Several papers recently published in ‘Brain, Behavior, and Immunity’ have addressed the mental health consequences of using psychoneuroimmunity to slow the spread of COVID-19 (Kim and Su, 2020, Tan et al., 2020). Tan et al. (2020) showed that non-social psychoneuroimmunity measures, such as handwashing, can play a protective psychological function. However, social measures for mitigating COVID transmission, including social distancing, travel bans, and sheltering-in-place, have not been examined. Curbing socially facilitated transmission of COVID is the most effective strategy for reducing rates of infection. However, as noted by Kim and Su (2020), it also introduces considerable challenges to daily functioning and as such, may ultimately compromise psychosocial sources of immunity. It is vital for health professionals, policy makers, and researchers to recognize whether this tradeoff exists: does prevention through social isolation reduce immunity by adding to the mental health burden of the pandemic?
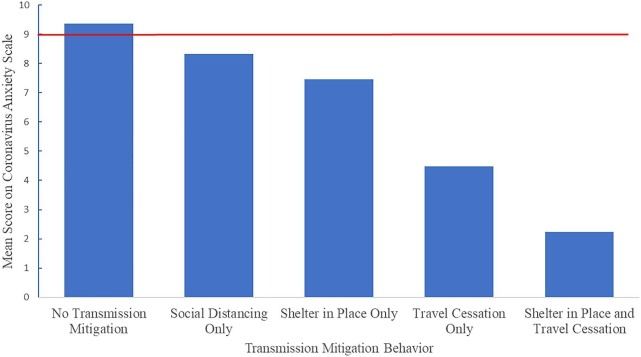
We addressed this question by examining how social isolation behaviors related to clinically dysfunctional coronavirus anxiety (Lee, Jobe, & Mathis, 2020), which is a key mental health outcome established by a previous publication in ‘Brain, Behavior, and Immunity’ (Lee, 2020). An online survey was collected April 14–15, 2020 from 408 MTurk workers (233 males, 174 females, 1 other gender, median age: 34 years, range: 21–65). Mean coronavirus anxiety scores did not reach the dysfunctional range (M < 9) among those who engaged in social isolation to mitigate coronavirus transmission, but did reach the dysfunctional range (M ≥ 9) among those who did not engage in any transmission-mitigating behaviors (see Fig. 1 ). In fact, coronavirus anxiety progressively decreased as social isolation measures intensified, such that coronavirus anxiety was significantly lower among those who both sheltered-in-place and ceased non-essential travel (F(5, 304) = 32.90, p < .01; M = 2.24, SD = 3.10) than among those who did not engage any transmission-mitigation (M = 9.36, SD = 5.59), those who social distanced only (M = 8.32, SD = 5.19) and those who sheltered-in-place only (M = 7.46, SD = 5.98). Further, a logistic regression demonstrated that sheltering-in-place [odds ratio 0.20, 95% CI 0.09–0.44] and cessation of long-distance travel [odds ratio 0.06, 95% CI 0.03–0.13] were significantly, negatively associated with dysfunctional coronavirus anxiety, while sociodemographic variables (age, gender, race) and pandemic stressors (increased cost of living, employment loss, decreased income, loss of childcare) were not. This model explained 50% (Nagelkerke R2) of the variance in dysfunctional coronavirus anxiety.
Fig. 1.
Mean scores on the Coronavirus Anxiety Scale (CAS) for participants based on their approach to engaging in coronavirus transmission-mitigation behavior. The red line indicates the cut-off for dysfunctional coronavirus anxiety on the CAS. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
We then examined the mechanism by which preventative social isolation protected against dysfunctional coronavirus anxiety. In line with previous research on the impact of stressful experiences (Milman et al., 2019), it appears that engaging in social prevention measures reduces coronavirus anxiety by minimizing the degree to which the pandemic violates beliefs regarding the controllable and predictable nature of the world. Indeed, those who sheltered-in-place and ceased long-distance travel reported significantly less belief violation (F(5, 304) = 18.33, p < .01; M = 2.52, SD = 1.06) than those who did not engage in preventative measures (M = 3.71, SD = 1.26).
These results demonstrate that social isolation strategies do not add to the mental health burden of the pandemic, and thereby are not likely to compromise immune functioning. In fact, social isolation strategies decreased the likelihood of clinically dysfunctional coronavirus anxiety, even in the context of pandemic stressors such as employment loss, decreased income, loss of childcare, and increased cost of living. It appears that by offering opportunities to participate in the effort to curb COVID transmission, social isolation policies also bolster sense of control and predictability which is otherwise diminished by the pandemic. Therefore, mental health practitioners would be well-advised to encourage social measures of transmission-mitigation as a means of tempering coronavirus anxiety. Addressing the considerable pressure to ease social isolation policies, these outcomes imply that staying the course will minimize both the physical and psychological consequences of the pandemic.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbi.2020.05.007.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Kim S.-W., Su K.-P. Using psychoneuroimmunity against COVID-19. Brain, Behav., Immun. 2020 doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain, Behav., Immun. 2020 doi: 10.1016/j.bbi.2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A., Jobe M.C., Mathis A.A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 2020 doi: 10.1017/S003329172000121X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman E., Neimeyer R.A., Fitzpatrick M., MacKinnon C.J., Muis K.R., Cohen S.R. Prolonged grief and the disruption of meaning: establishing a mediation model. J. Counseling Psychol. 2019;66(6):714. doi: 10.1037/cou0000370. [DOI] [PubMed] [Google Scholar]
- Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese Workforce. Brain, Behav., Immun. 2020 doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.