Abstract
Background and Purpose:
The National Institutes of Health (NIH) StrokeNet provides a nationwide infrastructure to advance stroke research. Capitalizing on this unique opportunity, the NIH StrokeNet Training Core (NSTC) was established with the overarching goal of enhancing the professional development of a diverse spectrum of professionals who are embedded in the stroke clinical trials network of the NIH StrokeNet.
Methods:
This special report provides a descriptive account of the rationale, organization and activities of the NSTC since its inception in 2013. Current processes and their evolution over time for facilitating training of NIH StrokeNet trainees have been highlighted. Data collected for monitoring training are summarized. Outcomes data (publications and grants) collected by NSTC was supplemented by publicly available resources.
Results:
The NSTC comprises of cross-network faculty, trainees and education coordinators. It helps in development and monitoring of training programs and organizes educational and career development activities. Trainees are provided directed guidance towards their mandated research projects, including opportunities to present at the International Stroke Conference. The committee has focused on developing sustainable models of peer-to-peer interaction and cross-institutional mentorships. A total of 124 professionals (43.7% female, 10.5% underrepresented minorities) have completed training between 2013 and 2018, of whom 55% were clinical vascular neurologists. Of the total, 85% transitioned to a formal academic position and 95% were involved in stroke research post-training. Altogether, 1,659 indexed publications have been authored or co-authored by NIH StrokeNet Trainees, of which 58% were published during or after their training years. Based on data from 109 trainees, 33% had submitted 72 grant proposals as principal or co-principal investigators of which 22.2% proposals have been funded.
Conclusion:
NSTC has provided a foundation to foster nationwide training in stroke research. Our data demonstrate strong contribution of trainees towards academic scholarship. Continued innovation in educational methodologies is required to adapt to unique training opportunities such as the NIH StrokeNet.
Keywords: Stroke, Education, National Institutes of Health
Background
In fall of 2013, The National Institute of Neurological Diseases and Stroke (NINDS) established the National Institutes of Health (NIH) StrokeNet to enable coordinated planning, swift initiation, effective implementation, streamlined operationalization and centralized monitoring of stroke clinical trials evaluating prevention, treatment and recovery interventions.1 The National Coordinating Center (NCC) at the University of Cincinnati and the National Data Management Center (NDMC) at the Medical University of South Carolina function as central organizing institutions. Since its inception, the NIH StrokeNet has developed into a robust and expansive network comprised of twenty-nine academic regional coordinating centers (RCCs) across the United States, each with their respective clinical performance and satellite sites. As of April 2019, this network is comprised of over 500 hospitals. The NIH StrokeNet was chartered not only to conduct high quality collaborative stroke research, but training and ongoing education of physicians from various disciplines and a wide spectrum of healthcare professionals was also planned and incorporated as a tenet of the NIH StrokeNet. The NIH StrokeNet training was not envisioned to substitute or replace institutional professional research training programs or individual funding awards, but rather it is embedded within the overarching clinical trials infrastructure and is geared towards professional advancement of the selected trainees. The NIH StrokeNet award provides funding to ensure that trainees at individual RCCs can dedicate at least 50% protected time to effectively train and engage in stroke research. The NIH StrokeNet Training Core (NSTC) is a multidisciplinary committee that oversees the StrokeNet trainees and endavors to realize the NIH StrokeNet mission of training and mentoring future leaders in stroke research. The NSTC serves to fulfil this integral function by providing educational resources, rending direct feedback, fostering cross-institutional mentorships, organizing opportunities for peer-to-peer (P2P) interaction, and supervising training for the NIH StrokeNet trainees at RCCs nationwide. This special report provides an account of organization, processes, achievements and future directions of the NSTC.
Methods
Organizational Structure and Membership
The principal operations of the NSTC are directed and coordinated from the NIH StrokeNet NCC. However, the core committee includes cross-network representation of faculty, education coordinators, and current and past trainees. Other than the NCC staff and the Chair and Co-Chair, all members of the NSTC (including faculty) are rotated to provide an opportunity to multiple RCCs for contribution towards NSTC activities. Currently, NSTC is comprised of 14 members (6 faculty – including Chair and Co-Chair, 3 coordinators – including the main NSTC coordinator at NCC, 2 each of former and current trainees, and an NINDS project scientist). Each academic year, new trainees are invited to serve on the NSTC as trainee representatives. Trainee applications are reviewed by current NSTC members and final selection is based on applicants’ record of productivity, interest in academic medicine, and considerations of diversity in representation. All past and current members of the NSTC were invited to participate in drafting this special report.
Salient Activities and Resources
The overarching goal of the NSTC is two-fold; 1) to provide oversight for the RCC training programs and 2) to function as a resource for trainees and their mentors. A schematic representation of various activities undertaken by the NSTC over the course of a typical academic year to fulfil these goals is provided in Figure 1. A brief account of these activities and functions is described below.
Figure 1:
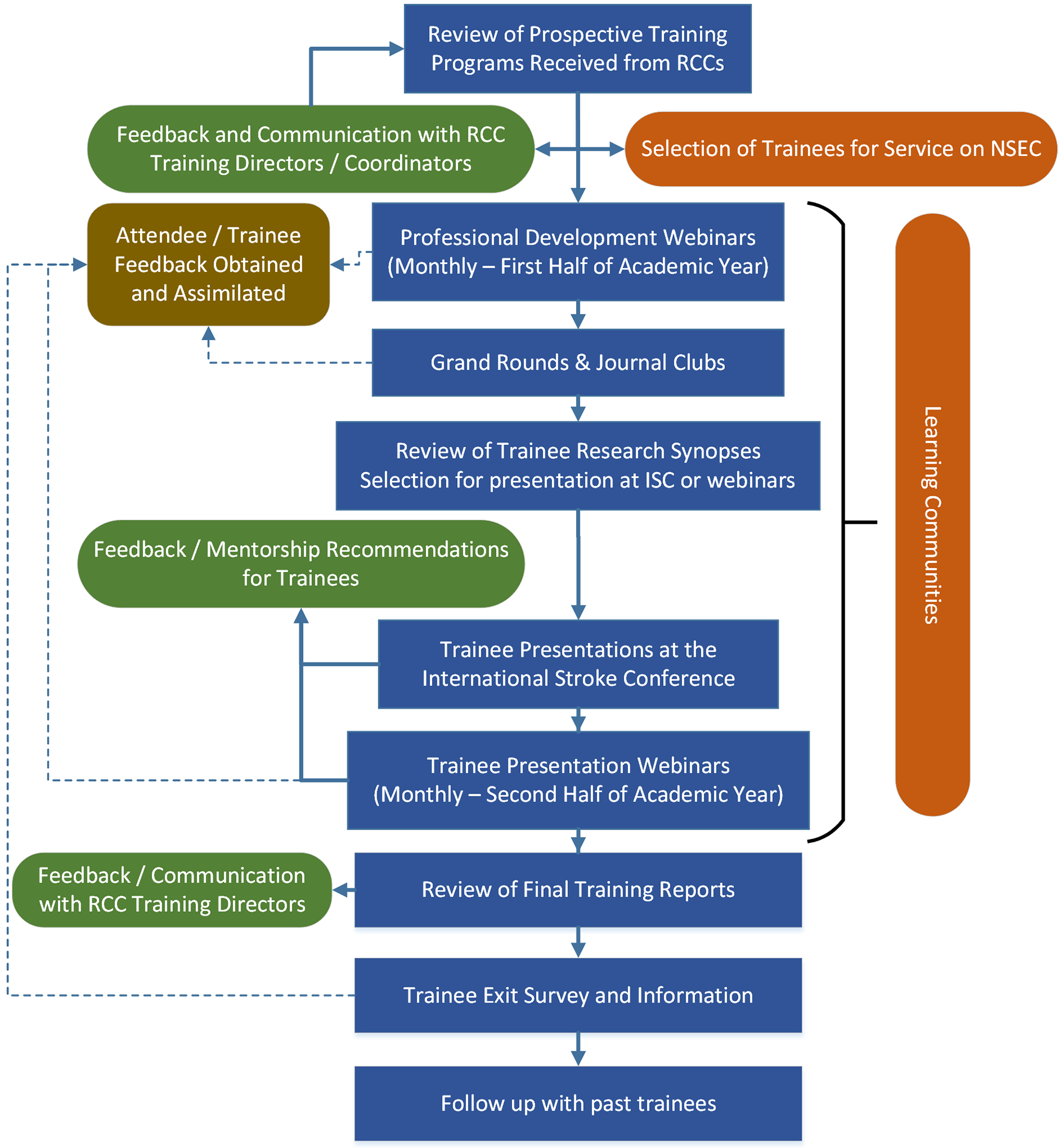
Schematic representation of the activities undertaken by the NIH StrokeNet Training Core (NSTC) on an annual process. The figure chronologically represents (starting from top) a typical academic year. Blue boxes are various activities of the NSTC, green and brown boxes are feedback and communication loops with RCCs and trainees. Activities undertaken as a part of learning health communities are highlighted in orange.
Training oversight:
At initiation of each academic year, RCCs submit individualized training programs for their respective trainees. These training programs are solicited in a structured format to objectively evaluate potentially heavy clinical workloads or obligations that might interfere with the trainees’ protected time to engage in stroke research and training. The trainees, with their mentors, are also required to develop an educational plan, a research focus, and specific milestones. Each training plan is independently reviewed by two NSTC members and further discussed in a full committee NSTC meeting, with clarifications sought from RCCs if required. Additional oversight is provided by review of the final trainee progress reports which detail the achievement of research milestones (abstracts, manuscripts, grants, other presentations, coursework, participation in clinical trials, attendance of StrokeNet webinars) throughout the training year. Data on training metrics are also summarily assimilated and reviewed by the NSTC. Finally, all trainees are strongly encouraged to complete a blinded exit survey with the objective of obtaining an unbiased assessment of their training year and candid recommendations for improvements to the training program. De-identified survey results are compiled and reviewed during a NSTC session and the findings weigh heavily in planning and program improvements for the subsequent year.
Learning Communities:
A primary goal of the NSTC is to provide a platform for peer-to-peer (P2P) interaction. Not only has the effectiveness of P2P interaction been demonstrated in various training settings,2, 3 lack of peer networking was also the most frequently cited weakness by StrokeNet trainees in the past. The NSTC has since piloted and monitored the effectiveness of various P2P platforms. Beginning in the 2017 – 2018 training cycle, the NSTC assembled ‘Learning Communities’ for the NIH StrokeNet trainees. At the beginning of the academic year, trainees are assigned to small groups based on similar research interests paired with a senior faculty mentor. The goal is to provide networking opportunities with colleagues, and mentorship in research and career development. The NSTC continually monitors and annually evaluates the performance of these Learning Communities. One successful example of a Learning Community during its first academic year entailed monthly video conference call sessions that included career development topics requested by trainees, guest lecturers, and opportunities to practice and receive feedback on research presentations.
StrokeNet Grand Rounds:
The monthly NIH StrokeNet Grand Rounds comprise stroke experts presenting topics that are deemed useful for not only the trainees but also appeal to a broader audience of stroke researchers. The sessions are presented in webinar format and moderated by a member of the NSTC. Trainees are either required to attend live webinars or view recordings of these webinars which are available on the NIH StrokeNet website. Potential topics and speakers to be included in this series are solicited from all RCCs at the beginning of the academic year. Topics are thematically organized to avoid duplication or replication and a final list is assembled by the NSTC, with an attempt to create diversity in speakers and themes presented. Overall, this series has been successful in generating enlightening post-presentation discussions and has received increasingly stronger positive feedback from the trainees over the years (Figure 2). All NSTC webinars are recorded, and viewable on demand on the NIH StrokeNet website (https://www.nihstrokenet.org/education).
Figure 2:
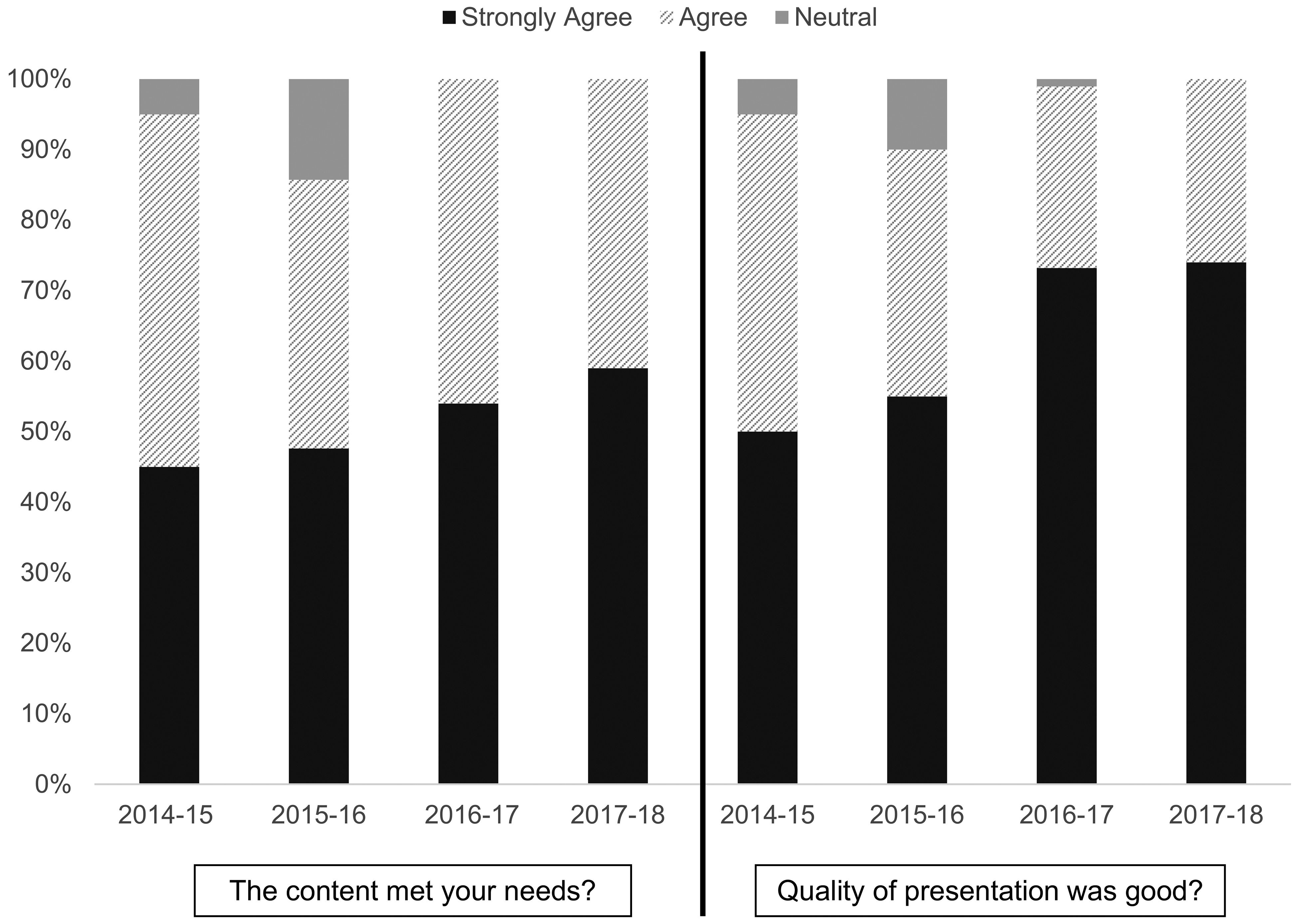
Proportions of trainee / attendee responses across categories of agreement regarding content and quality of NIH StrokeNet Training Core moderated grand rounds for last four annual training cycles.
Professional Development Webinars:
Professional development webinars are delivered by NSTC core and other network faculty in the first half of the academic year. Topics include how to prepare your CV, how to present data, grant writing, and study budgets. Although primarily focused to provide fundamental knowledge to early career trainees, the topics covered in this series have continually received positive feedback from all levels of attendees (Figure 3). Topics and speakers for this series are decided internally by the NSTC, largely based on attendee feedback from prior years or any new suggestions made by NSTC members.
Figure 3:
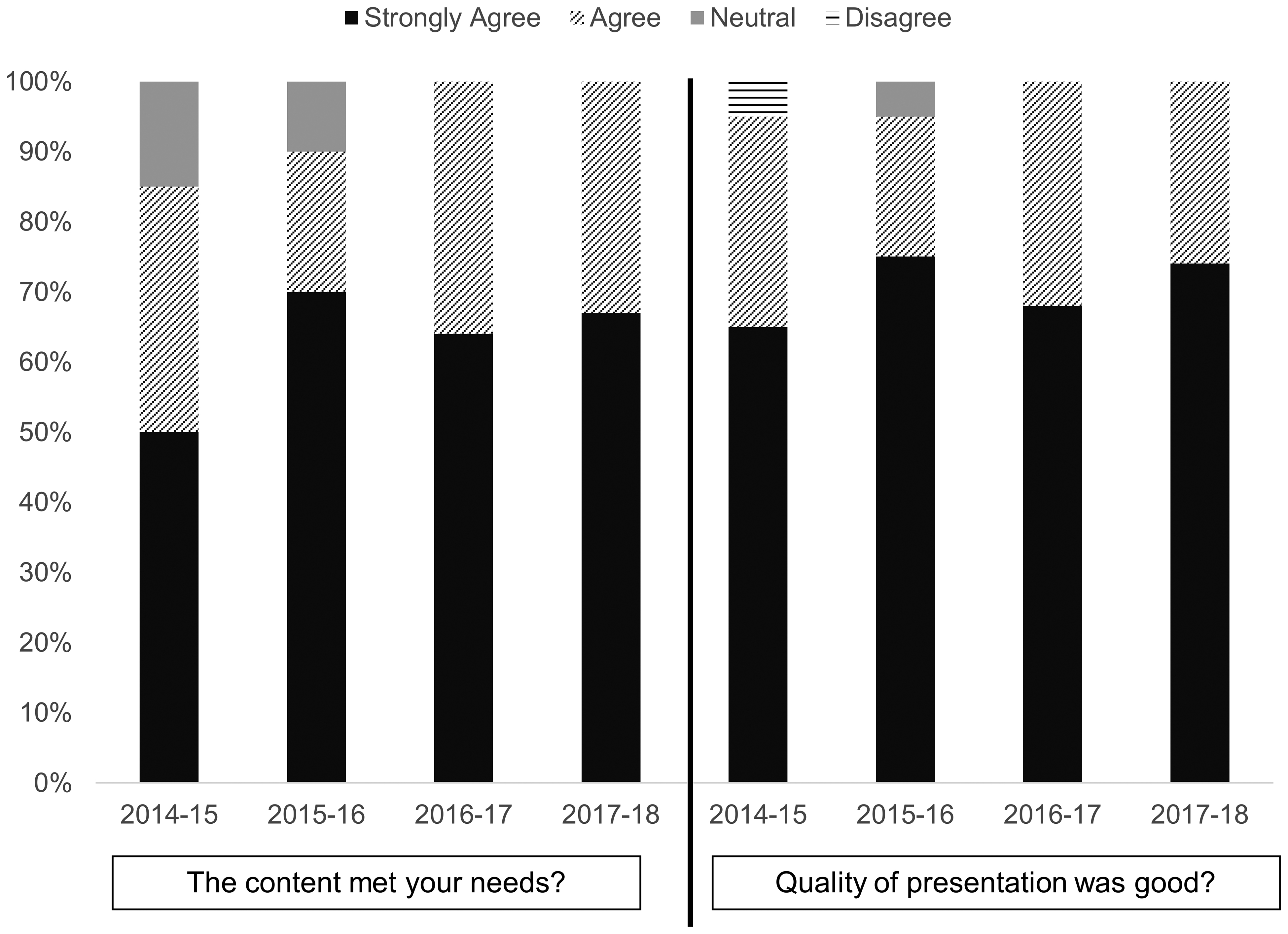
Proportions of trainee / attendee responses across four categories of agreement regarding content and quality of NIH StrokeNet Training Core moderated professional development webinars for last four annual training cycles.
Basic Science Journal Club Webinars:
More recently, the NSTC has initiated basic science journal clubs as biannual webinars led by investigators with an ongoing NIH StrokeNet trial. The concept is to help the trainees develop critical thinking required for linkage between basic and clinical science by providing practical examples of translational research that underlies a StrokeNet clinical trial. To date, three webinars have been delivered highlighting the basic science underlying the ARCADIA and the CREST-H and MOST trials of the NIH StrokeNet.4–6 The NSTC continues to evaluate the impact and feasibility of this series.
Research Presentations:
During the academic year, NIH StrokeNet trainees are required to develop and execute a primary research project. The projects are identified at the beginning of the academic year and trainees are provided opportunities to present their research during training. The NSTC has organized trainee research presentations during the annual International Stroke Conference (ISC). Project synopses or results are solicited from trainees towards the end of the calendar year (mid-academic year) and are independently scored by two NSTC members using methods analogous to the NIH review. During a full committee NSTC session, research projects are reviewed and network-wide faculty members are identified who can provide feedback and mentorship to the trainees based on scientific interest areas. Six to nine highest scoring projects are selected for an oral presentation at the NIH StrokeNet meeting before the ISC, and identified faculty mentors are requested to attend. The remaining research presentations are delivered via webinar throughout the second half of the academic year with suggested mentors in attendance. These presentations have been consistently rated as a high value activity by the trainees. The NSTC has also made concerted efforts in pairing trainees with cross-network mentors. The in-person presentations at the ISC have been engaging, generating excellent discussion and feedback not only by assigned mentors but also by other faculty and trainees in attendance. The overarching vision of the NSTC is not only to improve the quality of training for the NIH StrokeNet trainees, but also to link a diverse group of mid-career mentors at several excellent academic institutions across the nation with trainees at other centers who are likely to be future leaders in stroke research.
Results
Summary Trainee Data:
Starting in academic year 2013 – 2014 through the time of this publication, a total of 124 trainees (43.7% females, 10.5% underrepresented minority) across 29 nationwide RCCs have either completed or are currently undergoing training via the NIH StrokeNet mechanism. Of these, 6 trainees have completed two-year training whereas the rest underwent the conventional one-year training cycle. At the initiation of training, the primary degree for the majority (81%) of the trainees was a clinical doctorate (MD/DO), whereas the rest were either PhDs (10%) or had obtained other postgraduate/doctoral degrees in pharmacy, physical therapy, nursing or public health (9%). Approximately 55% of NIH StrokeNet trainees have either been clinical fellows or junior faculty specializing in vascular neurology/stroke, whereas the remaining encompass a wide range of clinical specialties such as neurosurgery, neurocritical care, neuroradiology, emergency medicine, physical medicine and neuro-rehabilitation, pharmacy and biomedical engineering.
Post Training Research Engagement:
Among the trainees who have completed their training, 87% have advanced to a formal academic position and overall 95% stated that their new position will involve some aspect of stroke research. Furthermore, in their new positions, 80% of trainees affirmed that they would be enrolling patients into clinical trials and 68% indicated that they planned on submitting proposals for funding. At the time of exit, the median (interquartile range, IQR) percent effort that the trainees anticipated dedicating to stroke research was 30% (12.5% – 70%).
Trainee Feedback and Survey:
Trainees’ satisfaction and engagement with various aspects of the training program was also assessed upon training completion using a five-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree). Metrics included the overall experience, content suitability, quality of presentations, opportunity to share ideas and network with peers, communication received from NSTC, usefulness of NIH StrokeNet/NSTC website, and interactions with mentors. Throughout the full course of the training program, near-complete (> 95%) data are obtained for both the exit information and the trainee feedback. Greater than 80% trainees have either agreed or strongly agreed with usefulness and applicability of all aspects of NSTC directed training over the course of the last 5 years. Figures 2 and 3 represent the content suitability and quality of presentation feedback respectively for NIH StrokeNet grand rounds and professional development webinars across the years of training.
In rare cases where trainees identified issues within their program, the NSTC has worked collectively to specifically address these concerns.
Trainee Manuscripts and Publications:
We conducted a systematic search for all publications authored or co-authored by the NIH StrokeNet trainees using online PubMed search tool PubMed Pub Reminer (https://hgserver2.amc.nl/cgi-bin/miner/miner2.cgi) version 1.31. Search results were cross referenced for specialty and subject matter to avoid false positives. Moreover, trainees’ current publicly available institutional profiles were also cross referenced to increase specificity. Trainees for whom the publication data was either not accessible or not specific enough were contacted in person to provide current updates on their publication metrics. Complete data are available for 98% of the trainees and are updated as of Feb 28, 2019. The total number of PubMed indexed publications authored or co-authored by the NIH StrokeNet trainee cohort is 1,659. Of these, 973 (58%) have been published after the start of NIH StrokeNet training. The NIH StrokeNet trainees are either the first or the last authors on 45% of 973 NIH StrokeNet associated publications. The median (IQR) number of total publications by the NIH StrokeNet trainees is 9 (4 – 19), whereas the median (IQR) number of publications published during or after the training period is 5 (2 – 11). The trainees published a median (IQR) of 1.5 (0.67 – 3.5) manuscripts per year either during or after their StrokeNet training. The distribution of publications per year is skewed upward by the top 10 percentile of NIH StrokeNet trainees (n = 16) who have averaged 8.9 publications per year since the start of their NIH StrokeNet training.
Trainee Grants and Funding Proposals:
Based on data from four training cycles (Training years 2014–2015 through 2017–2018) we assimilated grant submission metrics for a total of 109 NIH StrokeNet trainees. We only included proposals for which the trainees were either the principal investigators (PI) or co-PI. Proposals for which trainees collaborated as co-investigators were not included. Of the 109 trainees during the included training years, 36 (33%) had submitted a total of 72 funding proposals either as PI or a co-PI. At the time of data collection, 37 (51.4%) of these 72 proposals were under review, whereas 16 (22.2%) had been funded. The targeted mechanisms of funding include federal training and research grants, state government grants, foundation and industry grants, local institutional grants, professional organizations such as the American Heart and Stroke Association and the American Academy of Neurology, and other mechanisms such as health service organizations. The cumulative proportions of submitted, under-review and funded grants for each funding mechanism are shown in Figure 4.
Figure 4:
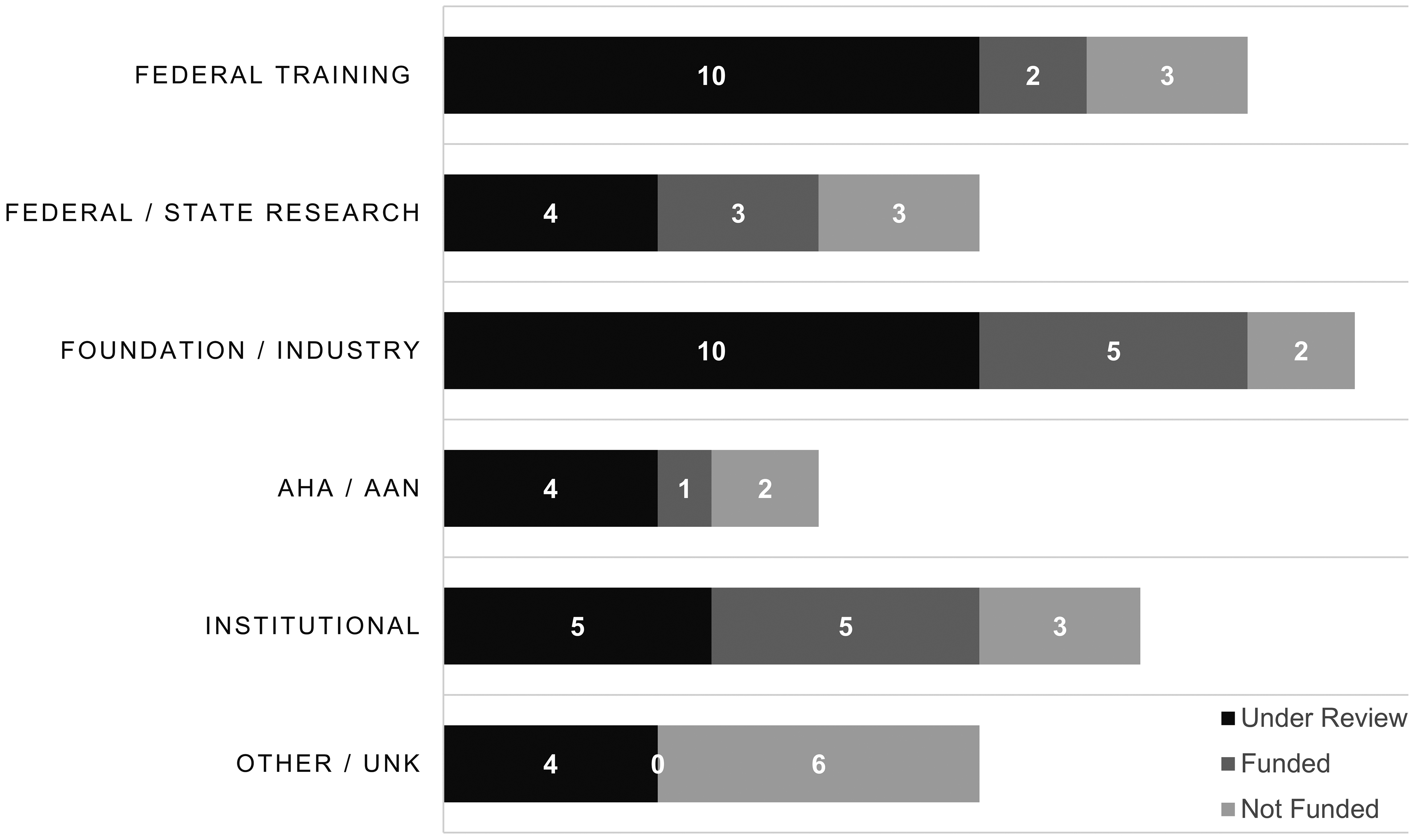
Number of grant proposals submitted by the NIH StrokeNet Trainees categorized as ‘not funded’, ‘under review’ and ‘funded’ across various funding mechanisms during past four training cycles. Representation of data on total 109 NIH StrokeNet trainees. AHA: American Heart Association, AAN: American Academy of Neurology, UNK: Unknown
Conclusion
Overall, the StrokeNet research training fellowship provides valuable opportunities for education and training in stroke research as well as career development. More than 95% of former trainees stated that they will continue to be involved in some aspect of stroke research including 80% of trainees who plan to enroll patients into clinical trials and 68% who intend to submit research proposals for funding. Our data also demonstrate a strong contribution of the trainees towards academic scholarship in terms of publications and submissions for funding opportunities. The NSTC has provided a foundational infrastructure to foster burgeoning stroke researchers by means of mentorship, educational curricula and funding. The NSTC leadership and members have maintained an adaptive learning model in design, implementation and monitoring of the training program whereby several programmatic aspects have been tested, modified and retested in the process. This was particularly important because of the novel nature of this training paradigm. We believe that this has significantly contributed to the growth and thoughtfulness of the NSTC. We would like to highlight that data presented in this report were not generated from an experimental / interventional design and there are no comparable controls. However, the training component was rigorously evaluated at the NIH along with the overall renewal application of the StrokeNet. Furthermore, it is also possible that the trainees selected at various RCCs were already motivated to engage in stroke research. The attributability of NIH StrokeNet training to the productivity metrics should therefore be interpreted with caution. The NSTC will continue to seek opportunities to promote diversity and improve the quality of its well-established educational program to foster the development of future stroke researchers.
Acknowledgements:
We acknowledge the role of all training directors at regional coordinating centers (RCC) of the NIH StrokeNet. We are also thankful for all past and present NIH StrokeNet Training Core committee members and all past and present trainees. We would specifically like to acknowledge efforts of Jeanne Sester, the NIH StrokeNet Training Core Coordinator at the University of Cincinnati for her untiring efforts and contributions to the core. We would like to thank Katie Alex and Maria Attia at the University of Texas Health Science Center Houston for helping with data abstraction for this special report.
Funding: NIH StrokeNet Grant 5U01NS086872-07
Footnotes
Conflicts / Roles: All authors (other than JRM) are either past or present members of the NIH StrokeNet Training Committee (NSTC). DK and RSM serve as the chair and co-chair of the NSTC. FSV and CBS are prior trainees who currently serve on the NSTC. Manuscript was written by FSV and CBS. Data were assimilated and analyzed by FSV and JRM. Manuscript concept and design was developed by FSV and DK. All other authors provided edits and feedback on the manuscript content and have approved the submission of the manuscript. LCJ reports receiving professional fees as medical expert for a legal case, not related to this work. RJR received additional institutional support related to this manuscript and received professional fees by Hippo Education not related to this work.
References
- 1.Broderick JP, Palesch YY, Janis LS, National Institutes of Health StrokeNet I. The national institutes of health strokenet: A user’s guide. Stroke. 2016;47:301–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glynn LG, MacFarlane A, Kelly M, Cantillon P, Murphy AW. Helping each other to learn--a process evaluation of peer assisted learning. BMC medical education. 2006;6:18–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.House JB, Choe CH, Wourman HL, Berg KM, Fischer JP, Santen SA. Efficient and effective use of peer teaching for medical student simulation. West J Emerg Med. 2017;18:137–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamel H, Longstreth WT Jr., Tirschwell DL, Kronmal RA, Broderick JP, Palesch YY, et al. The atrial cardiopathy and antithrombotic drugs in prevention after cryptogenic stroke randomized trial: Rationale and methods. International journal of stroke : official journal of the International Stroke Society. 2019;14:207–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marshall RS, Lazar RM, Liebeskind DS, Connolly ES, Howard G, Lal BK, et al. Carotid revascularization and medical management for asymptomatic carotid stenosis–hemodynamics (crest-h): Study design and rationale. International Journal of Stroke. 2018;13:985–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Multi-arm optimization of stroke thrombolysis trial. (2019). Nihstrokenet.org. Retrieved 31 October 2016, from https://www.nihstrokenet.org/most/most


