Dear Editor,
A recent article in Journal of Infection by Lv et al. projected that many countries could face similar COVID-19 situations as witnessed in Hubei in China.1 There are many factors that can influence the course of an infectious disease outbreak.
In the wake of the Ebola outbreak in 2014, the Global Health Security Index (GHSI) was developed with the aim of gauging countries’ capacity to deal with infectious disease outbreaks.2 The GHSI highlights the shortcomings of existing pandemic policies and procedures, with the aim of spurring improvement of future practices. The index ranges from 0 to 100, and assesses six core elements: prevention, detection and reporting, response, health system, compliance with norms and risk of infectious disease outbreaks.2 A higher GHSI indicates better preparedness.
In the present study, we examined the correlation between GHSI and various measures of COVID-19 burden across different countries. We hypothesised that higher GHSI was inversely associated with measures of COVID-19 burden.
Country-level data on COVID-19 as at 11 April 2020 were sourced from the ‘worldometer’.3 Countries without testing data, or those with no assigned GHSI score were excluded. Furthermore, we included only countries with at least 100 confirmed cases of COVD-19. Data on countries’ median age and proportion of females in 2019 were sourced from the United Nations population database.4
We analysed the association between GHSI and COVID-19 burden, represented by numbers of tests confirmed cases and deaths per million people per day since the first confirmed case in each country. First, we plotted GHSI against natural log transformed values of these outcomes (to provide more symmetrical distributions). Secondly, we used a generalised linear model (GLM) to determine the association between GHSI and confirmed cases and deaths per million people per day, with adjustment for testing rate, population median age and proportion of females.
We considered GHSI both as a continuous variable and as a categorical variable comprising four quartiles. In the latter analyses, the first (lowest) quarter of GHSI was considered as the reference category.
A total of 100 countries with complete data were included in the analysis (Supplementary Table S1). At the time of the analyses, there were 1,431,533 confirmed COVID-19 cases globally and 82,058 deaths. The median number of tests per million population across the included countries was 2486 (interquartile range [IQR] 623-9515). The countries with the highest and lowest testing rates were Iceland (84,957 per million population) and Nigeria (24 per million population), respectively. The median number of cases and deaths per million population were 207 (IQR: 35-498) and 3 (IQR: 0•8-11), respectively.
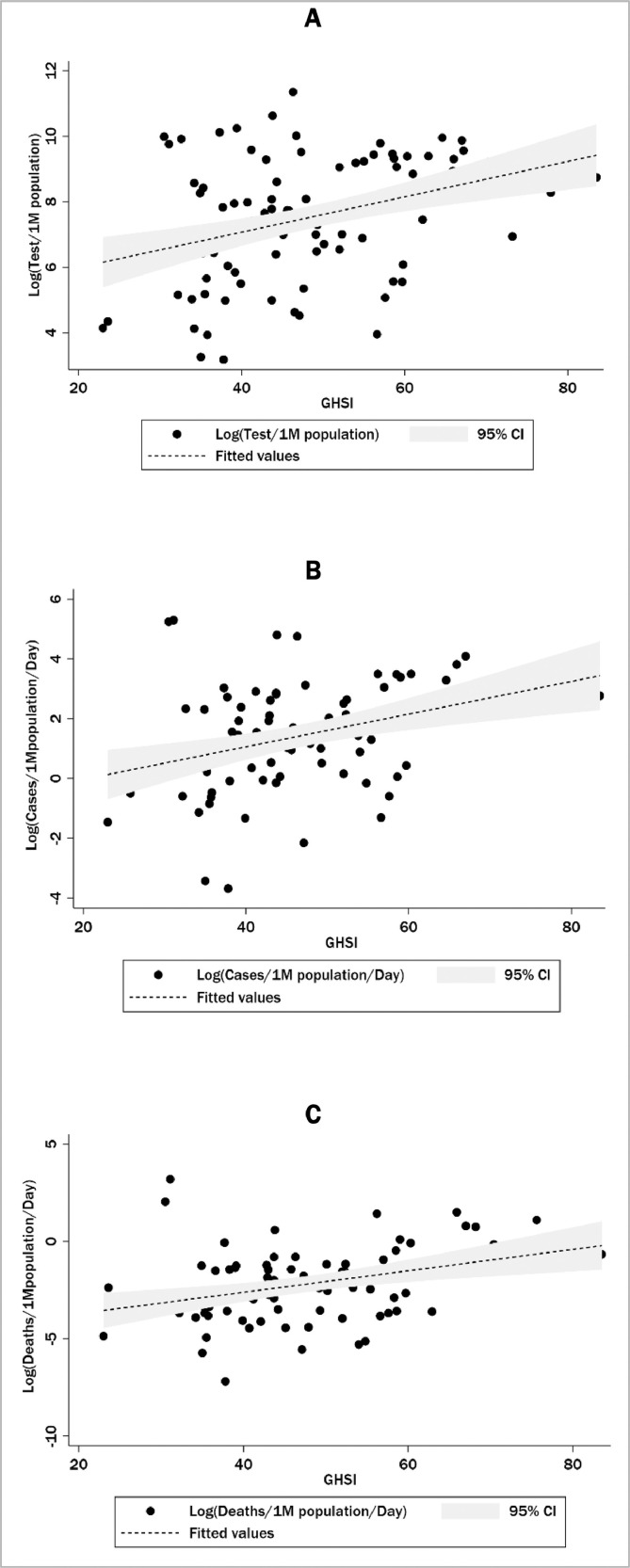
COVID-19 metrics (log transformed) plotted against GHSI are presented in Fig. 1 . These suggest a positive correlation between GHSI and testing rate, as well as cases and deaths per million people per day since the first recorded case. Of note, the US was the highest ranked country in terms of GHSI of all 100 countries analysed yet had the largest number of COVID-19 cases worldwide at the time of analyses.2 , 3 Second-ranked UK was also bearing a large burden of disease.
Figure 1.
Scatter plot of showing unadjusted correlation between GHSI and testing rate (A), COVID-19 cases (B) and deaths (C) per million people per day.
The results from the GLM model are presented in Table 1 . There was no statistically significant association observed between GHSI and testing rate. After adjusting for testing rate, median age and the proportion of females, a positive association was also observed between GHSI and COVID-19 cases and deaths, with the biggest burden borne by countries at the highest quartile of GHSI.
Table 1.
Relationship between GHSI and COVID-19 measures.
| COVID-19 metric | GHSI (continuous) | Incidence rate ratio (95% confidence interval) |
|||
|---|---|---|---|---|---|
| GHSI quartile |
|||||
| Q1 | Q2 | Q3 | Q4 | ||
| Tests per million people | 1.01 (0.97-1.03), p=0.210 | 1.0 (ref) | 2.22 (0.78-6.30), p=0.135 | 1.08 (0.47-2.47), p=0.858 | 1.88 (0.89-4.01), p=0.099 |
| Cases per million people per day (unadjusted) | 0.99 (0.96-1.04), p=0.858 | 1.0 (ref) | 0.87 (0.22-3.45), p=0.842 | 0.46 (0.14-1.48), p=0.193 | 1.16 (0.37-3.67), p=0.798 |
| Cases per million people per day (adjusted)a | 1.02 (1.01-1.03), p=0.011 | 1.0 (ref) | 1.69 (0.76-3.71), p=0.195 | 1.46 (0.80-2.65), p=0.212 | 2.56 (1.49-4.55), p=0.001 |
| Deaths per million people per day (unadjusted) | 0.99 (0.91-1.07), p=0.728 | 1.0 (ref) | 0.15 (0.03-0.74), p=0.020 | 0.22 (0.38-1.30), p=0.096 | 0.87 (0.19-3.90), p=0.854 |
| Deaths per million people per day (adjusted)a | 1.05 (1.02-1.07), p<0.001 | 1.0 (ref) | 1.09 (0.34-3.47), p=0.879 | 1.28 (0.43-3.86), p=0.655 | 3.56 (1.25-10.1), p=0.017 |
Adjusted for testing rate, age and sex; IRR=incidence rate ratio
The findings of our study were unexpected. First, no association was noted between GHSI and testing rate, despite that GHSI should serve as a surrogate for healthcare capacity, including COVID-19 testing. Effective pandemic response requires significant investment in testing, with adequate training of healthcare workers in testing, as well as sufficient supply of PPE and testing kits.5 In addition, effective and widespread dissemination of information to the general population regarding testing criteria assists case detection.5
Secondly, the associations between GHSI and COVID-19 cases and deaths were positive, meaning that the GHSI can reflect a country's capacity to deal with epidemics or pandemics, but in the opposite manner than intended. No doubt there was confounding by increased globalisation among more developed countries (with higher GHSI). Increased exposure to foreigners travelling for the purposes of tourism, business and use of healthcare is likely to increase the risk of new infectious pathogens being introduced. Similarly, mass migration contributes to disruption of local bacterial and viral environments.2 Furthermore, the rarity of pandemics in conjunction with false reassurance from a high GHSI may have contributed to more lenient adherence to infection control mechanisms in recent years.6
The intent of the GHSI is noble, and the findings of our study should not discourage future endeavours to gauge capacity to respond to pandemics. However, as the world becomes increasingly interconnected, the value of assessing the capacity of countries to manage infectious disease outbreaks individually is redundant. This interconnectedness extends beyond social, political, and business interactions to pathogenic environments. Consequently, identifying and controlling spread of newly arising infectious agents is only as effective as the practices within the poorest performing countries.
The COVID-19 pandemic has revealed insufficiencies in existing knowledge of pandemic preparedness and response. A more integrated global approach is necessary, as is further research into alternative factors related to infection control that have not yet been considered. Development of international response protocols and effective communication channels will permit coordinated global action. Furthermore, establishment of dynamic models and tools will ensure the world is better prepared for future outbreaks.
Acknowledgments
Acknowledgement
None
Funding
None
Conflicts of interest
None
Authors contribution statement
All authors contributed to study design, data analysis and manuscript preparation. All authors read and approved final version before submission
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2020.05.001.
Appendix. Supplementary materials
References
- 1.Lv B., Li Z., Chen Y. Global COVID-19 fatality analysis reveals Hubei-like countries potentially with severe outbreaks. J Infect. 2020 Apr 14 doi: 10.1016/j.jinf.2020.03.029. pii: S0163-4453(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nuclear Threat Initiative, Johns Hopkins Center for Health Security, The Economist Intelligence Unit. Global Health Security Index. Available from:https://www.ghsindex.org/(Accessed April 13 2020).
- 3.Worldometers.info. Worldometer COVID-19 Coronavirus Pandemic. Available from:https://www.worldometers.info/coronavirus/(Accessed April 26, 2020).
- 4.United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019 Available from:https://population.un.org/wpp/Download/Standard/Population/(Accessed April 11, 2020).
- 5.Krumkamp R., Ahmad A., Kassen A., Hjarnoe L., Syed A.M., Aro A.R. Evaluation of national pandemic management policies—A hazard analysis of critical control points approach. Health Policy. 2009;92(1):21–26. doi: 10.1016/j.healthpol.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation . The world health report 2007 - A safer future: global public health security in the 21st century. In: Heymann D.L., Prentice Thomson, Reinders Lina Tucker, editors. World Health Organisation; Geneva: 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.