Abstract
Background
The American Academy of Pediatrics 2015 policy statement on telehealth proposed that telehealth could increase access to high-quality pediatric care and that pediatricians should work to reduce barriers to telehealth for their patients. However, little is known about pediatricians’ experiences with and attitudes toward telehealth.
Methods
Data from a nationally representative survey of American Academy of Pediatrics postresidency US member pediatricians in 2016, restricted to respondents providing direct patient care (n = 744; response rate = 48.7%). Survey collected information on experience with telehealth in the previous 12 months, perceived barriers to telehealth incorporation, and conditions under which nonusers would consider using telehealth. In addition to descriptive statistics, we used multivariable logistic regression to examine characteristics associated with any telehealth experience in the past 12 months.
Results
Fifteen percent of pediatricians reported any telehealth use in the 12 months prior to the survey. The most commonly reported barriers to telehealth adoption were insufficient payment and billing issues. Multivariable regression models indicated that pediatricians in rural areas, the West, and subspecialists were most likely to report telehealth use, and identifying barriers was negatively associated with telehealth use. Among nonusers, over half indicated they would consider adopting telehealth if they were paid for the visits.
Conclusion
Telehealth is considered an important health care delivery mechanism, but only 15% of pediatricians in 2016 reported having used telehealth. Reducing barriers will be instrumental in promoting future telehealth adoption. Many barriers have been reduced during the response to COVID-19, and the impact of these policy changes will need further study.
Keywords: pediatrician survey, telehealth
What's New.
In 2016, 15% of pediatricians reported having used telehealth in the past year, with pediatricians in rural areas and the West being most likely. The most reported barriers to telehealth adoption were insufficient payment and inability to bill for services.
Alt-text: Unlabelled box
Telehealth is broadly defined as “the use of electronic information and communications technologies to provide and support health care when distance separates participants,”1 where the “technologies include videoconferencing, the internet, store-and-forward imaging, streaming media, and terrestrial and wireless communications.”2 Physician access to telehealth had increased in the years prior to the outbreak of COVID-19 in March 2020, and the growth of telehealth was largely attributed to factors such as rapid advancements in technology and transformations in the organization and delivery of health care.3, 4, 5 Nearly two thirds of hospitals reported having a computerized telehealth system in 2016, up from 55% only 2 years earlier, and the American Telemedicine Association estimated that around 15 million patients received some care via telehealth annually.6, 7, 8
The growing availability of telehealth has brought the potential to increase patient access to care, improve health outcomes, and reduce costs.4 , 9, 10, 11 The potential for telehealth to expand patient access to medical care is strongest in rural regions or other areas that face provider shortages.5 , 12 For pediatricians, there are a broad range of possible applications of telehealth including quality control, education, practice, consultation, and research.13 Correspondingly, the American Academy of Pediatrics (AAP), in its 2015 policy statement on telehealth, proposed that telehealth could increase access to high-quality pediatric care and recommended that pediatricians work to reduce barriers to providing telehealth to their patients.12
Even as the infrastructure and technology required to provide patient care via telehealth has expanded in recent years, only a few studies have provided national estimates of the prevalence of telehealth use among physicians. Estimates from these available studies indicate that telehealth usage rates among physicians remained low. Data from the 2016 Physician Practice Benchmark Survey of the American Medical Association estimated that 15% of all physicians worked in practices that used telemedicine for some kind of patient interaction, and that percentage was estimated at 12% for pediatricians; overall, this survey found that physicians in solo practices were least likely to report telehealth use relative to those who reported working in group practices or as hospital employees.14 Similarly, a 2014 survey by the American Academy of Family Physicians found that 15% of family physician respondents reported using telehealth services in the past 12 months, and barriers to using telehealth included lack of training, lack of reimbursement, cost of equipment, and potential liability issues.15 Another study measuring barriers to telehealth adoption in pediatrics identified reimbursement as the greatest barrier, followed by time investment, provider interest, and state regulations.16
This manuscript was written prior to the global outbreak of COVID-19, which has rapidly and dramatically altered the landscape for use of telehealth in the United States.17 With the emergence of the COVID-19 pandemic, there has been a quick rise in telehealth use among physicians, and forecasts for the expected number of telehealth visits in 2020 were revised sharply upwards.18, 19, 20, 21 A March 2020 survey of primary care providers found that while physicians were using more telehealth and that patients were accepting of telehealth visits, concerns remained regarding payment for these services.22 The societal and regulatory changes that have led to a massive surge in telehealth use are potentially short-lived, although it is also possible that the response to the pandemic will permanently alter how health care is delivered in the United States going forward.
In 2016, the AAP surveyed its members to better understand pediatricians’ telehealth experiences, and the resulting research serves as a valuable resource on the state of telehealth in pediatrics prior to the COVID-19 pandemic, as our state and federal legislators, health care leaders, and other stakeholders determine how best to adapt to the changes to the health care system brought on by COVID-19. Analyzing the 2016 survey data, this research addressed the following questions:
-
1.
What percent of pediatricians report having used telehealth in the past 12 months?
-
2.
What are the perceived barriers to incorporating telehealth into pediatric practice?
-
3.
What characteristics are associated with using telehealth?
-
4.
Among nonusers, under what types of conditions would they consider using telehealth?
Methods
Data
This analysis used data from the Periodic Survey, a nationally representative survey of randomly selected, nonretired US members of the AAP. The 2016 survey was administered to 1614 postresidency respondents. We sent up to 7 mailed surveys and 2 emails (with a link to complete the survey online) to nonrespondents between March and August of 2016. The final survey response rate was 49% (786/1614), and a nonresponse bias analysis indicated that respondents and nonrespondents did not differ with respect to age, gender, or geographic region. We restricted the analytic sample to pediatricians that reported providing direct patient care, yielding a final analytic sample of 744 respondents. Pairwise deletion was used in the descriptive analyses, and listwise deletion was used for the multivariable regression models. The AAP Institutional Review Board approved the survey.
Measures
The 2016 Periodic Survey from the AAP was developed through a collaboration between AAP staff and pediatrician subject matter experts, and the survey collected respondent demographic and practice characteristics and detailed responses regarding experience with and views about telehealth. In the survey, telehealth was defined for respondents as “the exchange of medical information from one location to another via electronic communications, i.e., providing care using real-time interactive video visits, referral consultations using live interactive video, and/or shared diagnostic images, vital signs, video clips or patient data to improve a patient's health” (simple phone-to-phone exchange was not included in the survey's definition of telehealth). To capture telehealth usage, the survey asked respondents, “During the past 12 months have you A) used telehealth or B) referred any of your patients for a telehealth consult?” (response options for both items A and B included “yes” and “no”). We combined these 2 utilization measures into one variable that is coded “1” if the respondent reported any telehealth in the past 12 months, and “0” otherwise; this “any telehealth” variable is our primary outcome measure and the dependent variable in our multivariable logistic regression analysis.
We also examined reported barriers to telehealth adoption. The survey asked, “How much of a barrier are each of the following to incorporating telehealth in your practice?,” and response options were included on a 3-point Likert scale: “not a barrier,” “a minor barrier,” and “a major barrier.” The listed barriers included insufficient payment, inability to bill for services, cost to purchase/maintain equipment/services, lack of information on quality of vendors/services, lack of information about subspecialists using telehealth, lack of support for troubleshooting, insufficient electronic infrastructure, lack of adequate training, lack of usefulness, lack of confidence in telehealth diagnoses, and patient reluctance to participate.
Additionally, the survey measured conditions under which nontelehealth utilizers would consider using telehealth. The survey asked, “For each of the following, please indicate ‘yes,’ ‘no,’ or ‘unsure:’ I would consider using telehealth in my practice”: The question items included: “if I were paid for visits or consults,” “for follow-up care,” “if it significantly reduces the amount of time my patients spend travelling to see me,” “to connect my patients to subspecialists or other pediatricians,” “to care for my patients,” and “for initial office visits.”
The respondent demographic and practice characteristics used in the bivariate and multivariable analyses included practice area (suburban; rural; urban, inner city; urban, not inner city), practice setting (solo/2 physician practice; group practice/health maintenance organization; medical school/hospital/clinici ), specialty status (primary care pediatrician; subspecialist pediatrician), gender (female; male), geographic region (Northeast; Midwest; South; West), and age (39 years or less; 40–49 years; 50–59 years; 60 years or more). The inclusion of these characteristics was motivated by past analyses of Periodic Survey data and author consensus.
Analysis Plan
We first described the demographic and practice characteristics of the analytic sample. Second, we examined the percent of respondents that report any telehealth use in the past 12 months by demographic and practice characteristics, using chi-squared analysis to assess the statistical significance of differences across groups. Third, we examined perceived barriers to telehealth use, displaying the percent of respondents indicating that each factor is “a major barrier” to telehealth adoption. Then, we analyzed the relationship between perceived barriers to adoption and reporting any telehealth use in the past 12 months. Next, we used 2 separate multivariable logistic regression models to explore how respondent characteristics and perceptions of barriers were associated with our primary dependent variable: reporting any telehealth in the past 12 months (coded “1” if the respondent reported any telehealth in the past 12 months, and “0” otherwise). Finally, we examined the conditions under which nonusers might consider using telehealth. Differences with a P value less than .05 were considered statistically significant. Data were analyzed using R, a statistical software package.23
Results
Demographic and Practice Characteristics of the Analytic Sample
Our analytic sample had a mean age of 48.6 years and was 64% female (Table 1 ). In regards to practice area, 11% of respondents practiced in rural areas, with 41% in suburban areas and the remainder in urban practice areas. Around 12% of respondents were in solo or 2 physician practices, while 56% were in group practices and 31% were in medical schools, hospitals, or clinics. About 35% of respondents practiced in the South region of the United States, 22% in the Northeast, 21% in the West, and 22% in the Midwest. Just under three fourths of respondents identified as primary care pediatricians.
Table 1.
Respondent Characteristics (n = 744)
| % | |
|---|---|
| Age (mean = 48.6; SD = 10.7) | |
| 39 years or less | 25.1 |
| 40–49 years | 29.1 |
| 50–59 years | 27.2 |
| 60+ years | 18.5 |
| Gender | |
| Women | 64.1 |
| Men | 35.9 |
| Area | |
| Suburban | 41.0 |
| Urban, inner city | 20.9 |
| Urban, not inner city | 26.9 |
| Rural | 11.1 |
| Setting | |
| Solo or 2 physician practice | 12.2 |
| Group practice/health maintenance organization | 56.4 |
| Medical school/hospital/clinic | 31.4 |
| Region | |
| Northeast | 21.6 |
| Midwest | 22.0 |
| South | 35.3 |
| West | 20.9 |
| Subspecialist status | |
| Primary care | 73.9 |
| Subspecialist | 26.0 |
SD indicates standard deviation.
Reported Telehealth Use in Past 12 Months
Overall, 12.9% of pediatricians indicated they had used telehealth in the past 12 months, and 6.4% reported they had referred patients for telehealth during that same time (Table 2 ). Taken together, 15.2% of respondents reported any telehealth during the past year (referred and/or used telehealth). There were no differences in reporting any telehealth by age or gender. However, over 20% of pediatricians in rural and urban, not inner city, practice areas reported any telehealth compared to only 8% of suburban pediatricians (P < .001). We also found setting differences, with pediatricians in medical schools, hospitals or clinics most likely to report any telehealth (P = .014). Variation in any telehealth by region also emerged, as over 28% of pediatricians in the West reported any telehealth, compared to only 8% in the Northeast (P < .001). About a quarter of subspecialists reported any telehealth relative to only 12% of primary care pediatricians (P < .001).
Table 2.
Percent Reporting Using Telehealth in Past 12 Months
| % | |
|---|---|
| A. Full sample | |
| Total | |
| Used telehealth | 12.9 |
| Referred patients for telehealth consult | 6.4 |
| Any telehealth (referred and/or used) | 15.2 |
| B. Any telehealth, by characteristic | |
| Age (P = .041) | |
| 39 years or less | 13.9 |
| 40–49 years | 18.9 |
| 50–59 years | 15.7 |
| 60+ years | 12.9 |
| Gender (P = .088) | |
| Women | 13.7 |
| Men | 18.5 |
| Area (P < .001) | |
| Suburban | 7.9 |
| Urban, inner city | 16.2 |
| Urban, not inner city | 21.9 |
| Rural | 24.4 |
| Setting (P = .014) | |
| Solo or 2 physician practice | 15.9 |
| Group practice/health maintenance organization | 12.1 |
| Medical school/hospital/clinic | 20.8 |
| Region (P < .001) | |
| Northeast | 8.2 |
| Midwest | 15.8 |
| South | 11.2 |
| West | 28.4 |
| Subspecialist status (P < .001) | |
| Primary care | 11.7 |
| Subspecialist | 25.7 |
P values refer to results from chi-squared tests assessing the statistical significance of differences in any telehealth use across groups.
Perceived Barriers to Telehealth Use
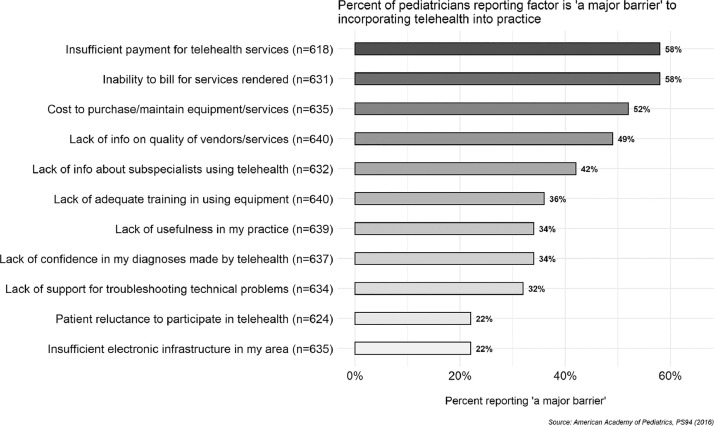
Figure 1 displays pediatricians’ reported barriers to incorporating telehealth into practice and shows that the barriers most commonly noted as “major barriers” were related to the financial aspects of adopting telehealth. The most reported barriers were “insufficient payment for telehealth services” and “inability to bill for services rendered” at 58% reporting, followed by “cost to purchase/maintain equipment/services” at 52% reporting. Barriers related to having specific types of technical information on using telehealth were also reported, as 49% cited “lack of information on quality of vendors/services” and 42% cited “lack of information about subspecialists using telehealth.” Only 22% of respondents identified “patient reluctance to participate in telehealth” and “insufficient electronic infrastructure in my area” as barriers, respectively.
Figure 1.
Perceived barriers to telehealth use.
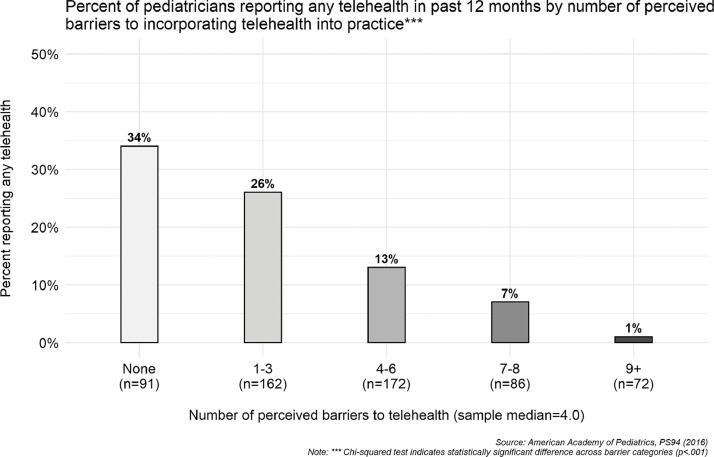
Relationship between Perceived Barriers and Telehealth Use
Building on the results in Figure 1, Figure 2 displays the relationship between number of perceived barriers and reporting any telehealth. We grouped respondents according to the total number of barriers from Figure 1 that they identified as “a major barrier,” and the bars display the percent of respondents in each barrier grouping that reported any telehealth in the past 12 months. Overall, this figure indicates that as respondents perceived more barriers to incorporating telehealth into their practice, they were less likely to report any telehealth (P < .001). Among those perceiving no barriers to telehealth, 34% reported any telehealth in the past 12 months. However, among those perceiving 4 to 6 barriers, the share that reported any telehealth decreased to 13%. Among those perceiving 9 or more barriers, only 1% reported any telehealth use.
Figure 2.
Any telehealth by number of perceived barriers.
Characteristics Associated With Telehealth Use
Using multivariable logistic regression models (Table 3 ), we examined the characteristics associated with reporting any telehealth use. In Model 1, we included only demographic and practice characteristic variables, but in Model 2, we also include the number of perceived barriers to telehealth adoption. Model 1 results indicate that respondents in the West region (adjusted odds ratio [AOR] = 3.57; 95% confidence interval [CI] = 1.73–7.79), in rural areas (AOR = 3.77; 95% CI = 1.78–7.93), in urban, not inner city areas (AOR = 2.33; 95% CI = 1.23–4.48), and working as subspecialists (AOR = 2.47; 95% CI = 1.40–4.36) are more likely to report any telehealth use in the past 12 months.
Table 3.
Logistic Regression Results for Characteristics Associated With “Any Telehealth in Past 12 Months”
| Model 1† |
Model 2‡ |
|||||||
|---|---|---|---|---|---|---|---|---|
| AOR | CI Low | CI High | P Value | AOR | CI Low | CI High | P Value | |
| Gender (ref = men) | ||||||||
| Women | 0.68 | 0.41 | 1.12 | .132 | 0.72 | 0.43 | 1.21 | .211 |
| Age (ref = 39 years or less) | ||||||||
| 40–49 years | 1.31 | 0.68 | 2.56 | .418 | 1.27 | 0.64 | 2.55 | .495 |
| 50–59 years | 1.45 | 0.74 | 2.92 | .285 | 1.35 | 0.67 | 2.79 | .406 |
| 60+ years | 1.03 | 0.47 | 2.27 | .938 | 0.91 | 0.40 | 2.04 | .811 |
| Region (ref = Northeast) | ||||||||
| Midwest | 1.38 | 0.63 | 3.14 | .425 | 1.02 | 0.45 | 2.46 | .924 |
| South | 1.03 | 0.48 | 2.27 | .946 | 0.86 | 0.39 | 1.97 | .710 |
| West | 3.57⁎⁎ | 1.73 | 7.79 | .001 | 3.23⁎⁎ | 1.50 | 7.35 | .004 |
| Setting (ref = solo or 2 physician practice) | ||||||||
| Group practice/health maintenance organization | 0.64 | 0.31 | 1.38 | .237 | 0.46 | 0.21 | 1.02 | .051 |
| Medical school/hospital/clinic | 0.74 | 0.33 | 1.71 | .474 | 0.45 | 0.19 | 1.08 | .069 |
| Area (ref = suburban) | ||||||||
| Urban, inner city | 1.69 | 0.80 | 3.54 | .166 | 1.96 | 0.89 | 4.29 | .092 |
| Urban, not inner city | 2.33* | 1.23 | 4.48 | .010 | 2.16* | 1.11 | 4.26 | .023 |
| Rural | 3.77⁎⁎⁎ | 1.78 | 7.93 | <.001 | 3.76⁎⁎ | 1.72 | 8.22 | .0001 |
| Subspecialty status (ref = primary care) | ||||||||
| Subspecialist | 2.47⁎⁎ | 1.40 | 4.36 | .002 | 2.16* | 1.11 | 4.26 | .021 |
| Number of perceived barriers to incorporating telehealth (ref = none) | ||||||||
| 1–3 barriers | – | – | – | – | 0.73 | 0.39 | 1.36 | .32 |
| 4–6 barriers | – | – | – | – | 0.34⁎⁎ | 0.17 | 0.69 | .003 |
| 7–8 barriers | – | – | – | – | 0.13⁎⁎⁎ | 0.04 | 0.36 | <.001 |
| 9+ barriers | – | – | – | – | 0.03⁎⁎ | 0.01 | 0.17 | .0001 |
CI indicates confidence interval; AOR, adjusted odds ratio.
Dependent variable is any telehealth use in past 12 months (1 = yes, 0 = no); n = 550.
P < .05.
P < .01.
P < .001.
Model controls include only pediatrician demographics/characteristics.
Model controls include pediatrician demographics/characteristics and number of perceived barriers to incorporating telehealth.
In Model 2, which keeps the demographic controls from Model 1 but also includes the number of perceived barriers, we found the same strong negative relationship between number of perceived barriers to telehealth incorporation and reporting any telehealth that we found in the bivariate analysis displayed in Figure 2. While those perceiving 1 to 3 barriers are not statistically different from those perceiving no barriers, with each subsequent increase in barriers we find that respondents were increasingly less likely to have reported any telehealth use. We found that those who identified 4 to 6 barriers (AOR = 0.34; 95% CI = 0.17–0.69), 7 to 8 barriers (AOR = 0.13; 95% CI = 0.17–0.69), and 9 or more barriers (AOR = 0.03; 95% CI = 0.01–0.17) are all significantly less likely to report any telehealth in the past 12 months.
Adopting Telehealth
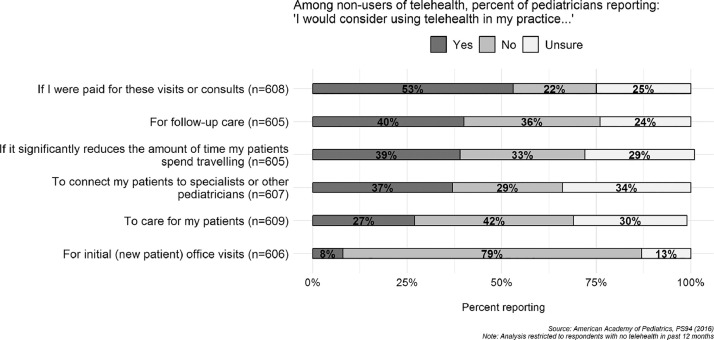
Finally, our analysis examined conditions under which nonusers would consider adopting telehealth (Fig. 3). Results indicated that the top condition under which pediatricians would consider telehealth adoption was if they were “paid for these visits or consults” (53%). Around 40% of respondents indicated that they would consider adopting telehealth for “follow-up care,” if telehealth “significantly reduces the amount of time patients spend travelling,” and to “connect patients to specialists or other pediatricians.” Only 8% reported they would consider adopting for “initial (new patient) office visits.” These results, like the findings presented in Figure 1 on perceived barriers, highlight the extent to which payment and other financial considerations are impediments to pediatricians using telehealth.
Figure 3.
Conditions under which pediatricians would consider using telehealth.
Discussion
In its 2015 policy statement on telehealth, the AAP stated that “telemedicine technologies, applied to the medical home and its collaborating providers, have the potential to improve current models of care,” and recommended that existing financial barriers to telehealth including equipment costs and equitable payment for services be reduced to ensure more patient access to pediatricians.12 The results of this 2016 survey indicated that while some pediatricians had incorporated telehealth into their practice, more work is needed to continue to reduce barriers to telehealth use.
Despite reports of growing telehealth access, our survey results from 2016 indicated that the overall reported use of telehealth was relatively low, with 15% of pediatricians indicating that they had used some kind of telehealth in the past 12 months. Our finding here is consistent with previous estimates of the prevalence of telehealth use among physicians in general.14 , 15 In our survey, pediatricians in rural areas, pediatricians in the West region of the United States, pediatricians in medical school or hospital settings, and pediatric subspecialists were the most likely to report having used telehealth. These findings also reflected previous research that has found that subspecialists and providers in rural areas are more likely to use telehealth.9 , 13 Taken together, these results suggest that while overall use of telehealth by pediatricians was limited, it may play an important role in better connecting patients in underserved, rural areas to pediatric care.5
The survey results on perceived barriers provided some insight into the overall low rates of telehealth use, as our analysis found that a majority of respondents indicated that financial issues are major barriers to incorporating telehealth into their practice. Nearly 6 of 10 respondents identified “insufficient payment for telehealth services” and “inability to bill for services rendered” as barriers, respectively. These results are unsurprising, given that payment and reimbursement policies for telehealth remain fragmented across states, and this inconsistency across geography and payers was identified by the US Department of Health and Human Services as a key policy challenge for expansion of telehealth.5 , 24 Pediatrics is unique in this regard in that, in contrast to adult populations like those covered by Medicare and the Veteran's Administration, there are no federal programs providing uniform payment coverage for telehealth services for pediatrics. Reliance on Medicaid and private payers increases the state-by-state variability of coverage and limits the ability to address payment issues for pediatric telehealth at the federal level. However, the trend in telehealth policy, even prior to COVID-19, is that states and private payers are increasingly incorporating payment for telehealth services, which would create a more favorable payment environment for telehealth in the future.24 , 25
Relatedly, over half of respondents noted the “cost of purchasing/maintaining equipment/services” as a barrier, but continued advancements in telehealth technology should continue to drive down the material costs associated telehealth.4 , 25 Collectively, these results on barriers—coupled with our finding that a majority of nonusers would consider using telehealth if they were paid for the visits or consults—suggest that financial issues are at the forefront of physicians’ decision-making process around adopting telehealth.
Our analysis also added to the existing literature on telehealth use by examining the association between perceived barriers to telehealth incorporation and having used telehealth in the past 12 months. Specifically, we found that as the number of perceived barriers increased, the likelihood of having used telehealth decreased significantly. For example, among those who reported no barriers, 34% reported having used telehealth, but this decreased to 13% among those who reported 4 to 6 barriers. This relationship provides evidence that in order to encourage pediatricians to incorporate telehealth, the full range of potential financial, quality, implementation, administrative, and technical barriers should be addressed and remedied.
Further, our regression models show that pediatricians in rural practice areas, urban, not inner-city practice areas, and the West region were significantly more likely to report telehealth use. Given that telehealth access is heavily shaped by state-level policies, laws, and regulations,24 , 26 the geographic variation observed in our models indicates that there may important differences in telehealth adoption and use by state that is beyond the scope of our data to examine.
Telehealth and COVID-19
Dramatically increased telehealth use has played a critical role in the response to the COVID-19 pandemic in the United States, allowing some patients access to care while avoiding in-person visits to physicians’ offices and hospitals.18 In March 2020, the AAP released guidance for pediatricians related to telehealth policy, noting that it was “working at all levels to strongly advocate for changes that will eliminate burdens on pediatricians seeking to begin or expand use of telehealth care.”17 The federal government, in addition to many state governments, has taken temporary actions to broaden access to telehealth, including relaxing regulations, waiving some state licensure requirements, and expanding Medicare, Medicaid, and Children's Health Insurance Programs eligibility for telehealth payment.20 , 27, 28, 29, 30
It is unclear if the elevated levels of telehealth use will persist, particularly if the temporary government measures related to payment are not extended once the COVID-19 crisis subsides. While the survey data analyzed here were collected well before the outbreak, financial barriers were the top reported barriers to telehealth adoption, indicating that extending actions taken to reduce barriers to payment could encourage more pediatricians to continue to incorporate telehealth into their practice. Clinicians report mixed reviews of the transformation to virtual care during the COVID-19 pandemic; an April 2020 survey of primary care physicians found more telehealth use but also frustrations with implementation including billing problems and patients’ lack of access to technology.31 Thus, while telehealth is being adopted by many medical providers to provide patient care during the response to COVID-19, the extent to which barriers to successful implementation can be identified and remedied will likely play a large role in determining if gains in telehealth use will continue postpandemic.
Limitations
As with any survey-based research, there are several limitations to our findings here. First, this survey is based on respondent self-report, and so there is potential for social desirability bias or recall error. Second, our survey was limited to AAP member pediatricians, and the telehealth experiences of AAP members may differ from non-AAP members; however, this likely did not influence our findings, given that 60% of board-certified pediatricians in the United States between the ages of 27 and 70 were AAP members in 2016, indicating that AAP members represent the majority of board-certified pediatricians. Last, our data were collected in 2016, and so it is possible our estimates of telehealth use by pediatricians are lower than current levels; for instance, since 2016, a number of states have broadened their Medicaid fee-for-service telehealth policies to provide reimbursement for a wider range of telehealth modalities which may have further encouraged telehealth use, and the COVID-19 pandemic has also reportedly produced an increase in telehealth use.26
Conclusion
Although access to telehealth has expanded and it is increasingly discussed as an important, innovative tool that has the potential to reduce costs and expand access to care going forward, our 2016 survey results indicated that only 15% of pediatricians reported using telehealth technologies to provide patient care. Most respondents reported that financial concerns are a major barrier to incorporating telehealth into their practice, and the perception of more barriers was independently associated with a lower likelihood of having any telehealth experience in the past year. Among nonusers, however, most reported that they would use telehealth if financial barriers were resolved. Given that multiple barriers to telehealth incorporation remain across a variety of domains, reducing those impediments will be instrumental in promoting future telehealth adoption among pediatricians. Future surveys will be useful to help track adoption rates, examine if pediatricians continue to use telehealth once the COVID-19 crisis has passed, and evaluate the persistence of barriers to telehealth use by pediatricians.
Acknowledgments
Financial statement: This survey was funded by the American Academy of Pediatrics.
Footnotes
The authors have no conflicts of interest to disclose.
Note: The “medical school/hospital/clinic” category includes respondents who indicated their primary employment setting is one of the following: medical school or parent university, nongovernment hospital or clinic, nonprofit community health center, or US government hospital or clinic.
References
- 1.Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine . In: Telemedicine: A Guide to Assessing Telecommunications in Health Care. Field MJ, editor. National Academies Press (US); Washington (DC): 1996. Available at: http://www.ncbi.nlm.nih.gov/books/NBK45448/. Accessed October 30, 2018. [PubMed] [Google Scholar]
- 2.The Office of the National Coordinator for Health Information Technology. What is telehealth? How is telehealth different from telemedicine? Available at:https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine. 2019. Accessed March 2, 2020.
- 3.Yang YT. Telehealth Parity Laws. 2016:1–5. [Google Scholar]
- 4.Kahn J. Virtual visits—confronting the challenges of telemedicine. N Engl J Med. 2015;372:1684–1685. doi: 10.1056/NEJMp1500533. [DOI] [PubMed] [Google Scholar]
- 5.Office of Health Policy, Office of the Assistant Secretary for Planning and Evaluation . U.S. Department of Health and Human Services; Washington, DC: 2016. Report to Congress: E-Health and Telemedicine. [Google Scholar]
- 6.Gumpert K. Telehealth services becoming popular with US consumers and insurers. Reuters. 2015. Available at: https://www.reuters.com/article/usa-healthcare-telemedicine-idUSL1N14B20B20151223. Accessed October 30, 2018.
- 7.Khullar D. Telemedicine is getting trendy, but doctors may not be keeping up. The Washington Post. 2018 Available at: https://www.washingtonpost.com/national/health-science/telemedicine-is-getting-trendy-but-doctors-may-not-be-keeping-up/2018/04/20/681e1644-2178-11e8-badd-7c9f29a55815_story.html. Accessed October 30, 2018. [Google Scholar]
- 8.American Hospital Association . American Hospital Association; Chicago, Ill: 2017. Fact Sheet: Telehealth. Available at: https://www.aha.org/system/files/2018-01/fs-telehealth.pdf. Accessed May 26, 2020. [Google Scholar]
- 9.Institute of Medicine . The National Academies Press; Washington, DC: 2012. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. Available at: https://www.ncbi.nlm.nih.gov/books/NBK207145/. Accessed October 30, 2018. [PubMed] [Google Scholar]
- 10.Adler-Milstein J, Kvedar J, Bates DW. Telehealth among US hospitals: several factors, including state reimbursement and licensure policies, influence adoption. Health Aff Proj Hope. 2014;33:207–215. doi: 10.1377/hlthaff.2013.1054. [DOI] [PubMed] [Google Scholar]
- 11.Younts J. Berkeley Research Group; Washington (DC): 2015. Telehealth Utilization: Potential Benefits of Expanded Coverage and Reimbursement. Available at: https://www.thinkbrg.com/media/publication/689_689_Younts_Telehealth_Whitepaper_20150916.pdf. Accessed May 26, 2020. [Google Scholar]
- 12.Marcin J, Rimsza ME, Moskowitz W. The use of telemedicine to address access and physician workforce shortages. Pediatrics. 2015;136:202–209. doi: 10.1542/peds.2015-1253. [DOI] [PubMed] [Google Scholar]
- 13.Burke BL, Hall RW. Telemedicine: pediatric applications. Pediatrics. 2015;136:e293–e308. doi: 10.1542/peds.2015-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood) 2018;37:1923–1930. doi: 10.1377/hlthaff.2018.05077. [DOI] [PubMed] [Google Scholar]
- 15.Moore MA, Coffman M, Jetty A. Only 15% of FPs report using telehealth; training and lack of reimbursement are top barriers. Am Fam Physician. 2016;93:101. [PubMed] [Google Scholar]
- 16.Olson CA, McSwain SD, Curfman AL. The current pediatric telehealth landscape. Pediatrics. 2018;141 doi: 10.1542/peds.2017-2334. [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Pediatrics. AAP Guidance: telehealth payer policy in response to COVID-19. 2020. Available at: http://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/aap-guidance-telehealth-payer-policy-in-response-to-covid-19/. Accessed April 15, 2020.
- 18.Coombs B. Telehealth visits are booming as doctors and patients embrace distancing amid the coronavirus crisis. CNBC. 2020 Available at: https://www.cnbc.com/2020/04/03/telehealth-visits-could-top-1-billion-in-2020-amid-the-coronavirus-crisis.html. Accessed April 15, 2020. [Google Scholar]
- 19.Jordan K. An unexpected benefit of the pandemic: the doctor will virtually see you now. The Washington Post. April 14, 2020. Available at: https://www.washingtonpost.com/outlook/2020/04/14/telemedicine-virtual-health-coronavirus/. Accessed April 15, 2020.
- 20.Robeznieks A. Key Changes Made to Telehealth Guidelines to Boost COVID-19 Care. American Medical Association. 2020. Available at: https://www.ama-assn.org/delivering-care/public-health/key-changes-made-telehealth-guidelines-boost-covid-19-care. Accessed April 15, 2020.
- 21.Arizton Advisory & Intelligence. The telehealth market in US to reach revenues of over $25 billion during the period 2020−2025. PRNewswire. April 15, 2020. Available at: https://www.prnewswire.com/news-releases/the-telehealth-market-in-us-to-reach-revenues-of-over-25-billion-during-the-period-2020-2025s-market-research-by-arizton-301040962.html. Accessed April 15, 2020.
- 22.Primary Care Collaborative; Larry A. Green Center. Primary Care & COVID-19: Week 2 Survey. Washington (DC): Primary Care Collaborative. March 26, 2020. Available at: https://www.pcpcc.org/2020/03/26/primary-care-covid-19-week-2-survey. Accessed April 15, 2020.
- 23.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. Available at: https://www.R-project.org/. Accessed May 26, 2020.
- 24.Center for Connected Health Policy . National Telehealth Policy Resource Center; Sacramento, Calif: 2019. State Telehealth Laws and Reimbursement Policies. Available at: https://www.cchpca.org/sites/default/files/2019-05/cchp_report_MASTER_spring_2019_FINAL.pdf. Accessed May 26, 2020. [Google Scholar]
- 25.American Academy of Pediatrics. Economics of Telehealth. Itasca, Ill. 2020. Available at: https://www.aap.org/en-us/professional-resources/practice-transformation/economics/Pages/Economics-of-Telehealth.aspx. Accessed May 26, 2020.
- 26.Center for Connected Health Policy . National Telehealth Policy Resource Center; Sacramento, Calif: 2020. State Telehealth Medicaid Fee-For-Service Policy: A Historical Analysis of Telehealth, 2013–2019. Available at: https://www.cchpca.org/sites/default/files/2020-01/Historical%20State%20Telehealth%20Medicaid%20Fee%20For%20Service%20Policy%20Report%20FINAL.pdf. Accessed May 26, 2020. [Google Scholar]
- 27.Trzcinski A. Quick resource guide to help organizations scale healthcare support during COVID-19. Forrester. 2020. Available at: https://go.forrester.com/blogs/quick-resource-guide-to-help-organizations-scale-healthcare-support-during-covid-19/. Accessed April 15, 2020.
- 28.Alliance for Connected Care. State telehealth and licensure expansion COVID-19 dashboard. Washington, DC; 2020. Available at:http://connectwithcare.org/state-telehealth-and-licensure-expansion-covid-19-chart/. Accessed April 15, 2020.
- 29.American Academy of Family Physicians. Using telehealth to care for patients during the COVID-19 pandemic. 2020. Available at: https://www.aafp.org/patient-care/emergency/2019-coronavirus/telehealth.html. Accessed April 15, 2020.
- 30.Centers for Medicare & Medicaid Services. Fact sheet: Medicare telemedicine health care provider fact sheet. March 17, 2020. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed April 15, 2020.
- 31.Primary Care Collaborative; Larry A. Green Center. Primary Care & COVID-19: Week 4 Survey. Washington (DC): Primary Care Collaborative. April 8, 2020. Available at: https://www.pcpcc.org/2020/04/08/primary-care-covid-19-week-4-survey?language=en. Accessed April 15, 2020.