To rapidly communicate information on the global clinical effort against Covid-19, the Journal has initiated a series of case reports that offer important teaching points or novel findings. The case reports should be viewed as observations rather than as recommendations for evaluation or treatment. In the interest of timeliness, these reports are evaluated by in-house editors, with peer review reserved for key points as needed.
A 3-week-old boy presented with a 2-day history of nasal congestion, tachypnea, and reduced feeding. He was born at 36 weeks of gestation to a 21-year-old woman (gravida 3, para 1) who had received antenatal treatment for carriage of group B streptococci. He had previously received a 48-hour course of antibiotics for suspected neonatal sepsis because of a fever (temperature, 38.5°C), but the workup for sepsis was negative, and he was discharged home.
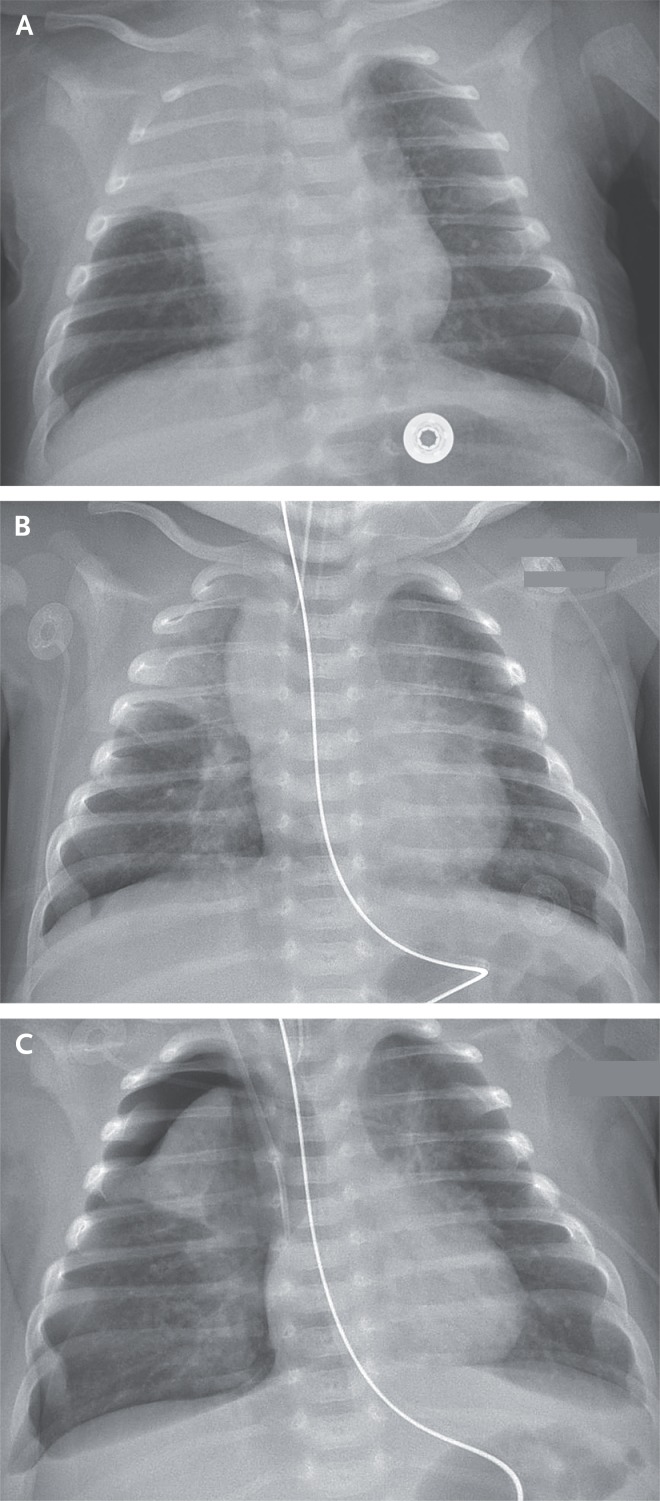
On admission of the patient to the emergency department, the temperature was 36.1°C, the pulse 166 beats per minute, the blood pressure 89/63 mm Hg, the respiratory rate 40 breaths per minute, and the oxygen saturation 87% while the patient was breathing ambient air. Chest radiography showed bilateral linear opacities and consolidation in the right upper lobe (Figure 1A). Oxygen and empirical antibiotics (ampicillin and gentamicin) were administered, and the patient was transferred to a pediatric hospital.
Figure 1. Chest Radiographs.
On admission, a radiograph showed bilateral linear opacities and consolidation in the right upper lobe (Panel A). After intubation, a radiograph showed bilateral infiltrates and partial collapse of the right upper lobe (Panel B). On day 2 after admission, a radiograph showed pneumothorax on the right side (Panel C).
On transfer, the patient had hypotension, tachycardia, hypothermia, and tachypnea. Droplet and contact precautions were initiated, and he was transferred to a negative-pressure room in the pediatric intensive care unit (PICU), where he was intubated and received crystalloid solution at a dose of 60 ml per kilogram of body weight, followed by vasopressors. Nasal swabs were obtained for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) testing and a respiratory viral panel. Chest radiography performed after intubation showed bilateral infiltrates and partial collapse of the right upper lobe (Figure 1B). Transthoracic echocardiography showed normal cardiac anatomy and function. The white-cell count was 4000 per cubic millimeter with 55% lymphocytes; levels of inflammatory markers were elevated (full laboratory results are provided in the Supplementary Appendix, available with the full text of this case at NEJM.org).
Mechanical ventilation was initiated with a positive end-expiratory pressure of 7 cm of water, a fraction of inspired oxygen of 0.6, and a mean airway pressure of 22 cm of water, resulting in a partial pressure of arterial oxygen of 49 mm Hg and a partial pressure of arterial carbon dioxide of 80 mm Hg. Treatment was switched to vancomycin, cefepime, and ampicillin and was discontinued after 48 hours when the cultures were negative. Hydroxychloroquine and azithromycin were initiated for presumed Covid-19.
On day 2 after admission, the hypotension resolved. A pneumothorax that developed on the right side (Figure 1C) was successfully treated by tube thoracostomy. The patient was extubated on day 5 and was transferred out of the PICU. The results of reverse-transcriptase–polymerase-chain-reaction testing to detect SARS-CoV-2 on admission were positive on day 7; he completed the 5-day course of hydroxychloroquine and azithromycin. The patient was discharged on day 9 without supplemental oxygen. One of eight household contacts of the patient, a 49-year-old woman, was symptomatic; however, none of the contacts were tested for SARS-CoV-2.
Although children are less likely than adults to have severe Covid-19, this case illustrates that it can occur and can be successfully managed with standard PICU protocols.1 The one exception to the standard protocol was that noninvasive mechanical ventilation was not attempted, since Covid-19 was suspected.
Supplementary Appendix
Disclosure Forms
This case was published on April 22, 2020, at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this case at NEJM.org.
Reference
- 1.Lu X, Zhang L, Du H, et al. SARS-CoV-2 infection in children. N Engl J Med. DOI: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.