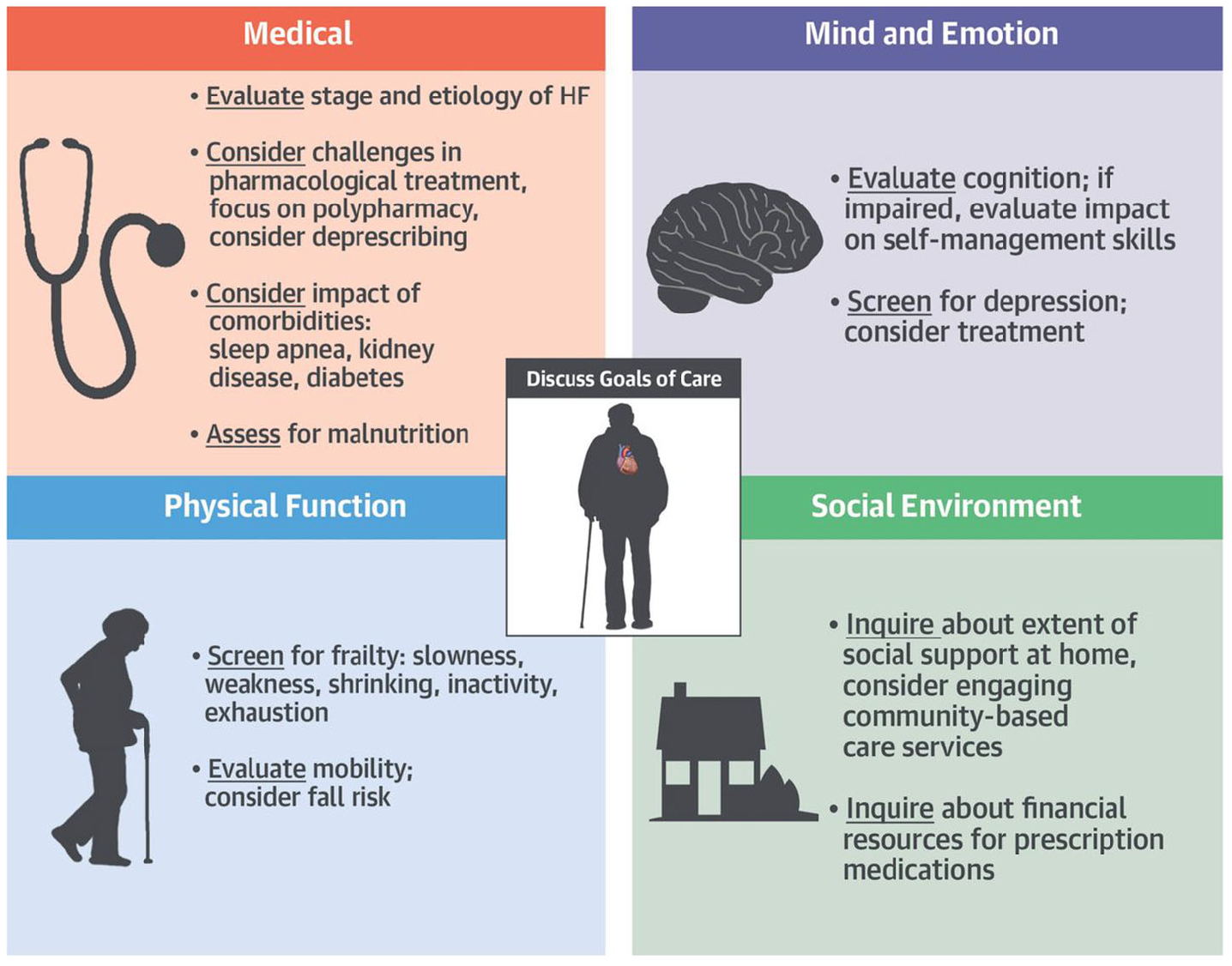
The domain management approach for older adults with heart failure (HF). Republished with permission from Gorodeski et al.2
While developing a holistic model to improve the care of older adults with HF is an important first step, the best strategies to implement this model into real-world practice are unknown. We, therefore, conducted a survey of several active physician members from the geriatric cardiology community, perhaps the strongest proponents of the domain management approach, to better understand which domains and subdomains are currently assessed in these selected real-world practices, how they are assessed, and how they are being incorporated into clinical management and decision making.
METHODS
Study Population
The ACC Geriatric Cardiology Section Leadership Council identified active ACC member physicians from the geriatric cardiology community who (1) provide ambulatory care to HF patients and (2) have previously self-reported implementing aspects of the domain management approach into their practices.
Data Collection
We created an electronic survey (Supplementary Text S1) of up to 39 total questions that inquired about which domains and subdomains are routinely assessed in practice (multiple choice), how they are assessed (free-text response), and how they are incorporated into clinical management and decision making (free-text response). The survey also inquired about the available personnel and time allocated to office visits (multiple choice) since these factors can impact whether performing these assessments is feasible.
Statistical Analysis
We calculated the proportion of respondents who reported routinely assessing each domain and subdomain and counted the number of different tools reported for each subdomain.
One investigator (P.G.) reviewed and coded free-text responses for the questions inquiring about ways that each subdomain affected clinical care and subsequently grouped them into themes. Two additional investigators (E.Z.G. and S.H.) independently reviewed and corroborated these themes; disagreements were resolved through discussion.
Finally, we calculated the distribution of time allocated for new and follow-up office visits and the proportion of respondents who had additional personnel to assist with implementing the domain management model.
RESULTS
Of 15 clinicians, 14 responded to the survey; respondents came from the United States and Canada (Supplementary Figure S1). Among respondents, 13 were trained in cardiology; 6 had additional training in HF, and 2 had additional training in geriatrics (Supplementary Table S1). One individual was trained in geriatrics alone. Of 14 respondents, 12 were affiliated with a large academic institution. Several respondents reported leading programs targeting a specific population in which geriatric issues are especially relevant—this included four geriatric cardiology programs, two HF with preserved ejection fraction programs, and one post–acute care program where care was primarily provided in nursing homes.
Domain and Subdomain Assessments
The majority of respondents reported routinely assessing 3 to 4 domains (median, 3; interquartile range, 3–4) and a range of 4 to 12 subdomains (median, 8; interquartile range, 6–11). As shown in Figure 2, all respondents routinely assessed some component of the medical and physical function domains, 71% assessed the mind/emotion domain, and 50% assessed the social domain. All respondents routinely assessed the medical subdomains of comorbidity burden and polypharmacy. They also commonly reported assessing several physical function subdomains, including basic function (93%), mobility (86%), falls risk (71%), and physical frailty (64%). The only other subdomain routinely assessed by over half of the cohort was the mind/emotion subdomain of cognition (57%).
Figure 2.
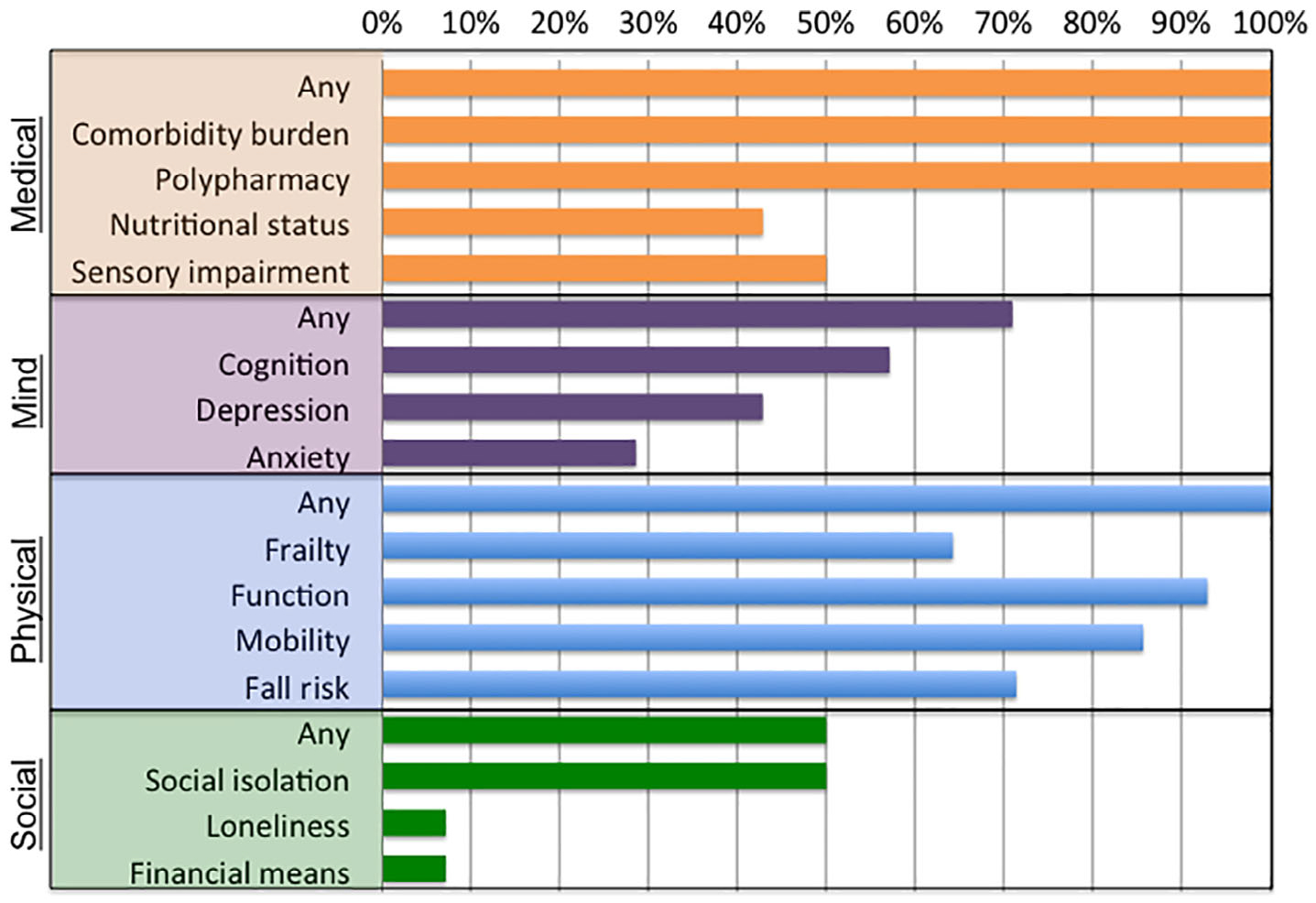
Percentage of respondents who routinely assessed each domain and subdomain.
Table 1 shows the methods that each respondent uses to assess each subdomain. Within the medical domain, respondents universally review the electronic medical record (EMR) to assess comorbidity burden and polypharmacy. Respondents reported seven different ways to assess nutritional status, with no clear consensus. Among respondents who assess sensory impairment, most reported simply asking patients about the presence of these impairments, while two respondents also reported using the EMR and two reported performing sensory examinations to gather this information.
Table 1.
Assessment and impact of domains and subdomains
| Domain | Subdomain | Methods used | Impact on care |
|---|---|---|---|
| Medical | Comorbidity burden |
|
|
| Polypharmacy |
|
|
|
| Nutritional status |
|
|
|
| Sensory impairment |
|
|
|
| Mind and emotion | Cognition |
|
|
| |||
| Depression |
|
|
|
| Anxiety |
|
|
|
| Physical function | Frailty |
|
|
| Function | |||
| |||
| |||
| Mobility |
|
|
|
| Fall risk |
|
|
|
| Social environment | Social isolation |
|
|
| Loneliness |
|
|
|
| Financial means |
|
|
Abbreviations: ADL, activity of daily living; EMR, electronic medical record; GAD-7, Generalized Anxiety Disorder seven-item scale; IADL, instrumental ADL; PHQ-2, Patient Health Questionnaire-2; SOF, Study of Osteoporotic Fracture.
Among respondents who routinely assess cognition, most use the Mini-Cog. The Mini-Cog consists of a three-word recall and clock drawing test and provides a simple screening test for cognitive impairment with a high negative predictive value.3,4 To assess for depression and anxiety, several respondents ask patients about associated symptoms; the use of validated tools, like the Patient Health Questionnaire-25 and Generalized Anxiety Disorder seven-item scale,6 was rarely reported.
There was significant variability with regard to the assessment of physical function subdomains. For physical frailty assessments, respondents reported using the Short Physical Performance Battery (SPPB),7 the Fried frailty index,8 gait speed, the Essential Frailty Toolset (a four-item test that combines chair stands, cognitive impairment, serum hemoglobin, and serum albumin),9 the sit-to-stand maneuver, and the Study of Osteoporotic Fracture (SOF) index (a three-item test that combines chair stands, weight loss, and a self-report of energy level).10 To assess for basic function, the majority of respondents reported inquiring about activities of daily living and instrumental activities of daily living (N = 8). Other reported methods included gait speed, New York Heart Association class, 6-minute walk test, the SPPB, the sit-to-stand maneuver, the SOF index, and the Kansas City Cardiomyopathy Questionnaire. One respondent reported simply watching the patient walk to the examination room and watching the patient get onto the examination table. To assess mobility, the majority of respondents reported measuring gait speed (N = 9). Other reported tests included chair stands and the SPPB. Finally, to assess fall risk, the majority of respondents report asking about a history of falls.
Respondents assess for social isolation and loneliness based on self-report. The one respondent who assesses financial means discusses the cost of medications.
Impact on Clinical Care
When asked about how various subdomains would impact clinical care, several common themes emerged (Table 1), including informing prognosis, informing risk-benefit of pharmacologic therapy and invasive procedures, and consideration for palliative care. There was significant overlap with regard to how the subdomains impacted various aspects of clinical care.
Respondent Time and Resources
There was significant variability in the duration of office visits (Supplementary Figure S2A); new patient visits ranged from 20 to 60 minutes, and follow-up visits ranged from 15 to 30 minutes. Approximately a third of respondents reported that they conduct assessments on their own, without the assistance of any other personnel (Supplementary Figure S2B).
DISCUSSION
The domain management approach has been proposed as the optimal care model for older adults with HF.2 Key findings were that respondents often assess multiple domains and subdomains, and they view these domains and subdomains as having an impact on several aspects of care; but the subdomains assessed and the tools used to assess these subdomains differed across respondents. These data provide insight on the relevance of the domain management approach to the care of older adults with HF and ongoing challenges to its implementation.
The domain management approach has yet to be validated; however, our findings indicate that aspects of this model are commonly used by active physician members in the geriatric cardiology community and provide important information for clinical care. Indeed, respondents frequently reported systematically assessing the medical, mind and emotion, and physical function domains; and they reported that almost every subdomain had an impact on multiple aspects of care. This included informing prognosis, which shapes discussions regarding health goals and priorities, as well as the risk-benefit ratios of various diagnostic studies and therapeutic interventions. For example, frailty may affect decision making for placement of an implantable cardioverter-defibrillator for primary prevention11 or implantation of a left ventricular assist device.12,13 Subdomain deficits are relevant to medication management as well. For example, the risk of adverse drug reactions increases in the setting of polypharmacy, cognitive impairment, and frailty.14–16 These deficits can alter the risk-benefit ratio of several different medications, perhaps even those in HF clinical practice guidelines. Indeed, many respondents in this study reported that they would consider deprescribing17 in the setting of polypharmacy, cognitive impairment, and frailty. Taken together, our findings provide empirical support for utilizing the domain management approach in the care of older adults with HF, and they highlight the need to formally validate the domain management approach as a care model to improve patient-centered outcomes in older adults with HF.
While we found that respondents commonly assessed multiple subdomains, we noted substantial heterogeneity in the methods used to identify deficits in these subdomains. This was especially noteworthy for frailty. While many of these tests include overlapping components (eg, the sit-to-stand maneuver is a component of the SPPB and the Essential Frailty Toolset), our findings demonstrate the lack of consensus on how best to assess frailty in older adults with HF. The variability across several other domains and subdomains observed in this study indicates that this lack of consensus is a global issue for components highlighted in the domain management approach. Accordingly, our findings highlight the need to develop best practices for assessing the domains and subdomains outlined in the domain management approach in older adults with HF.
While the majority of respondents typically assessed some aspect of the medical, mind and emotion, and physical function domains, the subdomains varied. For example, nutrition, sensory impairments, depressive symptoms, anxiety symptoms, social isolation, and loneliness were each routinely assessed by 50% or less of the cohort. This is particularly notable because we found this among a select cohort of perhaps the strongest proponents of the domain management approach. There are several possible reasons for this. First, clinicians may not have sufficient time to assess these subdomains, in part due to the current reimbursement structure, which does not account for time spent on conducting geriatric assessments. Respondents reported having as little as 20 minutes to see new patients; and many did not have additional support staff to assist with assessments. Second, it may be unclear how to best assess various subdomains. For example, respondents reported six different ways to assess frailty and seven different ways to assess nutrition. Third, it may not be clear what to do with the findings. For example, identifying loneliness might prompt a more thorough evaluation of social support, but interventions to address deficits in this area remain underdeveloped. Last, it is not clear which subdomains should be routinely assessed and which should be assessed on an as-needed basis. Taken together, these limitations support the need to systematically study the impact of the domain management approach in older adults with HF. In the meantime, it may be reasonable to develop a consensus on how best to assess various domains and subdomains and to devise strategies that directly address deficits when present. Practice models that incentivize comprehensive and patient-centric evaluations for older adults are needed18; whether the domain management approach can provide a formal model of such care is unknown and represents another potential area for future study.
There are some important limitations that we wish to note. We surveyed 15 active participants in the geriatric cardiology community, predominantly from academic settings. Accordingly, their responses reflect expertise and experience that is not representative of all clinicians caring for older adults with HF, and probably represent the current best-case scenario for the implementation of the domain management approach. Future study on how a broader cohort of clinicians caring for older adults with HF can incorporate the domain management approach into clinical care is warranted.
CONCLUSIONS
We describe how selected active physician members from the geriatric cardiology community incorporate the domain management approach in their clinical care of older adults with HF. While there were similarities in how various subdomains were reported to impact care, we found substantial heterogeneity regarding the subdomains that were routinely evaluated and the assessment tools that were used. These observations provide a foundation that informs a research agenda with regard to providing holistic and patient-centered care to older adults with HF.
Supplementary Material
Supplementary Figure S1: Geographic location of respondents.
Supplementary Figure S2: Time and resources available to implement the domain management approach, according to respondents. A, Distribution of time allotted for patient office visits. B, Percentage of respondents who reported having personnel available to help with domain and subdomain assessments.
Supplementary Table S1: Characteristics of survey respondents.
Supplementary Text S1: Survey questions.
ACKNOWLEDGMENTS
Financial Disclosure: Dr Goyal is supported by National Institutes of Health (NIH)/National Institute on Aging (NIA) grant R03AG056446 and American Heart Association grant 18IPA34170185. Dr Dodson is supported by NIH/NIA grant K23AG052463 and NIH/NIA grant R01AG062520. Dr Maurer is supported by NIH/NIA grant K24AG036778. Dr Hummel is supported by NIH/National Heart, Lung, and Blood Institute grant R01HL139813 and VA grant I01CX001636.
Sponsor’s Role: The sponsor did not have a role in the design, methods, subject recruitment, data collections, analysis, or preparation of the manuscript.
Footnotes
Conflicts of Interest: None.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- 1.Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492. [DOI] [PubMed] [Google Scholar]
- 2.Gorodeski EZ, Goyal P, Hummel SL, et al. Domain management approach to heart failure in the geriatric patient: present and future. J Am Coll Cardiol. 2018;71(17):1921–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003; 51(10):1451–1454. [DOI] [PubMed] [Google Scholar]
- 4.Tam E, Gandesbery BT, Young L, Borson S, Gorodeski EZ. Graphical instructions for administration and scoring the Mini-Cog: results of a randomized clinical trial. J Am Geriatr Soc. 2018;66(5):987–991. [DOI] [PubMed] [Google Scholar]
- 5.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. [DOI] [PubMed] [Google Scholar]
- 6.Lowe B, Decker O, Muller S, et al. Validation and standardization of the Generalized Anxiety Disorder screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. [DOI] [PubMed] [Google Scholar]
- 7.Volpato S, Cavalieri M, Sioulis F, et al. Predictive value of the Short Physical Performance Battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011;66(1):89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. [DOI] [PubMed] [Google Scholar]
- 9.Afilalo J, Lauck S, Kim DH, et al. Frailty in older adults undergoing aortic valve replacement: the FRAILTY-AVR study. J Am Coll Cardiol. 2017;70 (6):689–700. [DOI] [PubMed] [Google Scholar]
- 10.Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168(4):382–389. [DOI] [PubMed] [Google Scholar]
- 11.Chen MY, Orkaby AR, Rosenberg MA, Driver JA. Frailty, implantable cardioverter defibrillators, and mortality: a systematic review. J Gen Intern Med. 2019. 10.1007/s11606-019-05100-9.[Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunlay SM, Park SJ, Joyce LD, et al. Frailty and outcomes after implantation of left ventricular assist device as destination therapy. J Heart Lung Transplant. 2014;33(4):359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung CJ, Wu C, Jones M, et al. Reduced handgrip strength as a marker of frailty predicts clinical outcomes in patients with heart failure undergoing ventricular assist device placement. J Card Fail. 2014;20(5):310–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marcum ZA, Amuan ME, Hanlon JT, et al. Prevalence of unplanned hospitalizations caused by adverse drug reactions in older veterans. J Am Geriatr Soc. 2012;60(1):34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larson EB, Kukull WA, Buchner D, Reifler BV. Adverse drug reactions associated with global cognitive impairment in elderly persons. Ann Intern Med. 1987;107(2):169–173. [DOI] [PubMed] [Google Scholar]
- 16.Jyrkka J, Enlund H, Lavikainen P, Sulkava R, Hartikainen S. Association of polypharmacy with nutritional status, functional ability and cognitive capacity over a three-year period in an elderly population. Pharmacoepidemiol Drug Saf. 2011;20(5):514–522. [DOI] [PubMed] [Google Scholar]
- 17.Krishnaswami A, Steinman MA, Goyal P, et al. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol. 2019;73(20):2584–2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Geriatrics Society Expert Panel on the Care of Older Adults With Multimorbidity. Patient-centered care for older adults with multiple chronic conditions: a stepwise approach from the American Geriatrics Society. J Am Geriatr Soc. 2012;60(10):1957–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1: Geographic location of respondents.
Supplementary Figure S2: Time and resources available to implement the domain management approach, according to respondents. A, Distribution of time allotted for patient office visits. B, Percentage of respondents who reported having personnel available to help with domain and subdomain assessments.
Supplementary Table S1: Characteristics of survey respondents.
Supplementary Text S1: Survey questions.


