Abstract
We evaluated the effectiveness of pressure-controlled ventilation-volume guaranteed (PCV-VG) mode combined with open-lung approach (OLA) in patients during one-lung ventilation (OLV). First, 176 patients undergoing thoracoscopic surgery were allocated randomly to four groups: PCV+OLA (45 cases, PCV-VG mode plus OLA involving application of individualized positive end-expiratory pressure (PEEP) after a recruitment maneuver), PCV (44 cases, PCV-VG mode plus standard lung-protective ventilation with fixed PEEP of 5 cmH2O), VCV+OLA (45 cases, volume-controlled ventilation (VCV) plus OLA), and VCV (42 cases, VCV plus standard lung-protective ventilation). Mean airway pressure (Pmean), dynamic compliance (Cdyn), PaO2/FiO2 ratio, intrapulmonary shunt ratio (Qs/Qt), dead space fraction (VD/VT), and plasma concentration of neutrophil elastase were obtained to assess the effects of four lung-protective ventilation strategies. At 45 min after OLV, the median (interquartile range (IQR)) Pmean was higher in the PCV+OLA group (13.00 (12.00, 13.00) cmH2O) and the VCV+OLA group (12.00 (12.00, 14.00) cmH2O) than in the PCV group (11.00 (10.00, 12.00) cmH2O) and the VCV group (11.00 (10.00, 12.00) cmH2O) (P < 0.05); the median (IQR) Cdyn was higher in the PCV+OLA group (27.00 (24.00, 32.00) mL/cmH2O) and the VCV+OLA group (27.00 (22.00, 30.00) mL/cmH2O) than in the PCV group (23.00 (21.00, 25.00) mL/cmH2O) and the VCV group (20.00 (18.75, 21.00) mL/cmH2O) (P < 0.05); the median (IQR) Qs/Qt in the PCV+OLA group (0.17 (0.16, 0.19)) was significantly lower than that in the PCV group (0.19 (0.18, 0.20)) and the VCV group (0.19 (0.17, 0.20)) (P < 0.05); VD/VT was lower in the PCV+OLA group (0.18 ± 0.05) and the VCV+OLA group (0.19 ± 0.07) than in the PCV group (0.21 ± 0.07) and the VCV group (0.22 ± 0.06) (P < 0.05). The concentration of neutrophil elastase was lower in the PCV+OLA group than in the PCV, VCV+OLA, and VCV groups at total-lung ventilation 10 min after OLV (162.47 ± 25.71, 198.58 ± 41.99, 200.84 ± 22.17, and 286.95 ± 21.10 ng/mL, resp.) (P < 0.05). In conclusion, PCV-VG mode combined with an OLA strategy leads to favorable effects upon lung mechanics, oxygenation parameters, and the inflammatory response during OLV.
1. Introduction
One-lung ventilation (OLV) has been used routinely in thoracic surgery to provide an optimal visual field for a surgical procedure on a collapsed lung. Unfortunately, this approach creates a “shunt-like” effect through the nondependent lung and results in hypoxemia [1]. Furthermore, OLV and surgical trauma are accompanied by the release of excessive amounts of inflammatory mediators and neutrophil elastase, which lead to pulmonary infection and systemic inflammatory response syndrome [2, 3].
Lung-protective ventilation, consisting a tidal volume (VT) of 5–6 mL/kg of predicted body weight (PBW) and positive end-expiratory pressure (PEEP) of 5 cmH2O with an alveoli recruitment maneuver at 20 cmH2O for 15–20 s, can reduce the risk of ventilator-induced lung injury [4]. However, except for low VT, the advantages of appropriate PEEP with or without an alveoli recruitment maneuver have not been established exactly [5, 6]. Alternatively, an open-lung approach (OLA), in which the individualized PEEP is determined by PEEP titration after an alveoli recruitment maneuver, can contribute to favorable physiologic effects [7, 8].
The literature regarding the ideal ventilation mode on pulmonary outcomes for OLV is controversial [9–11]. Volume-controlled ventilation (VCV) ensures a stable minute ventilation volume, but this mode generates a high airway pressure with subsequent volutrauma and barotrauma and leads to uneven distribution of gas in the lungs. Pressure-controlled ventilation (PCV) offers the benefits of lower airway pressure with a decelerating flow pattern, but it can provoke lung injury due to a tractive force on alveoli [12]. Pressure-controlled ventilation-volume guaranteed (PCV-VG) mode is a relatively innovative ventilation model introduced to the operating theatre. In PCV-VG mode, initially a preset VT is transmitted at a lower airway pressure by a decelerating flow. Upon calculation of a patient's pulmonary compliance and inspiratory pressure, the ventilator automatically adjusts the airway pressure of the next breath according to the previous breath's measured exhaled VT [13, 14]. Recently, different results by comparing the efficacy of PCV-VG over other modes were published [9, 14]. Nevertheless, lung-protective ventilation applied to PCV-VG mode has not been studied deeply, and whether PCV-VG combined with an OLA is superior to VCV plus standard lung-protective ventilation during OLV is not known.
We carried out the study to explore the benefits of PCV-VG mode in combination with an OLA on lung mechanics, oxygenation parameters, and the inflammatory response during thoracic surgery.
2. Materials and Methods
2.1. Study Population
The ethics committee of Hebei General Hospital (Hebei, China) approved the study protocol. Each participant (or family member) provided written informed consent. The study was registered with the Chinese Clinical Trial Registry (ChiCTR1900020895).
The study enrolled patients with ASA physical status I–III scheduled for elective thoracoscopic surgery requiring OLV. Patients were excluded if they met any of the following criteria: age < 18 years, body mass index ≥ 35 kg/m2, pneumothorax or giant bullae, chronic lung disease or pulmonary infection within one month of study initiation, previous thoracic surgery, and contraindication to PEEP (high intracranial pressure, hypovolemic shock, or right-heart failure). Dropout criteria were a change in type of surgical procedure to thoracotomy, intraoperative bleeding ≥ 500 mL, and OLV duration < 45 min.
2.2. Randomization
Participants were assigned to one of four lung-protective ventilation strategies using a computer-generated randomization sequence, with an allocation of 1 : 1 : 1 : 1.
2.3. Anesthesia and Surgery
After placement of monitors, anesthesia induction and endobronchial intubation were achieved with 0.3 mg/kg etomidate, 0.3 μg/kg sufentanil, and 1.0 mg/kg rocuronium. The location of the left- or right-sided double-lumen tube (DLT) was regulated by a fiberoptic bronchoscope in supine and lateral positions. Anesthesia was maintained with sevoflurane, remifentanil, and rocuronium. Sevoflurane was titrated to keep the bispectral index between 40 and 60. Lactated Ringer's solution was infused continuously at 3–5 mL/kg/h. All patients received patient-controlled intravenous analgesia after surgery. And patients were treated in the thoracic surgery intensive care unit (ICU) after surgery.
2.4. General Ventilator Strategy
After endobronchial intubation, all patients in the four groups were ventilated with an anesthesia ventilator (Avance CS2 Pro; GE Healthcare, Piscataway, NJ, USA).
Before OLV, all participants were set the same ventilation parameters, consisting of a fraction of inspired oxygen (FiO2) of 1.0, VT of 8 mL/kg PBW, and an initial PEEP of 5 cmH2O (which was maintained in the PCV group and the VCV group throughout the whole procedure).
During OLV, all individuals received a VT of 5–6 mL/kg PBW with FiO2 of 0.8. The inspiratory : expiratory (I : E) ratio was 1 : 2, and ventilation frequency was adjusted to maintain end-tidal carbon dioxide partial pressure (PETCO2) between 35 and 45 mmHg. The maximal acceptable peak airway pressure (Ppeak) was set at 30 cmH2O, and if Ppeak was exceeded, VCV was switched to PCV.
2.5. Alveoli Recruitment Maneuver and Decremental PEEP Trial
OLV was initiated after rechecking the correct position of the DLT. The dependent lung had a standard alveoli recruitment maneuver. The ventilation mode was changed from VCV to PCV with a driving pressure of 20 cmH2O and respiratory rate of 15 breaths per minute, PEEP of 5 cmH2O, I : E of 1 : 1, and FiO2 of 1.0. PEEP was increased at a step size of 5 cmH2O, and 10 breaths were maintained at each step (5, 10, 15, and 20 cmH2O) until recruitment of opening pressure up to 40 cmH2O (20 cmH2O PEEP and 20 cmH2O of driving pressure) was applied for 20 breaths.
If the hemodynamics were unstable during the alveoli recruitment maneuver phase (a decrease in mean arterial pressure (MAP) > 30%), the alveoli recruitment maneuver was interrupted and vasoactive drugs given; after hemodynamic stability, a new alveoli recruitment maneuver was implemented.
After the first alveoli recruitment maneuver had been accomplished, individualized PEEP was titrated through a trial with decreased PEEP. PEEP was reduced in steps of 2 cmH2O with each PEEP level (20, 18, 16, 14, 12, 10, 8, and 6 cmH2O) and held for 15 s until the greatest dynamic compliance (Cdyn) was produced, which was considered to be the individualized or optimal PEEP. Then, a new alveoli recruitment maneuver was carried out as described above (Figure 1).
Figure 1.
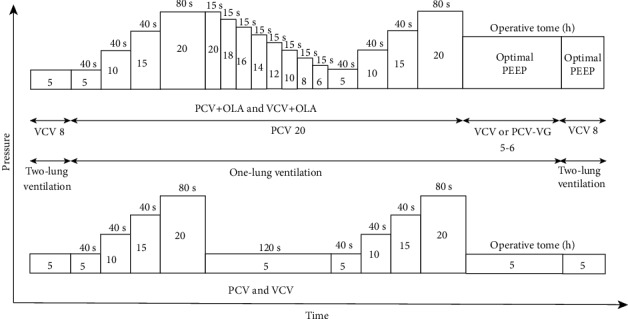
PCV 20: pressure-controlled ventilation mode with 20 cmH2O; VCV 8: volume-controlled ventilation mode with tidal volume set to 8 mL/kg; VCV or PCV-VG 5-6: volume-controlled ventilation mode or pressure-controlled ventilation-volume guaranteed mode with tidal volume set to 5 to 6 mL/kg.
2.6. Specific Intraoperative Ventilatory Management
In the PCV+OLA group, after the second alveoli recruitment maneuver, the ventilation mode was changed to PCV-VG during OLV, and the optimal PEEP was established and maintained throughout the whole study period.
In the VCV+OLA group, patients received the same procedures (alveoli recruitment maneuver and trial of decreased PEEP), the ventilation mode was switched to VCV during OLV, and the optimal PEEP maintained throughout the whole study period.
In the PCV and VCV groups, the same procedure (alveoli recruitment maneuver) was followed except for the PEEP titration. Patients received PCV-VG or VCV plus fixed PEEP (5 cmH2O) during OLV, respectively.
It is worth noting that alveoli recruitment maneuver was performed after OLV without PEEP titration. The ventilation mode was changed to VCV, and the PEEP value of each group was consistent with that during OLV.
2.7. Measurements
Studied variables were collected at three time points: (i) T1: total-lung ventilation 10 min after intubation; (ii) T2: OLV for 45 min; and (iii) T3: total-lung ventilation 10 min after OLV.
The studied endpoints were partial pressure of arterial carbon dioxide (PaCO2), pH, VT, PEEP, mean airway pressure (Pmean), Cdyn, Ppeak, dead space fraction (VD/VT), intrapulmonary shunt ratio (Qs/Qt), arterial partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2 ratio), and the plasma concentration of neutrophil elastase.
Parameters were calculated using the following equations:
| (1) |
| (2) |
whereby PA‐aDO2 = [FiO2 × (PB − PH2O)] − (PaCO2/R) − PaO2.
PA-aDO2 is the alveolar-arterial oxygen difference; PB is the barometric pressure (760 mmHg); PH2O is the vapor pressure of water (47 mmHg); R is the respiratory quotient (0.8).
The plasma concentration of neutrophil elastase was measured by enzyme-linked immunosorbent assays at T1 and T3.
Postoperative endpoints in the four groups were recorded: prevalence of pneumonia, atelectasis, and acute respiratory failure; duration of ICU stay; and duration of hospital stay after surgery.
3. Statistical Analyses
The sample size for our study was determined according to a pilot study, with an α level of 0.05, power of 0.8, and effect size of 0.3. Assuming a dropout of 30% of cases, 200 patients (50 patients per group) were included in each group.
Statistical data were analyzed using SPSS 22.0 (IBM, Armonk, NY, USA). The Shapiro-Wilk test was used for data with a normal distribution. Continuous variables are given as the mean ± standard deviation (SD) or median (interquartile range (IQR)). Categorical variables are described as numbers. Categorical data were analyzed using the chi-squared test. Data with a normal distribution were compared among the four groups using one-way ANOVA with LSD-t as the post hoc test. The Kruskal-Wallis test was used to compare multiple groups on continuous variables with a nonnormal distribution. P < 0.05 (two-sided) was considered significant for all tests.
4. Results
4.1. Demographic and Intraoperative Characteristics of Patients
Initially, 200 patients were assessed for eligibility, and 176 patients completed the study (Figure 2). The four groups were balanced in terms of demographics and data relating to the surgical procedure (P > 0.05) (Tables 1 and 2).
Figure 2.
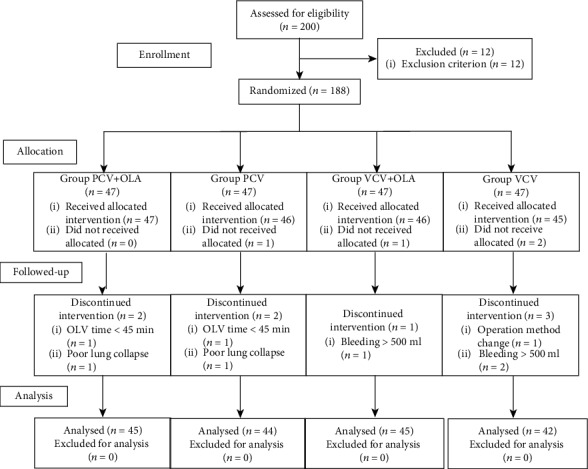
The study flow diagram.
Table 1.
Patients' characteristics.
| PCV+OLA (n = 45) |
PCV (n = 44) |
VCV+OLA (n = 45) |
VCV (n = 42) |
P | |
|---|---|---|---|---|---|
| Age (years) | 57.44 ± 8.47 | 58.93 ± 7.07 | 59.02 ± 10.12 | 57.76 ± 8.05 | 0.185 |
| Sex (F/M) | 19/26 | 22/22 | 22/23 | 20/22 | 0.887 |
| Height (cm) | 165.29 ± 7.05 | 165.19 ± 7.58 | 165.71 ± 8.89 | 165.50 ± 8.43 | 0.714 |
| BMI (kg/m2) | 25.28 ± 2.72 | 24.85 ± 3.17 | 24.45 ± 2.78 | 24.75 ± 3.40 | 0.583 |
| PBW (kg) | 59.31 ± 8.44 | 59.93 ± 8.65 | 59.69 ± 10.12 | 59.62 ± 8.70 | 0.888 |
| ASA (I/II/III) | 4/31/10 | 6/26/12 | 5/28/12 | 3/28/11 | 0.731 |
| ARISCAT score | |||||
| Intermediate/high | 29/16 | 28/16 | 30/15 | 22/20 | 0.527 |
| Preoperative haemoglobin (mg/dL) | 133.60 (124.80, 144.40) | 137.55 (119.80, 144.40) | 131.00 (123.95, 140.80) | 138.20 (128.58, 145.88) | 0.583 |
| Comorbidity | |||||
| Hypertension | 12 (26.7%) | 22 (50.0%) | 14 (31.1%) | 18 (42.9%) | 0.090 |
| Diabetes | 2 (4.4%) | 8 (18.2%) | 6 (13.3%) | 4 (9.5%) | 0.214 |
| CVD | 10 (22.2%) | 4 (9.1%) | 4 (8.9%) | 6 (14.3%) | 0.215 |
| Smoking | |||||
| No/current | 38/7 | 33/11 | 32/13 | 32/10 | 0.498 |
| Creatinine (μmol/L) | 67.70 (60.95, 74.95) | 69.25 (59.13, 80.45) | 68.90 (61.70, 75.05) | 69.50 (63.68, 79.43) | 0.714 |
| LEF (%) | 65.00 (62.00, 70.00) | 65.00 (61.00, 67.75) | 66.00 (63.00, 68.00) | 65.50 (61.75, 69.00) | 0.720 |
| FVC (L) | 3.21 ± 0.73 | 3.11 ± 0.80 | 3.05 ± 0.71 | 3.34 ± 0.81 | 0.102 |
| FEV1 (%) | 98.00 (89.00, 104.00) | 95.50 (82.95, 105.48) | 96.00 (80.50, 104.50) | 101.00 (89.00, 110.25) | 0.287 |
| FEV1/FVC (%) | 79.84 ± 6.20 | 77.94 ± 8.10 | 78.90 ± 9.41 | 78.68 ± 9.50 | 0.632 |
| Preoperative SaO2 (%) | 97.30 (95.85, 97.80) | 97.10 (96.20, 97.65) | 96.70 (95.95, 97.55) | 97.10 (96.28, 98.00) | 0.795 |
Data are expressed as mean ± standard deviation (SD), numbers, or median (interquartile range). F: female; M: male; PBW: predicted body weight, calculated as follows: for women (45.5 + 0.91) × (height in cm − 152.4), for men (50.0 + 0.91) × (height in cm − 152.4); ASA: American Society of Anesthesiologist; BMI: body mass index; CVD: coronary vessel disease; LEF: left ventricle ejection fraction; FVC: forced vital capacity; FEV1: forced expiratory volume in the first second; SaO2: oxyhaemoglobin saturation.
Table 2.
Intraoperative characteristics.
| PCV+OLA (n = 45) |
PCV (n = 44) |
VCV+OLA (n = 45) |
VCV (n = 42) |
P | |
|---|---|---|---|---|---|
| Type of surgery | |||||
| Lobectomy | 21 (46.7%) | 24 (54.5%) | 25 (55.6%) | 23 (54.8%) | 0.664 |
| Wedge resection | 20 (44.4%) | 13 (29.5%) | 13 (28.9%) | 12 (28.6%) | |
| Segmentectomy | 4 (8.9%) | 7 (15.9%) | 7 (15.6%) | 7 (16.7%) | |
| Double lumen tube | |||||
| Left/right | 39/6 | 42/2 | 43/2 | 39/3 | 0.331 |
| Vasoactive drugs | 25 (55.6%) | 23 (52.3%) | 26 (57.8%) | 22 (52.4%) | 0.945 |
| Volume of fluids (mL) | 1002.50 (922.50, 1158.54) | 1028.75 (925.52, 1163.00) | 1068.75 (902.63, 1153.65) | 1057.50 (917.71, 1270.94) | 0.685 |
| Urine output (mL) | 300.00 (200.00, 500.00) | 275.00 (200.00, 400.00) | 300.00 (200.00, 400.00) | 300.00 (200.00, 500.00) | 0.401 |
| Duration of operation (min) | 140.00 (100.00, 193.50) | 147.50 (107.50, 189.50) | 155.00 (107.50, 190.00) | 170.00 (114.25, 220.50) | 0.339 |
| Duration of anesthesia (min) | 180.00 (140.00, 237.50) | 195.00 (141.25, 225.00) | 200.00 (145.00, 228.50) | 212.50 (157.50, 262.50) | 0.400 |
| Duration of OLV (min) | 120.00 (87.50, 175.00) | 133.00 (96.25, 170.00) | 135.00 (92.50, 175.00) | 160.00 (100.00, 200.00) | 0.352 |
| Blood loss (mL) | 40.00 (10.00, 50.00) | 40.00 (10.00, 50.00) | 50.00 (10.00, 50.00) | 50.00 (10.00, 100.00) | 0.489 |
| HR | |||||
| T1 | 76.16 ± 7.78 | 74.00 ± 8.86 | 74.93 ± 8.05 | 73.79 ± 9.36 | 0.548 |
| T2 | 77.04 ± 7.07 | 74.23 ± 6.63 | 76.78 ± 8.08 | 77.00 ± 6.86 | 0.226 |
| T3 | 76.31 ± 5.76 | 75.50 ± 6.18 | 77.20 ± 6.44 | 76.41 ± 5.92 | 0.539 |
| MAP | |||||
| T1 | 89.44 ± 9.10 | 89.34 ± 8.14 | 91.73 ± 7.20 | 91.05 ± 8.16 | 0.422 |
| T2 | 93.00 ± 6.54 | 92.09 ± 7.40 | 92.20 ± 7.18 | 92.98 ± 7.97 | 0.343 |
| T3 | 91.87 ± 5.23 | 90.93 ± 6.52 | 91.69 ± 6.86 | 90.55 ± 7.22 | 0.138 |
Data are expressed as mean ± standard deviation (SD), numbers, or median (interquartile range). OLV: one-lung ventilation; HR: heart rate; T1: total-lung ventilation 10 min after induction; T2: one-lung ventilation 45 min; T3: total-lung ventilation 10 min after one-lung ventilation; MAP: mean arterial pressure.
4.2. Mechanics of the Respiratory System
Compared with the PCV and VCV groups (both 5.00 cmH2O), the median (IQR) PEEP was higher in the PCV+OLA group (8.00 (8.00, 10.00) cmH2O) and the VCV+OLA group (10.00 (8.00, 12.00) cmH2O) (P < 0.001).
At T2, the median (IQR) Pmean was higher in the PCV+OLA group (13.00 (12.00, 13.00) cmH2O) and the VCV+OLA group (12.00 (12.00, 14.00) cmH2O) than in the PCV and VCV groups (both 11.00 (10.00, 12.00) cmH2O) (P < 0.05). The median (IQR) Cdyn was higher in the PCV+OLA group (27.00 (24.00, 32.00) mL/cmH2O) and the VCV+OLA group (27 (22.00, 30.00) mL/cmH2O) than in the PCV group (23.00 (21.00, 25.00) mL/cmH2O) and the VCV group (20.00 (18.75, 21.00) mL/cmH2O) at T2 (P < 0.05). At T2, Ppeak showed no difference in the PCV+OLA and PCV groups (P = 0.320) or the VCV+OLA and VCV groups (P = 0.856) (Table 3).
Table 3.
Ventilatory parameters, respiratory system mechanics, blood gas, and oxygenation parameters.
| PCV+OLA (n = 45) |
PCV (n = 44) |
VCV+OLA (n = 45) |
VCV (n = 42) |
P | |
|---|---|---|---|---|---|
| V T (mL) | |||||
| T1 | 432.00 (405.00, 475.00) | 429.50 (404.50, 499.75) | 445.00 (399.50, 502.00) | 449.50 (410.25, 503.25) | 0.841 |
| T2 | 314.09 ± 34.35 | 324.98 ± 39.64 | 318.29 ± 47.47 | 326.90 ± 44.93 | 0.451 |
| T3 | 431.00 (408.00, 500.50) | 442.50 (411.50, 502.00) | 452.00 (405.00, 503.00) | 441.00 (407.00, 507.25) | 0.936 |
| PEEP (cmH2O) | |||||
| T1 | 5.00 | 5.00 | 5.00 | 5.00 | — |
| T2 | 8.00 (8.00, 10.00)∗▲ | 5.00 | 10.00 (8.00, 12.00)∗▲ | 5.00 | <0.001 |
| T3 | 8.00 (8.00, 10.00)∗▲ | 5.00 | 10.00 (8.00, 12.00)∗▲ | 5.00 | <0.001 |
| P peak (cmH2O) | |||||
| T1 | 18.71 ± 2.62 | 17.93 ± 2.98 | 19.16 ± 2.43 | 18.64 ± 3.45 | 0.255 |
| T2 | 21.00 (20.00, 22.00)△▲ | 22.00 (19.25, 23.00)△▲ | 24.00 (23.00, 25.00) | 23.00 (21.00, 25.00) | <0.001 |
| T3 | 20.22 ± 2.39 | 18.82 ± 2.95△ | 21.84 ± 2.49 | 18.69 ± 4.69△ | <0.001 |
| P mean (cmH2O) | |||||
| T1 | 10.00 (9.00, 11.00) | 10.00 (9.00, 11.00) | 10.00 (9.00, 11.00) | 10.00 (9.00, 11.00) | 0.245 |
| T2 | 13.00 (12.00, 13.00)∗▲ | 11.00 (10.00, 12.00) | 12.00 (12.00, 14.00)∗▲ | 11.00 (10.00, 12.00) | <0.001 |
| T3 | 12.00 (11.00, 13.00)∗▲ | 11.00 (10.00, 12.00) | 12.00 (11.00, 13.00)∗▲ | 10.00 (8.00, 11.00) | <0.001 |
| Cdyn (mL/cmH2O) | |||||
| T1 | 46.60 ± 5.60 | 46.36 ± 6.57 | 45.78 ± 7.51 | 46.17 ± 6.25 | 0.943 |
| T2 | 27.00 (24.00, 32.00)∗▲ | 23.00 (21.00, 25.00) | 27.00 (22.00, 30.00)∗▲ | 20.00 (18.75, 21.00) | <0.001 |
| T3 | 47.33 ± 5.59∗▲ | 44.78 ± 4.25▲ | 46.18 ± 5.22▲ | 43.12 ± 5.20 | 0.001 |
| PaCO2 (mmHg) | |||||
| T1 | 42.29 ± 3.76 | 43.30 ± 3.76 | 43.78 ± 4.38 | 43.57 ± 4.77 | 0.345 |
| T2 | 44.43 ± 3.90 | 44.17 ± 4.89 | 45.26 ± 4.71 | 44.20 ± 4.81 | 0.485 |
| T3 | 43.00 (39.50, 47.00) | 45.00 (41.00, 47.00) | 46.00 (41.00, 48.00) | 44.00 (41.00, 47.25) | 0.455 |
| pH | |||||
| T1 | 7.40 ± 0.03 | 7.39 ± 0.03 | 7.39 ± 0.04 | 7.39 ± 0.04 | 0.402 |
| T2 | 7.38 (7.35, 7.40) | 7.38 (7.35, 7.42) | 7.37 (7.39, 7.40) | 7.38 (7.35, 7.41) | 0.633 |
| T3 | 7.38 ± 0.04 | 7.38 ± 0.03 | 7.38 ± 0.05 | 7.38 ± 0.04 | 0.796 |
| V D/VT | |||||
| T1 | 0.17 ± 0.04 | 0.18 ± 0.06 | 0.19 ± 0.06 | 0.19 ± 0.05 | 0.210 |
| T2 | 0.18 ± 0.05∗▲ | 0.21 ± 0.07 | 0.19 ± 0.07∗▲ | 0.22 ± 0.06 | 0.003 |
| T3 | 0.16 (0.13, 0.21)∗▲ | 0.20 (0.17, 0.24) | 0.19 (0.14, 0.22) | 0.21 (0.17, 0.24) | <0.001 |
| Qs/Qt | |||||
| T1 | 0.16 ± 0.03 | 0.16 ± 0.03 | 0.16 ± 0.04 | 0.16 ± 0.03 | 0.873 |
| T2 | 0.17 (0.16, 0.19)∗▲ | 0.19 (0.18, 0.20) | 0.18 (0.17, 0.19) | 0.19 (0.17, 0.20) | 0.006 |
| T3 | 0.17 ± 0.03 | 0.17 ± 0.03 | 0.17 ± 0.03 | 0.18 ± 0.03 | 0.280 |
| PaO2/FiO2 ratio | |||||
| T1 | 341.91 ± 78.37 | 350.95 ± 62.70 | 342.47 ± 81.27 | 352.10 ± 74.73 | 0.875 |
| T2 | 173.75 (138.13, 221.87)▲ | 153.13 (109.38, 185.94) | 166.25 (146.25, 200.63)▲ | 134.38 (106.25, 180.63) | 0.002 |
| T3 | 330.69 ± 65.24 | 327.40 ± 64.31 | 317.60 ± 65.71 | 304.12 ± 73.40 | 0.264 |
Data are expressed as mean ± standard deviation (SD) or median (interquartile range). VT: tidal volume; T1: total-lung ventilation 10 min after induction; T2: one-lung ventilation 45 min; T3: total-lung ventilation 10 min after one-lung ventilation; PEEP: positive end-expiratory pressure; Ppeak: peak airway pressure; Pmean: mean airway pressure; Cdyn: dynamic compliance; PaCO2: partial pressure of arterial carbon dioxide; VD/VT: dead space fraction; Qs/Qt: intrapulmonary shunt ratio; PaO2/FiO2: arterial partial pressure of oxygen/fraction of inspired oxygen. ∗P < 0.05 versus PCV, △P < 0.05 versus VCV+OLA, and ▲P < 0.05 versus VCV.
4.3. Variables in Ventilation Efficiency
At T2, the median (IQR) Qs/Qt in the PCV+OLA group (0.17 (0.16, 0.19)) was significantly lower than that in the PCV group (0.19 (0.18, 0.20)) and the VCV group (0.19 (0.17, 0.20)) (P < 0.05). VD/VT was lower in the PCV+OLA group (0.18 ± 0.05) and the VCV+OLA group (0.19 ± 0.07) than that in the PCV group (0.21 ± 0.07) and the VCV group (0.22 ± 0.06) at T2 (P < 0.05). Compared with the VCV group, the PaO2/FiO2 ratio increased in the PCV+OLA and VCV+OLA groups (median (IQR) 173.75 (138.13, 221.87) vs. 134.38 (106.25, 180.63); 166.25 (146.25, 200.63) vs. 134.38 (106.25, 180.63), P < 0.05) (Table 3).
4.4. Plasma Concentration of Neutrophil Elastase
There was no significant difference in the plasma neutrophil elastase level among the four groups at T1 (P > 0.05). The plasma concentration of neutrophil elastase was lower in the PCV+OLA group than that in the PCV, VCV+OLA, and VCV groups at T3 (162.47 ± 25.71, 198.58 ± 41.99, 200.84 ± 22.17, and 286.95 ± 21.10, ng/mL, resp.) (P < 0.05) (Figure 3).
Figure 3.
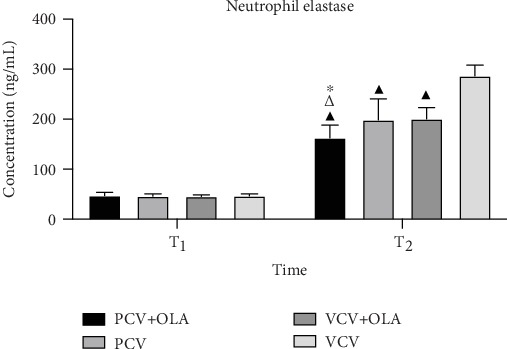
The plasma concentration of neutrophil elastase. Data are expressed as mean ± standard deviation (SD). ∗P < 0.05 versus PCV, △P < 0.05 versus VCV+OLA, and ▲P < 0.05 versus VCV.
4.5. Other Clinical Endpoints
The duration of ICU stay in the PCV+OLA group was shorter compared with that in PCV, VCV+OLA, and VCV groups (median (IQR) 32.00 (25.00, 37.00), 39.75 (32.88, 43.00), 39.50 (27.00, 43.50), and 39.60 (24.88, 43.70) h, resp.) (P < 0.05). There were no significant differences in the duration of hospital stay and the prevalence of pneumonia, atelectasis, and acute respiratory failure in the four groups after surgery (P > 0.05) (Table 4).
Table 4.
Other clinical endpoints.
| PCV+OLA (n = 45) |
PCV (n = 44) |
VCV+OLA (n = 45) |
VCV (n = 42) |
P | |
|---|---|---|---|---|---|
| Pneumonia | 2 (4.4%) | 5 (11.4%) | 4 (8.9%) | 7 (16.7%) | 0.312 |
| Atelectasis | 1 (2.2%) | 4 (9.1%) | 2 (4.4%) | 6 (14.3%) | 0.148 |
| Acute respiratory failure | 0 (0%) | 1 (2.3%) | 1 (2.2%) | 4 (9.5%) | 0.096 |
| The duration of ICU stay (hours) | 32.00 (25.00, 37.00)∗△▲ | 39.75 (32.88, 43.00) | 39.50 (27.00, 43.50) | 39.60 (24.88, 43.70) | <0.001 |
| The duration of hospital stay after surgery (days) | 6.00 (5.00, 7.00) | 6.00 (5.00, 8.00) | 6.00 (5.00, 8.00) | 6.00 (4.75, 7.00) | 0.204 |
Data are expressed as median (interquartile range) or numbers. ICU: intensive care unit. ∗P < 0.05 versus PCV, △P < 0.05 versus VCV+OLA, and ▲P < 0.05 versus VCV.
5. Discussion
The randomized controlled trial revealed that the ventilation strategy of PCV-VG plus OLA during OLV leads to preferable levels of Cdyn, PaO2/FiO2 ratio, and appropriate levels of Pmean, VD/VT, Qs/Qt, and neutrophil elastase. Additionally, the duration of ICU stay was shorter in the PCV+OLA group compared with the other three groups. These results suggest that the ventilation strategy of PCV-VG combined with OLA during OLV is beneficial for patients undergoing thoracic surgery.
Patients undergoing OLV are susceptible to hypoxemia due to shunting of blood or imbalance of ventilation and pulmonary perfusion. And the practice of OLV is an independent hazard factor for postoperative pulmonary complications (PPCs), as a result of direct surgical trauma of the nonventilated lung, exposed to high strain and nonphysiologic VT of the ventilated lung [15, 16]. Multiple mechanisms can cause lung tissue damage and inflammatory cytokine release, which often ahead of pneumonia and systemic inflammatory response syndrome ultimately affect the clinical prognosis of patients undergoing thoracic surgery [17, 18].
Usually, the lung-protective ventilation strategy, which has taken low VT as the core, is accepted by anesthesiologists as an effective way to alleviate ventilator-induced lung injury [19]. However, the application of a low VT without sufficient PEEP may be relevant to cyclic alveolar derecruitment with consequent promote atelectrauma [6]. PEEP can prevent atelectasis effectively, but the optimal PEEP level is not known. Pereira et al. observed that PEEP varied markedly among individuals and stated that intraoperative individualized PEEP settings could lower the risk of postoperative atelectasis while improving driving pressure and oxygenation [20]. On the contrary, a study showed that different perioperative OLA with individualized PEEP in major abdominal surgery did not reduce the prevalence of postoperative complications when compared with conventional lung-protective ventilation strategy [21]. Most protective ventilation strategies (including the OLA) were undertaken under VCV mode, which could pose a potential risk of high airway pressure and trigger pulmonary inflammatory response compared with PCV or PCV-VG [10, 22]. The PCV-VG mode has features of PCV and VCV, which creates lower airway pressure than that seen with VCV accompanied with improvement in oxygenation and reduction in the pulmonary shunt [1, 13]. However, Byun and colleagues indicated that the application of VT of 6 mL/kg with zero PEEP under PCV-VG led to a high risk of intraoperative hypoxemia [23]. Moreover, many studies found that compared with VCV, PCV-VG did not significantly improve intraoperative oxygenation [24, 25]. Hence, we designed this study to explore the benefits of PCV-VG along with an individualized OLA strategy in patients undergoing lung surgery with OLV.
The results of the present study are consistent with our expectation that using an OLA with individualized PEEP under PCV-VG mode can improve pulmonary gas exchange and lung mechanics as well as hemodynamic stability during OLV. Nevertheless, it is useful to note that during OLV, routinely measured airway pressure does not reflect the bronchial pressure, and the decrease in Ppeak under PCV mode is probably not clinically relevant when measured in the bronchus of the ventilated lung [26]. Therefore, we assumed that the difference in Ppeak in this study is meaningless due to the ventilation mode-related difference in end-inspiratory flow, as well as the resistance of the tracheal tube [27]. Unlike Ppeak, previous studies have demonstrated that Pmean closely reflects mean alveolar pressure and correlates with alveolar ventilation, arterial oxygenation, hemodynamic performance, and barotrauma under conditions of passive inflation [28, 29]. In this study, Pmean and Cdyn in the PCV+OLA and VCV+OLA groups were similar, and both were higher than those in the PCV and VCV groups. The reason may be related to the application of higher individualized PEEP. Indeed, others have shown that Pmean was significantly higher in the PCV+PEEP group compared with the VCV+zero PEEP and PCV+zero PEEP groups [24, 30]. Furthermore, it usually requires the application of extrinsic PEEP by increasing Pmean during OLV to prevent hypoventilation and atelectasis caused by low VT [31–33]. As a matter of fact, an abnormally high Pmean may incur the impairment of pulmonary circulation and hemodynamic stability [34]. However, there was no difference in hemodynamics among the four groups, probably because the higher Pmean in the PCV+OLA and VCV+OLA groups did not substantially affect hemodynamic stability during OLV. On the other hand, excessively high Pmean, especially mean alveolar pressure, increases pulmonary vascular resistance and makes blood flow towards the nonventilated lung, thus leading to the disturbance of Qs/Qt [29, 35, 36]. Nevertheless, the Qs/Qt in the PCV+OLA group was superior to that in the other groups during OLV, suggesting that acceptable Pmean recruits alveoli and tends to keep them properly open.
The higher PaO2/FiO2 ratio and lower VD/VT of the PCV+OLA and VCV+OLA groups during OLV may have been owing to the impact of the OLA and reasonable Pmean on oxygenation and the prevention of atelectasis. We assumed that the most suitable PEEP might more effectively maintain the advantages of an alveoli recruitment maneuver with regard to ventilation efficiency under the automatic adjustment of PCV-VG mode. Unlike the constant flow pattern observed in VCV, the pattern of inspiratory flow in PCV-VG mode is a deceleration type with high initial flow velocity, which results in compliant alveolar expansion and improves ventilation-perfusion matching [37]. Therefore, the PCV+OLA ventilation strategy integrated the merits of PCV-VG and OLA to improve both gas exchange and oxygenation accordingly. Another explanation was that FiO2 of 0.8 used during OLV could decrease the number of areas suffering from atelectasis and, consequently, lead to lowering Qs/Qt [35, 38]. However, some studies showed that compared with VCV, no benefits were found in PCV about the length of hospital stay and PaO2/FiO2 ratio [26, 39]. Consistent with the negative results of these studies, the results of respiratory mechanics and ventilation efficiency in the PCV group and the VCV group were similar; the reason may be that except for the different ventilator modes, the other treatment measures were the same in these two groups.
The release of pulmonary inflammatory mediators and their cascade reaction during OLV are the major mechanisms resulting in acute lung injury [16]. Neutrophil elastase participates in and initiates acute lung injury by injuring capillary endothelial cells and alveolar epithelial cells, as well as digesting and degrading the extracellular matrix and epithelial junctions [40]. A recent study showed that compared with VCV, PCV-VG could decrease the release of neutrophil elastase and minimize inflammatory reaction to reduce lung injury in patients undergoing OLV [22]. Fernandez-Bustamante et al. proposed that plasma neutrophil elastase might indicate atelectrauma in patients with short-term mechanical ventilation [41]. We found that the plasma concentration of neutrophil elastase was decreased considerably in the PCV+OLA group compared with the PCV, VCV, and VCV+OLA groups after OLV, demonstrating that the strategy of PCV-VG plus OLA had an important influence on alleviating ventilator-induced lung injury.
Unfortunately, except for the shortening of the duration of ICU stay, the prevalence of other postoperative endpoints did not decrease. Whether the strategy of PCV-VG plus OLA can impact upon postoperative duration of hospital stay, total duration of hospital stay, or the incidence of PPCs requires further study at multiple centers.
Our study had two main limitations. First, our study was not blinded, so biases are inevitable. Second, we only observed changes in heart rate and MAP. We intend to determine the effect of PCV-VG plus OLA during OLV on hemodynamic variables by measuring central venous pressure and cardiac output.
6. Conclusion
The ventilation strategy of PCV-VG combined with open-lung approach during OLV was associated with favorable effects upon intraoperative respiratory mechanics, oxygenation parameters, and the inflammatory reaction. This ventilation strategy may be a feasible alternative ventilation method in patients undergoing thoracic surgery.
Acknowledgments
The authors wish to thank all staff members in the Department of Anesthesiology, Hebei General Hospital, for their help in the study. The study was supported by the Key Research and Development Program of Hebei Province (19277714D).
Data Availability
The clinical data used to support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
No conflict of interest has to be disclosed.
Authors' Contributions
Jianli Li, MD, and Baogui Cai designed the study, conducted the study, analyzed the data, and approved the final manuscript. Dongdong Yu and Meinv Liu designed the study and wrote the manuscript. Xiaoqian Wu conducted the study. Junfang Rong, MD, analyzed data and wrote and edited the manuscript. Jianli Li and Baogui Cai contributed equally to this work and should be considered co-first authors.
References
- 1.Mahmoud K., Ammar A., Kasemy Z. Comparison between pressure-regulated volume-controlled and volume-controlled ventilation on oxygenation parameters, airway pressures, and immune modulation during thoracic surgery. Journal of Cardiothoracic and Vascular Anesthesia. 2017;31(5):1760–1766. doi: 10.1053/j.jvca.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 2.de la Gala F., Piñeiro P., Garutti I., et al. Systemic and alveolar inflammatory response in the dependent and nondependent lung in patients undergoing lung resection surgery: a prospective observational study. European Journal of Anaesthesiology. 2015;32(12):872–880. doi: 10.1097/EJA.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 3.Kaynar A. M., Houghton A. M., Lum E. H., Pitt B. R., Shapiro S. D. Neutrophil elastase is needed for neutrophil emigration into lungs in ventilator-induced lung injury. American Journal of Respiratory Cell and Molecular Biology. 2008;39(1):53–60. doi: 10.1165/rcmb.2007-0315OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park M., Ahn H. J., Kim J. A., et al. Driving pressure during thoracic surgery: a randomized clinical trial. Anesthesiology. 2019;130(3):385–393. doi: 10.1097/ALN.0000000000002600. [DOI] [PubMed] [Google Scholar]
- 5.Serpa Neto A., Hemmes S. N., Barbas C. S., et al. Protective versus conventional ventilation for surgery: a systematic review and individual patient data meta-analysis. Anesthesiology. 2015;123(1):66–78. doi: 10.1097/ALN.0000000000000706. [DOI] [PubMed] [Google Scholar]
- 6.Yang D., Grant M. C., Stone A., Wu C. L., Wick E. C. A meta-analysis of intraoperative ventilation strategies to prevent pulmonary complications: is low tidal volume alone sufficient to protect healthy lungs? Annals of Surgery. 2016;263(5):881–887. doi: 10.1097/SLA.0000000000001443. [DOI] [PubMed] [Google Scholar]
- 7.Ferrando C., Mugarra A., Gutierrez A., et al. Setting individualized positive end-expiratory pressure level with a positive end-expiratory pressure decrement trial after a recruitment maneuver improves oxygenation and lung mechanics during one-lung ventilation. Anesthesia and Analgesia. 2014;118(3):657–665. doi: 10.1213/ANE.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 8.Ferrando C., Suarez-Sipmann F., Tusman G., et al. Open lung approach versus standard protective strategies: effects on driving pressure and ventilatory efficiency during anesthesia - a pilot, randomized controlled trial. PLoS One. 2017;12(5) doi: 10.1371/journal.pone.0177399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lian M., Zhao X., Wang H., Chen L., Li S. Respiratory dynamics and dead space to tidal volume ratio of volume-controlled versus pressure-controlled ventilation during prolonged gynecological laparoscopic surgery. Surgical Endoscopy. 2017;31(9):3605–3613. doi: 10.1007/s00464-016-5392-x. [DOI] [PubMed] [Google Scholar]
- 10.Tan J., Song Z., Bian Q., Li P., Gu L. Effects of volume-controlled ventilation vs. pressure-controlled ventilation on respiratory function and inflammatory factors in patients undergoing video-assisted thoracoscopic radical resection of pulmonary carcinoma. Journal of Thoracic Disease. 2018;10(3):1483–1489. doi: 10.21037/jtd.2018.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bagchi A., Rudolph M. I., Ng P. Y., et al. The association of postoperative pulmonary complications in 109,360 patients with pressure-controlled or volume-controlled ventilation. Anaesthesia. 2017;72(11):1334–1343. doi: 10.1111/anae.14039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maeda Y., Fujino Y., Uchiyama A., Matsuura N., Mashimo T., Nishimura M. Effects of peak inspiratory flow on development of ventilator-induced lung injury in rabbits. Anesthesiology. 2004;101(3):722–728. doi: 10.1097/00000542-200409000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Lin F., Pan L., Qian W., Ge W., Dai H., Liang Y. Comparison of three ventilatory modes during one-lung ventilation in elderly patients. International Journal of Clinical and Experimental Medicine. 2015;8(6):9955–9960. [PMC free article] [PubMed] [Google Scholar]
- 14.Gad M., Gaballa K., Abdallah A., Abdelkhalek M., Zayed A., Nabil H. Pressure-controlled ventilation with volume guarantee compared to volume-controlled ventilation with equal ratio in obese patients undergoing laparoscopic hysterectomy. Anesthesia, Essays and Researches. 2019;13(2):347–353. doi: 10.4103/aer.AER_82_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amar D., Zhang H., Pedoto A., Desiderio D. P., Shi W., Tan K. S. Protective lung ventilation and morbidity after pulmonary resection: a propensity score-matched analysis. Anesthesia and Analgesia. 2017;125(1):190–199. doi: 10.1213/ANE.0000000000002151. [DOI] [PubMed] [Google Scholar]
- 16.Lohser J., Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesthesia and Analgesia. 2015;121(2):302–318. doi: 10.1213/ANE.0000000000000808. [DOI] [PubMed] [Google Scholar]
- 17.Sugasawa Y., Yamaguchi K., Kumakura S., et al. The effect of one-lung ventilation upon pulmonary inflammatory responses during lung resection. Journal of Anesthesia. 2011;25(2):170–177. doi: 10.1007/s00540-011-1100-0. [DOI] [PubMed] [Google Scholar]
- 18.Takenaka K., Ogawa E., Wada H., Hirata T. Systemic inflammatory response syndrome and surgical stress in thoracic surgery. Journal of Critical Care. 2006;21(1):48–53. doi: 10.1016/j.jcrc.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Güldner A., Kiss T., Serpa Neto A., et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123(3):692–713. doi: 10.1097/ALN.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 20.Pereira S. M., Tucci M. R., Morais C. C. A., et al. Individual positive end-expiratory pressure settings optimize intraoperative mechanical ventilation and reduce postoperative atelectasis. Anesthesiology. 2018;129(6):1070–1081. doi: 10.1097/ALN.0000000000002435. [DOI] [PubMed] [Google Scholar]
- 21.Ferrando C., Soro M., Unzueta C., et al. Individualised perioperative open-lung approach versus standard protective ventilation in abdominal surgery (iPROVE): a randomised controlled trial. The Lancet Respiratory Medicine. 2018;6(3):193–203. doi: 10.1016/S2213-2600(18)30024-9. [DOI] [PubMed] [Google Scholar]
- 22.Yao W., Yang M., Cheng Q., et al. Effect of pressure-controlled ventilation-volume guaranteed on one-lung ventilation in elderly patients undergoing thoracotomy. Medical Science Monitor. 2020;26 doi: 10.12659/MSM.921417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Byun S. H., Lee S. Y., Jung J. Y. Effects of small tidal volume and positive end-expiratory pressure on oxygenation in pressure-controlled ventilation-volume guaranteed mode during one-lung ventilation. Yeungnam University Journal of Medicine. 2018;35(2):165–170. doi: 10.12701/yujm.2018.35.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dion J. M., McKee C., Tobias J. D., et al. Ventilation during laparoscopic-assisted bariatric surgery: volume-controlled, pressure-controlled or volume-guaranteed pressure-regulated modes. International Journal of Clinical and Experimental Medicine. 2014;7(8):2242–2247. [PMC free article] [PubMed] [Google Scholar]
- 25.Song S. Y., Jung J. Y., Cho M. S., Kim J. H., Ryu T. H., Kim B. I. Volume-controlled versus pressure-controlled ventilation-volume guaranteed mode during one-lung ventilation. Korean Journal of Anesthesiology. 2014;67(4):258–263. doi: 10.4097/kjae.2014.67.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rozé H., Lafargue M., Batoz H., et al. Pressure-controlled ventilation and intrabronchial pressure during one-lung ventilation. British Journal of Anaesthesia. 2010;105(3):377–381. doi: 10.1093/bja/aeq130. [DOI] [PubMed] [Google Scholar]
- 27.Slinger P. D., Lesiuk L. Flow resistances of disposable double-lumen, single-lumen, and Univent tubes. Journal of Cardiothoracic and Vascular Anesthesia. 1998;12(2):142–144. doi: 10.1016/s1053-0770(98)90320-2. [DOI] [PubMed] [Google Scholar]
- 28.Bunnell A., Cheatham M. L. Airway pressures as surrogate estimates of intra-abdominal pressure. The American Surgeon. 2015;81(1):81–85. [PubMed] [Google Scholar]
- 29.Marini J. J., Ravenscraft S. A. Mean airway pressure: physiologic determinants and clinical importance--part 2: clinical implications. Critical Care Medicine. 1992;20(11):1604–1616. [PubMed] [Google Scholar]
- 30.Choi Y. S., Bae M. K., Kim S. H., Park J. E., Kim S. Y., Oh Y. J. Effects of alveolar recruitment and positive end-expiratory pressure on oxygenation during one-lung ventilation in the supine position. Yonsei Medical Journal. 2015;56(5):1421–1427. doi: 10.3349/ymj.2015.56.5.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gal T. J. Con: low tidal volumes are indicated during one-lung ventilation. Anesthesia and Analgesia. 2006;103(2):271–273. doi: 10.1213/01.ane.0000223678.64129.7c. [DOI] [PubMed] [Google Scholar]
- 32.Fanelli V., Ranieri M. V., Mancebo J., et al. Feasibility and safety of low-flow extracorporeal carbon dioxide removal to facilitate ultra-protective ventilation in patients with moderate acute respiratory distress syndrome. Critical Care. 2016;20(1) doi: 10.1186/s13054-016-1211-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gattinoni L. Ultra-protective ventilation and hypoxemia. Critical Care. 2016;20(1):p. 130. doi: 10.1186/s13054-016-1310-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Repessé X., Charron C., Vieillard-Baron A. Acute cor pulmonale in ARDS: rationale for protecting the right ventricle. Chest. 2015;147(1):259–265. doi: 10.1378/chest.14-0877. [DOI] [PubMed] [Google Scholar]
- 35.Sentürk M. New concepts of the management of one-lung ventilation. Current Opinion in Anaesthesiology. 2006;19(1):1–4. doi: 10.1097/01.aco.0000192778.17151.2c. [DOI] [PubMed] [Google Scholar]
- 36.Gallagher T. J., Banner M. J. Mean airway pressure as A determinant of oxygenation. Critical Care Medicine. 1980;8(4):p. 244. doi: 10.1097/00003246-198004000-00083. [DOI] [Google Scholar]
- 37.Prella M., Feihl F., Domenighetti G. Effects of short-term pressure-controlled ventilation on gas exchange, airway pressures, and gas distribution in patients with acute lung injury/ARDS: comparison with volume-controlled ventilation. Chest. 2002;122(4):1382–1388. doi: 10.1378/chest.122.4.1382. [DOI] [PubMed] [Google Scholar]
- 38.Edmark L., Kostova-Aherdan K., Enlund M., Hedenstierna G. Optimal oxygen concentration during induction of general anesthesia. Anesthesiology. 2003;98(1):28–33. doi: 10.1097/00000542-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Liu Z., Liu X., Huang Y., Zhao J. Intraoperative mechanical ventilation strategies in patients undergoing one-lung ventilation: a meta-analysis. Springerplus. 2016;5(1):p. 1251. doi: 10.1186/s40064-016-2867-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kodama T., Yukioka H., Kato T., Kato N., Hato F., Kitagawa S. Neutrophil elastase as a predicting factor for development of acute lung injury. Internal medicine. 2007;46(11):699–704. doi: 10.2169/internalmedicine.46.6182. [DOI] [PubMed] [Google Scholar]
- 41.Fernandez-Bustamante A., Klawitter J., Repine J. E., et al. Early effect of tidal volume on lung injury biomarkers in surgical patients with healthy lungs. Anesthesiology. 2014;121(3):469–481. doi: 10.1097/ALN.0000000000000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The clinical data used to support the findings of this study are available from the corresponding author upon reasonable request.


