Highlights
-
•
Brixia score is a new chest X-ray scoring system designed for COVID-19 pneumonia.
-
•
Brixia score, patient age and immunosuppressive conditions predict fatal outcome.
-
•
High Brixiascore and at least one other predictor confer the highest risk of death.
Keywords: SARS-CoV-2, COVID-19, Chest X-ray, Scoring system
Abstract
Objectives
This study aimed to assess the usefulness of a new chest X-ray scoring system — the Brixia score — to predict the risk of in-hospital mortality in hospitalized patients with coronavirus disease 2019 (COVID-19).
Methods
Between March 4, 2020 and March 24, 2020, all CXR reports including the Brixia score were retrieved. We enrolled only hospitalized Caucasian patients with COVID-19 for whom the final outcome was available. For each patient, age, sex, underlying comorbidities, immunosuppressive therapies, and the CXR report containing the highest score were considered for analysis. These independent variables were analyzed using a multivariable logistic regression model to extract the predictive factors for in-hospital mortality.
Results
302 Caucasian patients who were hospitalized for COVID-19 were enrolled. In the multivariable logistic regression model, only Brixia score, patient age, and conditions that induced immunosuppression were the significant predictive factors for in-hospital mortality. According to receiver operating characteristic curve analyses, the optimal cutoff values for Brixia score and patient age were 8 points and 71 years, respectively. Three different models that included the Brixia score showed excellent predictive power.
Conclusions
Patients with a high Brixia score and at least one other predictive factor had the highest risk of in-hospital death.
Introduction
Coronavirus disease 2019 (COVID-19), caused by a novel virus — the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) — has now become a pandemic. Currently, more than 200 countries, territories or areas are affected by this novel infectious disease (World Health Organization, 2020). On April 10, 2020, the overall number of confirmed COVID-19 cases was 1 521 252 worldwide, with a mortality rate of 6.1% (World Health Organization, 2020). Given the recent estimates of mortality rate for COVID-19 (Baud et al., 2020), clinicians should be aware of the risk factors associated with a fatal outcome. The literature reports that an older age, presence of underlying comorbidities (such as hypertension, diabetes, and cardiovascular disease), certain laboratory parameters, and severity of lung abnormalities are associated with an increased risk of mortality in patients with SARS-CoV-2 infection (Ruan et al., 2020; Wang et al., 2020; Yuan et al., 2020; Zhou et al., 2020). To improve the risk stratification for infected patients, we have introduced in clinical practice a new chest X-ray (CXR) scoring system for quantifying and monitoring the severity of lung abnormalities in patients with COVID-19 (Borghesi and Maroldi, 2020). This CXR scoring system (named the Brixia score) grades lung abnormalities due to COVID-19 on an 18-point severity scale (Borghesi and Maroldi, 2020). To the best of our knowledge, the predictive value of a CXR scoring system in patients with COVID-19 has not yet been studied. Therefore, this study aimed to investigate the usefulness of our CXR scoring system for predicting the risk of in-hospital mortality in patients with SARS-CoV-2 infection.
Materials and Methods
Through a retrospective search on the digital hospital archives between March 4, 2020 and March 24, 2020, all CXR reports including the new scoring system (the Brixia score) were retrieved. We enrolled only hospitalized Caucasian patients with COVID-19 (confirmed by real-time polymerase chain reaction) for whom the final outcome (recovery or death) was available. Patients with incomplete information about the presence of underlying comorbidities and immunosuppressive therapies were excluded from the study. For each included patient, only the CXR report with the highest score was considered for analysis. Each frontal chest projection linked to these reports was independently reviewed by a thoracic radiologist (A.B.), with 15 years’ experience of thoracic imaging, who reassigned the Brixia score. All chest X-rays were performed using portable digital radiography systems.
Notification of this retrospective study was presented to the Institutional Ethical Committee. Given the retrospective design of the study, the need for informed consent was waived.
To investigate significant differences between recovered and dead patients, we selected nine independent variables that were presumed to influence the final outcome (Table 1 ). These variables were analyzed using chi-square or Mann-Whitney U tests. The significant variables were subsequently included in a multivariable logistic regression model to extract the independent predictive factors for in-hospital mortality. In addition, the predictive power of the model was expressed as area under the curve. p-Values of <0.05 were considered statistically significant.
Table 1.
Association between the final outcome and the selected independent variables.
| Independent variables | Total (302) | Final outcome |
p-Value* | |
|---|---|---|---|---|
| Recovery (237) | Death (65) | |||
| Patient age, years | 67.0 (57.0–77.0) | 64.0 (54.0–73.3) | 77.0 (70.5–81.0) | <0.0001 |
| Patient sex | ||||
| Male | 194 (64.2) | 144 (47.7) | 50 (16.6) | 0.0162 |
| Female | 108 (35.8) | 93 (30.8) | 15 (5.0) | |
| Brixia score | 8.0 (5.0–11.0) | 7.0 (4.0–10.0) | 11.0 (9–13.0) | <0.0001 |
| Hypertension | ||||
| Yes | 154 (51.0) | 112 (37.1) | 42 (13.9) | 0.0133 |
| No | 148 (49.0) | 125 (41.4) | 23 (7.6) | |
| Cardiovascular disease | ||||
| Yes | 126 (41.7) | 84 (27.8) | 42 (13.9) | <0.0001 |
| No | 176 (58.3) | 153 (50.7) | 23 (7.6) | |
| Diabetes | ||||
| Yes | 38 (12.6) | 25 (8.3) | 13 (4.3) | 0.0422 |
| No | 264 (87.4) | 212 (70.2) | 52 (17.2) | |
| Chronic obstructive/restrictive lung disease | ||||
| Yes | 44 (14.6) | 31 (10.3) | 13 (4.3) | 0.1620 |
| No | 258 (85.4) | 206 (68.2) | 52 (17.2) | |
| Oncological history within the past 5 years | ||||
| Yes | 56 (18.5) | 36 (11.9) | 20 (6.6) | 0.0043 |
| No | 246 (81.5) | 201 (66.6) | 45 (14.9) | |
| T/D inducing immunosupppresion | ||||
| Yes | 98 (32.5) | 62 (20.5) | 36 (11.9) | <0.0001 |
| No | 204 (67.5) | 175 (57.9) | 29 (9.6) | |
Data are presented as numbers (%) or medians (interquartile range); *p-values obtained by Mann–Whitney U test or chi-square test; T/D, therapy or disease.
Results
We identified 302 Caucasian patients who were hospitalized for COVID-19 (Table 1). The relationships between the final outcome and the selected independent variables are summarized in Table 1. In the multivariable logistic regression model, only Brixia score, patient age, and conditions that induced immunosuppression were independent predictive factors for in-hospital mortality, and were therefore included in the predictive model (Table 2 ). With regard to immunosuppressive conditions, most patients had advanced renal failure (42%), hematological disorders (20%), or were treated with corticosteroids (18%).
Table 2.
Multivariable logistic regression analysis.
| Predictive factor | Coefficient | p-Value | Odds ratio | 95% CI |
|---|---|---|---|---|
| Brixia score | 0.283 | <0.0001 | 1.327 | 1.200–1.472 |
| Age | 0.078 | <0.0001 | 1.081 | 1.046–1.118 |
| T/D inducing immunosupppresion | 0.745 | 0.0278 | 2.106 | 1.085–4.087 |
T/D, therapy or disease; CI, confidence interval.
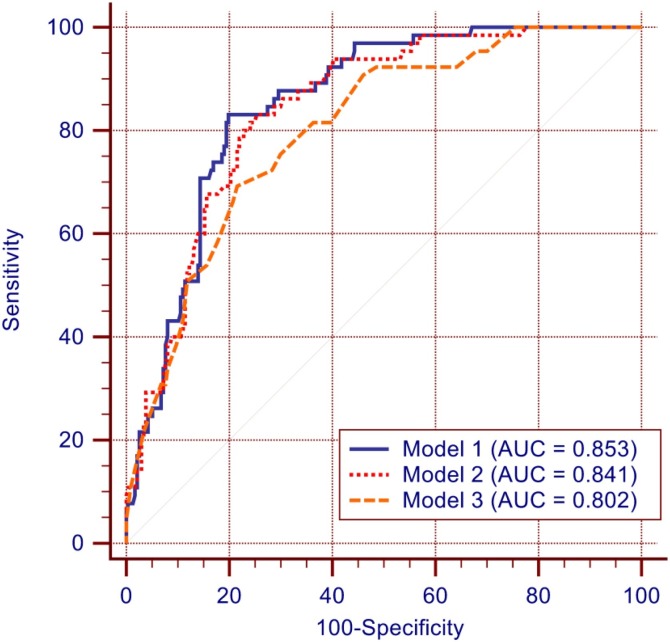
According to receiver operating characteristic curve analyses, the optimal cutoff values for Brixia score and patient age were 8 points and 71 years, respectively. Three different models that included the Brixia score showed excellent predictive power (Figure 1 ).
Figure 1.
Comparison of receiver operating characteristic (ROC) curves generated using the three risk prediction models. Solid blue line (Model 1): ROC curve obtained using all three predictive factors. Dotted red line (Model 2): ROC curve obtained using Brixia score and patient age. Dashed orange line (Model 3): ROC curve obtained using Brixia score and immunosuppressive conditions.
Discussion
For our large study cohort, in-hospital mortality was 21.5%, and higher in men than in women. Multivariable analysis showed that only Brixia score, patient age, and immunosuppressive conditions were the risk factors strongly associated with in-hospital mortality.
In line with the findings of many authors, our study found that older age and severity of lung abnormalities were associated with poor prognosis in patients with COVID-19 (Ruan et al., 2020; Wang et al., 2020; Yuan et al., 2020; Zhou et al., 2020). In addition, as reported in another study (Zhou et al., 2020), our results did not confirm the predictive power of underlying comorbidities such as hypertension, cardiovascular disease, diabetes, chronic lung disease, and oncological history.
The currently available data on the impact of immunosuppressive status on mortality in COVID-19 are few, with a limited number of patients, and obtained almost exclusively from Asian patients (Minotti et al., 2020). In our large cohort of adult Caucasian patients, we observed that immunosuppressive conditions significantly increased the risk of in-hospital mortality (Table 2). Therefore, we believe that our results will be of great importance and will help clinicians in determining appropriate clinical management by improving risk stratification in infected patients.
The major strength of this study is the large sample size, which comprised only Caucasian patients. Although several studies have investigated the role of CT score in patients with COVID-19 (Bernheim et al., 2020, Pan et al., 2020, Yuan et al., 2020), this is the first study to assess the effectiveness of a CXR scoring system for predicting in-hospital mortality in infected patients. The main limitations of this study include the retrospective study design and lack of laboratory parameters included in the predictive models (because these data were collected from a limited number of cases).
In conclusion, this study demonstrated for the first time that a high Brixia score and at least one other predictive factor — patient age and conditions that induced immunosuppression — conferred the highest risk of death due to COVID-19. This information may help clinicians with patient management and treatment planning, and would help them prepare for possible adverse outcomes.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors would like to thank their colleagues in the Diagnostic Imaging Department, ASST Spedali Civili of Brescia. Special thanks to EL.CO. s.r.l. (Savona, Italy) for their outstanding technical support.
References
- Baud D., Qi X., Nielsen-Saines K., Musso D., Pomar L., Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30195-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N. Chest CT findings in coronavirus disease-19 (COVID-19): Relationship to duration of infection. Radiology. 2020;295:685–691. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borghesi A., Maroldi R. COVID-19 outbreak in Italy: experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol Med. 2020;125:509–513. doi: 10.1007/s11547-020-01200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minotti C., Tirelli F., Barbieri E., Giaquinto C., Donà D. How is immunosuppressive status affecting children and adults in SARS-CoV-2 infection? A systematic review. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.026. pii:S0163-4453(20)30237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan F., Ye T., Sun P., Gui S., Liang B., Li L. Time course of lung changes at chest CT during recovery from coronavirus disease (COVID-19) Radiology. 2020;295:715–721. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Yang B., Li Q., Wen L., Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). Coronavirus disease 2019 (COVID-19). Situation Report—81. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. [Accessed 10 April 2020].
- Yuan M., Yin W., Tao Z., Tan W., Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS One. 2020;15 doi: 10.1371/journal.pone.0230548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;6736:1–9. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]