Highlights
-
•
COVID-19 is a pandemic caused by SARS-CoV-2.
-
•
The pandemic first originated in Wuhan the capital of Hubei province, China in December 2019 and then spread globally.
-
•
The disease trajectory in paediatric patients has a good prognosis.
-
•
Case fatality rate is low. However, it is there.
-
•
The most frequent symptoms in children are cough and fever.
-
•
Vertical and breast milk transmission are yet to be established.
Keywords: COVID-19, Wuhan, SARS-CoV-2, vertical transmission, Paediatrics
Abstract
Background
Coronavirus disease 2019 (COVID-19) is a pandemic first originated in Wuhan the capital of Hubei province, China in December 2019 and then spread globally. It is caused by SARS-CoV-2. Until 1st April 2020, the number of cases worldwide was recorded to be 823,626 with 40,598 deaths. Most of the reported cases were adults with few cases described in children and neonates.
Objectives
We performed a systematic review and meta-analysis to analyse the disease characterisation in paediatric age group including the possibility of vertical transmission to the neonates.
Methods
Articles published up to 2nd April 2020 in PubMed and google Scholar were considered for this study.
Findings
The most frequently reported symptoms were cough 49% (95% CI: 42 – 55%) and fever 47% (95% CI: 41- 53%). Lymphopenia and increased Procalcitonin were recorded in (21%, 95% CI: 12 – 30%) and (28%, 95% CI: 18 – 37%) respectively. No sex difference for COVID-19 was found in paediatric age group (p = 0.7). Case fatality rate was 0%. Four out of 58 neonates (6.8%) born to COVID-19 confirmed mothers tested positive for the disease.
Conclusion
The disease trajectory in Paediatric patients has good prognosis compared to adults. Intensive care unit and death are rare. Vertical transmission and virus shedding in breast milk are yet to be established.
1. Introduction
Coronavirus disease 2019 (COVID-19) is a pandemic that originated in Wuhan, China in December 2019 and then spread globally. Although the consequences of COVID-19 infection are devastating, it can be described as a primarily disease of adulthood rather than childhood as inferred by the reported number of cases worldwide [1]. On the 3rd of January 2020, the Chinese Center for Disease Control and Prevention confirmed that the disease is caused by a novel member of enveloped RNA coronavirus [[2], [3], [4]]. The International Committee on Taxonomy of Viruses officially announced the name of this new corona virus to be “Severe Acute Respiratory Syndrome Coronavirus 2” (SARS-CoV-2). The World Health Organization (WHO) announced that the official name of the disease caused by SARS-CoV-2 is Corona Virus Disease-19 (COVID-19) [5]. Herein, we reviewed the characterisation of COVID-19 infections in the Paediatric age group.
1.1. Mode of transmission
The initial infections were linked to Huanan Seafood market in China, mostly due to animal contact. However, COVID-19 is not considered as direct zoonosis as its transmission now is primarily human to human [6]. The mode of transmission of the virus between humans is via respiratory droplets [7]. However, aerosol spread could be a potential route of transmission as illustrated by a study investigating the aerosol and surface stability of SARS-CoV-2 [8], where the authors studied the viability of the virion particles on different surfaces including stainless-steel, plastic, cardboard, and copper as well as in aerosol particles (< 5 μm). It was found that the virus remains viable in aerosol particles for up to 3 hours with a median half-life of 1.2 hours [8]. The virus is more stable on plastic and stainless- steel surfaces than on copper and cardboard. The viability of the virus was found to be up to 3 days on plastic and stainless-steel, 24 hours on cardboard, and 4 hours on copper surfaces [8]. Direct contact is another source of virus transmission via touching the mouth, nose or conjunctiva with contaminated fingers [9].
Vertical transmission is still a matter of debate and yet to be established. In two studies performed on pregnant women with confirmed COVID-19 infection who delivered by either normal vaginal delivery or caesarean section, all neonates tested negative for COVID-19 [10,11]. Other study has found that 3 out of 33 neonates born to COVID-19 positive mothers had positive nasopharyngeal and rectal swabs for COVID-19 [12]. Fecal-oral transmission could be an alternative route of transmission as several studies have reported positive stool samples, even after nasopharyngeal/throat swabs were COVID-19 negative [13,14].
1.2. Pathogenesis
SARS-CoV-2 is primarily a lung pathogen. Its entry to the lung is facilitated by the binding of S protein to angiotensin-converting enzyme 2 (ACE2) receptors [15], which may be the same as SARS-CoV which also enter cells via ACE2 receptors [16,17]. Moreover, it uses the host Transmembrane protease serine 2 (TMPRSS2) for S protein priming and fusion of viral and host cell membranes [6]. ACE2 receptor binding can be shown by two lines of evidence: (1) sequence analysis of the receptor binding motif, which is the part of receptor binding domain that comes into direct contact with ACE2 receptor, which has revealed extensive similarities between SARS-CoV and SARS-CoV-2, and (2) the blockade of SARS-2-S driven cell entry by using human ACE2 antisera.
1.3. Diagnostic tools
1.3.1. Laboratory diagnosis
The gold standard test for SARS-CoV-2 is the real-time reverse transcriptase-polymerase chain reaction (RT-PCR) test. It is believed to be highly specific, and its sensitivity was reported to be 91% [95% CI: 83-97%] for initial RT-PCR [18]. Other study reported RT-PCR sensitivity as high as 95-97% [19].
1.3.2. Radiology
Although less sensitive than chest computed tomography (CT), chest radiography is the first-line imaging modality used to scan patients with suspected COVID-19. Its abnormalities mirror those of the CT and include consolidation or ground-glass opacity (GGO), which in most cases are bilateral and peripheral, and have lower zone predominance. Lung ultrasound may be also useful in the evaluation of critically ill COVID-19 patients [21,22]. The utilisation of CT radiological findings to diagnose/screen for COVID-19 is controversy. An American-Singaporean panel published that CT findings were not part of the diagnostic criteria for COVID-19 [19]. However, CT findings have been used as a surrogate diagnostic test by others [23,24].
2. Methods
2.1. Data sources
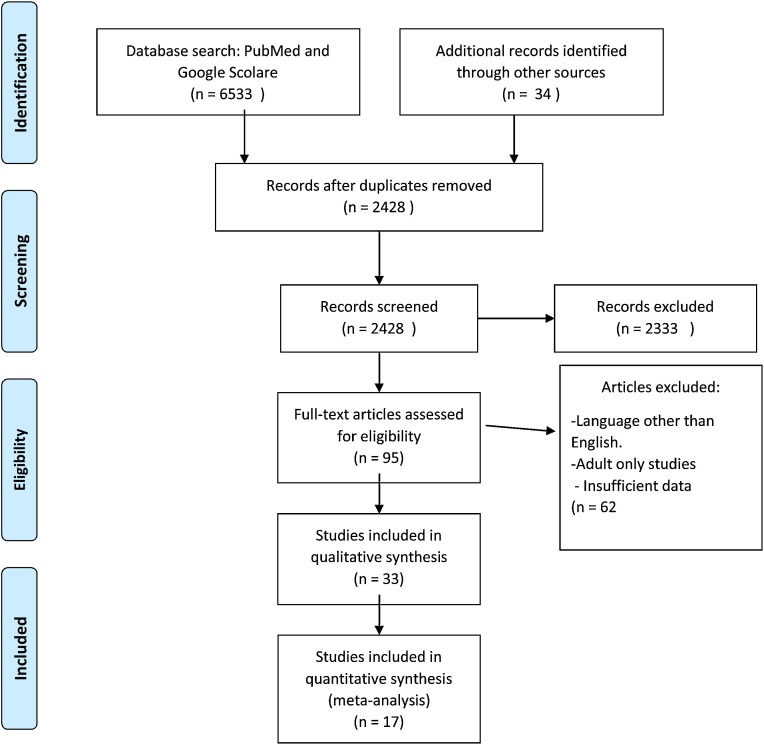
We searched PubMed and Google Scholar from inception through 2 April 2020 using the words “COVID”, “COVID-19”, “COVID” AND “children”, “COVID” AND “neonates”, “SARS-CoV-2”, “SARS-CoV-2” AND “children”, “Wuhan” AND “children” AND “COVID”, “COVID” AND “vertical transmission”, “COVID” AND “ACE2”, “COVID” AND “ICU”, “COVID” AND “epidemiology”, “COVID-19” AND radiology”, “COVID-19” AND “CT”. For further relevant studies, the references of selected articles were also identified through manual search. The literature search process is presented in (Fig. 1 ).
Fig. 1.
Flow diagram of the number of studies screened and included in the meta-analysis.
2.2. Inclusion and exclusion criteria
We included all studies that have reported the clinical picture, laboratory diagnosis, modes of transmission of COVID-19 in Paediatric age group. The excluded articles were published in languages other than English, adult only studies, abstract only, and studies with insufficient data to be analysed.
2.3. Statistical analysis
Data were collated in Microsoft Excel 2019 MSO 64-bit then analysed using RStudio version 3.6.1 (R. RStudio, Inc., Boston, MA), packages “Hmisc”. Categorical variables were expressed as number (%). Numerical variables were expressed as median and range or mean and standard deviation as appropriate. p values of less than 0.05 were assigned significance.
3. Results
3.1. Vertical transmission and the outcome of neonates born to COVID19 confirmed mouthers
Six studies [10,11,[25], [26], [27], [28]] were reviewed and analysed to determine whether SARS-CoV-2 could be transported from an infected mother to her neonate via vertical transmission (Table 1 ). The mean age of the pregnant females was 30.9 ± 2 years (95% CI, 29- 33). They gave birth by normal vaginal delivery 21% (12 cases, 95% CI: 10 – 32%) or Caesarean section (CS) 79% (45 cases, 95% CI: 68 – 90%) and all were COVID-19 positive. Seven females (12%) (95% CI: 4 – 29%) experienced premature rupture of membranes. The average gestational age (GA) was 37 + 4 days ±2 (95% CI: 34 – 41). Neonatal outcome was as follows: the average birth weight was 3,031 g (95% CI, 2,579 – 3,483). Prematurity was estimated to be 28 % (16 cases, 95% CI: 16 – 40%). Apgar scores were 8-9 in 1 minute, and 9 -10 in 5 minutes. The neonates clinical picture varied from intrauterine fetal distress 17% (10 cases, 95% CI: 7 – 27%), shortness of breath (SOB) 19 % (11 cases, 95% CI: 9 - 29%), gastrointestinal symptoms 14% (8 cases, 95% CI: 5 – 23%), and fever 8% (5 cases, 95% CI: 1 – 15%). One neonate died from multiorgan failure and DIC. Four neonates tested positive for COVID19 (6.8%) (95% CI: 0 – 9%). The affected neonates were all males and delivered by caesarean section.
Table 1.
Epidemiological and clinical outcomes of neonates born to COVID-19 mothers.
| Zhu et al. 2020 [25] | Khan et al. 2020 [11] | Li et al. 2020 [10] |
Fan et al. 2020 [26] | Wang et al. 2020 [27] | Zeng et al. 2020 [27] | |
|---|---|---|---|---|---|---|
| Demographic data | ||||||
| Number of newborn (twins) | 10 (2) | 3 (0) | 9 (0) | 2 (0) | 1 case report | 33 |
| Study time | 20 Jan 2020 to 05 Feb 2020 | 28 Jan 2020 to 1 March 2020 | 20 Jan 2020 to 31 Jan 2020 | 30 Jan 2020, 31 Jan 2020 | 1 Feb 2020 | |
| Country | China | China | China | China | China | China |
| Province | Hubei | Hubei, Wuhan | Hubei, Wuhan | Hubei, Wuhan | Hubei, Wuhan | Hubei, Wuhan |
| Maternal and Child Health Hospital | Renmin hospital | Zhongnan Hospital | Renmin Hospital | Tongji Hospital | fromWuhan Children's Hospital | |
| Maternal | ||||||
| Average age (Years) | 30 | 29.3 | 29.8 | 31.5 | 34 | |
| MOD | ||||||
| CS | 7/9 (77.8%) | 0/3 (0%) | 9/9 (100%) | 2/2 (100%) | CS | 26 (79%) |
| NVD | 2 (22.2%) | 3 (100%) | 0 (0%) | 0 (0%) | 7 (21%) | |
| Positive COVID-19 screening in the mother Nasopharyngeal/throat swab | 9 (100%) | 3 (100%) | 9 (100%) | 2 (100%) | 1 (100%) | 33 (100%) |
| Premature ROM | 3 (33.3%) | No | 1 (11.1%) | No | No | 3 (9%) |
| Neonate | ||||||
| Male | 8 (80%) | NA | NA | NA | 1 (100%) | 19 (57.5) |
| GA (Average) | 35 + 2 days | 37 + 3 days | 37 + 3 days | 40 | ||
| Birth weight, range, (Median) Kg | 1520 – 3800 (2,423) | 2890- 3730 (3,373) | 1880 – 3820(3011) | 2890 – 3400 (3145) | 3205 | |
| SGA | 2 (20%) | 0 (0 %) | 2/9 (22.2%) | 0/2 (0%) | No | 3 (9%) |
| Prematurity | 6 (60%) | 1 (33.3%) | 4 (44.4%) | 1 (50%) | No | 4 (12%) |
| Apgar score (average) | ||||||
| 1 min | 8.6 | 8.7 | 8.6 | 9 | 8 | |
| 5 min | 9.4 | 9.6 | 9.7 | 10 | 9 | |
| Clinical picture | ||||||
| SOB | 6/10 (60%) | No | No | 1/2 (50%) | No | 4 (12%) |
| Fever | 2/10 (20%) | No | No | 1/2 (50%) | No | 2 (6%) |
| Tachycardia | 1/10 (10%) | No | No | No | Yes | |
| GIT symptoms | 4/10 (10%) | No | No | 1/2 (50%) | Yes | 3 (9%) |
| Intrauterine Fetal distress | 6/10 (60%) | No | 2/9 (22.2%) | No | No | 2 (6%) |
| Chest-radiograph abnormality | 7/10 (70%) | NA | NA | 2/2 (100%) | yes | 3 (9%) |
| Laboratory | ||||||
| Thrombocytopenia | 2/10 (20%) | NA | NA | |||
| Lymphopenia | 1/7 (14%) | NA | NA | 2/2 (100%) | yes | 1 (3%) |
| Abnormal LFT | 2/10 (20%) | NA | NA | NA | AST (H) | No |
| T.Bil (μmol/l) | - | NA | NA | NA | 33 (H) | |
| D.Bil (μmol/l) | - | NA | NA | NA | 26 (H) | |
| CK (U/L) | NA | NA | NA | NA | 479 (H) | |
| COVID-19 screening in different samples | ||||||
| nasopharyngeal/throat swab | Negative 10/10 (100%) | Negative 3/3 (100%) | Negative 9/9 (100%) | Negative 2/2 (100%) | Positive | Positive 3/33 (9%) |
| Breast milk | NA | NA | Negative 9/9 (100%) | Negative 2/2 (100%) |
NA | NA |
| Amniotic fluid | NA | NA | Negative 9/9 (100%) | Negative 2/2 (100%) | NA | NA |
| Cord blood | NA | NA | Negative 9/9 (100%) | Negative 2/2 (100%) | Negative | NA |
| Placenta | NA | NA | NA | Negative 2/2 (100%) | Negative | NA |
| Vaginal swab | NA | NA | NA | Negative 2/2 (100%) | NA | NA |
| Neonatal Death | 1/10 (1%) | 0/3 (0%) | 0/9 (0%) | 0/2 (0%) | 0 % | NA |
Abbreviations: MOD, mode of Delivery; CS, caesarean section; NVD, normal vaginal delivery; GA, gestational age; ROM, rupture of membranes; SGA, small for gestational age; SOB, shortness of breath; GIT, gastrointestinal; T.Bil, total bilirubin; LFT, liver function tests; D.Bil, direct bilirubin; (H), high; NA, not available.
3.2. COVID-19 infection in children and neonates
Eleven studies were reviewed and analysed to investigate the incidence, clinical picture and laboratory finding of children and neonates with COVID 19 disease (Table 2 ).
Table 2.
Epidemiological and clinical data of COVID-19 positive children and neonates.
| Cai et al. 2020 [14] | Wei et al. 2020 [29] | Liu et al. 2020 [33] | Su et al. 2020 [5] | |
|---|---|---|---|---|
| Demographics | ||||
| N= | 10 | 9 | 6 | 9 |
| Period | 19 Jan 2020– 3 Feb 2020 | 8 Dec 2019 – 6 Feb 2020 | 7 Jan – 15 Jan 2020 | 24 Jan 2020 to 24 Feb 2020 |
| Country | China | China | China | China |
| Province | Anhui and Qingdao | Hubei, Wuhan | Shandong | |
| Age (range), Median | (3 m -11 y) | (1 – 11 m) | (1 – 7 y) | (11 mo – 9 yrs) |
| 6.5 y | 7 m | 3y | 5.5 y | |
| Gender, Male | 4/10 (40%) | 2/9 (22.2%) | 2/6 (33.3%) | 3/9 (33.3%) |
| Clinical picture | ||||
| Fever | 8/10 (80%) | 4/9 (44.4%) | 6/6 (100%) | 2/9 (22%) |
| Temperature | 37 - 39.2 | >39 C° | Afebrile – 38.5 C° | |
| 38.3 C° | ||||
| Cough | 6/10 (60%) | 1/9 (11%) | 6/6 (100%) | 1/9 (11%) |
| Sneezing | 2/10 (20%) | 0/9 (0%) | 0/6 (0%) | 0/9 (0%) |
| Stuffy nose | 3/10 (30%) | 0/9 (0%) | 0/6 (0%) | 0/9 (0%) |
| Rhinorrhoea | 2/10 (20%) | 1/9 (11 %) | 0/6 (0%) | 0/9 (0%) |
| Sore throat | 4/10 (40%) | 0/9 (0%) | 0/6 (%0) | 0/9 (0%) |
| Dyspnoea | 0/10 (0%) | 0/9 (0%) | 6/6 (100%) | 0/9 (0%) |
| Diarrhoea | 0/10 (0%) | 0/9 (0%) | 0/6 (0%) | 0/9 (0%) |
| ICU admission | 0/10 (0%) | 0/9 (0%) | 1/6 (16.6%) | 0/9 (0%) |
| Nausea/vomiting | 0/10 (0%) | 0/9 (0%) | 0/6 (0%) | 0/9 (0%) |
| fatigue | 0/10 (0%) | 0/9 (0%) | 0/6 (0%) | 0/9 (0%) |
| Pneumonia | 4/10 (40%) | 0/9 (0%) | 4/6 (66.6%) | 1/9 (11.1%) |
| complications | 0/10 (0%) | 0/9 (0%) | 0/6 (0%) | 0/9 (0%) |
| Laboratory | ||||
| leucopenia | 1/10 (10%) | NA | 4/6 (33.3%) | 2/9 (22.2%) |
| lecocytosis | 3/10 (30%) | NA | 0/6 (0%) | 1/9 (11.1%) |
| Neutrophilia | 1/10 (10%) | NA | 0/6 (0%) | 0/9 (0%) |
| Neutropenia | 3/10 (30%) | NA | 3/6 (50%) | 1/9 (11.1%) |
| Lymphopenia | 0/10 (0%) | NA | 6/6 (100%) | 0/9 (0%) |
| lymphocytosis | 1/10 (10%) | NA | 0/6 (0%) | 1/9 (11.1%) |
| Hemoglobin (g/dL) | (11.3 – 15.2) | NA | NA | 10.6 - 14 |
| 13 | 12 | |||
| thrombocytopenia | 1/10 (10%) | NA | NA | 1/9 (11.1%) |
| ALT | (18.5 – 100) | NA | NA | 9 to 22 |
| (U/L) | 7.7 | 14 | ||
| AST | (19.7 – 142) | NA | NA | 23 - 42 |
| (U/L) | 27.75 | 33 | ||
| C-reactive protein (mg/L) (range), median | (0.5 – 35) | NA | NA | 0.12 - 0.35 |
| 7.5 | NA | 0.19 | ||
| Procalcitonine, (range), median, ng/dl | 0.02 - 0.12 0.07 |
NA | NA | 0.02 - 0.08 0.04 |
| Lactate dehydrogenase (U/L) (range), median | (161 – 394) 254 |
NA | NA | |
| D-dimer (μg/mL) (range), median | (0.2 – 0.6) 0.45 |
NA | NA | - 0.4) 0.03 |
| Urea (mmol/L), (range), median | (0.5 – 4.1) 3.1 |
NA | NA | Normal |
| Creatinine | (13 – 58.9) | NA | NA | Normal |
| (μmol/L) | 35.5 | |||
| Creatine Kinase (U/L), (range), median | (12 - 42.3) 23 |
NA | NA | NA |
| CK-MB (U/L), (range), median | NA | NA | NA | (22 – 76) 30 |
| COVID-19 samples | ||||
| Nasopharyngeal/ | Positive 10/10 | Positive | Positive | positive |
| throat swab | 100% | 9/9 (100%) | 6/6 (100%) | 9/9 (100%) |
| Stool | Positive 5/6 | NA | NA | NA |
| 83.30% | ||||
| Urine | Positive 0/6 | NA | NA | NA |
| 0% | ||||
| Serum | Positive 0/6 | NA | NA | NA |
| 0% | ||||
| Ji et al., 2020 [35] | Sun et al. 2020 [34] | Xia et al. [20] | |
|---|---|---|---|
| Demographics | |||
| N= | 2 | 8 | 20 |
| period | 25 Jan – 3 Feb | 24 Jan - 24 Feb | 23 Jan - 8 Feb 2020 |
| Country | China | China | China |
| Province | Zhejiang | Wuhan | Wuhan |
| Age (range), Median | (9 – 15 y) | (2 m – 15 y) | 1 d - 14 y,7m |
| 12 y | 10 y, 9.5 m | 2 y, 1.5 m | |
| Gender | Male 2/2 (100%) | 6/8 (75%) | male 13 (65%) |
| Clinical picture | |||
| Fever | 1/2 (50%) | 6/8 (75%) | 12/20 (60%) |
| Temperature | 37.9 C° | ||
| Cough | 0 / 2 (0%) | 6/8 (75%) | 13/20 (65%) |
| Sneezing | 0 /2 | 0/8 (0%) | |
| Stuffy nose | 0 / 2 (0%) | 0/ 100 (0%) | |
| Rhinorrhoea | 0/2 (0%) | 0/8 (0%) | 3/20 (15%) |
| Sore throat | 1/2 (50%) | 0/ 100 (0%) | 1 (5%) |
| Dyspnoea | 0/20% | 7/8 (100%) | |
| Diarrhoea | 1/2 (50%) | 3/8 (37.5%) | 3/20 (15%) |
| ICU admission | 0/2 (0%) | 8/8 (100%) | |
| Nausea/vomiting | 4/8 (50%) | 2/20 (10%) | |
| fatigue | 1/8 (12.5%) | 1/20 (5%) | |
| Pneumonia | 0/2 (0%) | 8/8 (100%) | 20/20 (100%) |
| complications | 0/2 (0% | 4/8 (50%) | yes |
| Laboratory | |||
| leucopenia | 1/8 (12.5%) | 4/12 (5%) | |
| lecocytosis | 1/2 (50%) | 2/20 (10%) | |
| Neutrophilia | 0/2 (0%) | 1/8 (12.5%) | |
| Neutropenia | 0/2 (0%) | 1/8 (12.5%) | |
| Lymphopenia | 0/2 (0%) | 1/8 (12.5%) | 7/20 (35%) |
| lymphocytosis | 0/2 (0%) | 0/8 (0%) | 3/20 (15%) |
| Hemoglobin (g/dL) | NA | Anemia 3/8 (37.5%) | |
| thrombocytopenia | NA | 1/8 (12.5%) | |
| ALT (U/L) (range), median | NA | (8 – 100) 45 |
increased in 5/20 (25%) |
| AST (U/L), (range), median | NA | (14 – 410) 21.5 |
|
| C-reactive protein (mg/L), (range), median | 3.49 – 34.64 19.06 |
(0.5 – 103) 8.19 |
high in 7/20 35% |
| Procalcitonine (ng/dl), (range), median | NA | (0.04 - 17.6) 0.085 |
high in 16/20 (80%) |
| Lactate dehydrogenase (U/L), (range), median | NA | (187 – 891) 382 |
NA |
| D-dimer (μg/mL), (range), median | NA | (0.23 - 40.43) (0.455) |
NA |
| Creatinine, (μmol/L), (range), median | NA | (15 - 72.1) 35.25 |
NA |
| Creatine Kinase (U/L) | NA | 15 – 20702 (91.5) | NA |
| CK-MB (U/L) | NA | NA | high in 5/20 (25%) |
| COVID-19 samples | |||
| Nasopharyngeal/ | Positive 2/2 | Positive | positive 20/20 |
| throat swab | 100% | 8/8 (100%) | 100% |
| stool | NA | NA | NA |
| Urine | NA | NA | NA |
| Serum | NA | NA | NA |
| Li et et al. 2020 [31] | Xu et al. 2020 [13] | Lu et al. 2020 [32] | Kam et al. 2020 [30] | |
|---|---|---|---|---|
| Demographics | ||||
| N= | 5 | 10 | 171 | case report |
| period | 28 jan - 8 Feb 2020 | 28 Jan - 26 Feb 2020 | ||
| Country | China | China | China | Simgapore |
| Province | Guangdong | |||
| Age (range), Median | 10 m - 6 y | 2 m - 15.5 y | 1 d- 15 y | 6 M |
| 3 y, 8 m | 7 y | 6.7 y | ||
| Gender | 4/5 (80%) | Male 6/10 (60%) |
Male 104/171 (60.8%) | Male |
| Fever | 1/5 (20%) | 7/10 (70%) |
71/171 (41.5%) | no |
| Temperature | 37.8 - 39.1 38.5 |
|||
| Cough | 1/5 (20%) | 5/10 (50%) |
83/171 (48.5%) | no |
| Stuffy nose | 2/10 (20%) |
no | ||
| Rhinorrhoea | 1/5 (20%) | 2/10 (20%) |
13/171 (7.6%) | no |
| Sore throat | 1/5 (20%) | 4/10 (40%) |
no | |
| Diarrhoea | 3/10 (30%) |
15/171 (8.8%) | no | |
| ICU admission | 0/5 (0%) | no | ||
| Nausea/vomiting | 11/171 (6.4%) | no | ||
| fatigue | 13/171 (7.6%) | no | ||
| Pneumonia | 3/5 (60%) | 0/10 (0%) | 111/171 (65%) | no |
| complications | 0% | 0% | no | |
| Laboratory | ||||
| leucopenia | 3/10 (30%) | NA | no | |
| lecocytosis | 2/5 (40%) | NA | no | |
| Neutrophilia | 1/10 (10%) | NA | no | |
| Neutropenia | NA | yes | ||
| Lymphopenia | 3/10 (30%) | NA | ||
| lymphocytosis | ||||
| Haemoglobin (g/dL) | NA | (10.2 - 16.3) 12.4 |
NA | Normal |
| thrombocytopenia | NA | 0% | NA | no |
| ALT (U/L), (range), median | NA | (6 – 172) 17 |
NA | Normal |
| AST (U/L), (range), median | (16 – 127) 23 |
NA | Normal | |
| C-reactive protein (mg/L), (range), median | 1 (20%) | (0.3 - 22.03) 1.14 |
NA | NA |
| Procalcitonine (ng/dl), | NA | slighly increased in 5 patients | NA | NA |
| Lactate dehydrogenase (U/L) | NA | (138 – 378) 217 |
NA | NA |
| D-dimer (μg/mL), (range), median | NA | (0.23 - 0.84) 0.32 |
NA | NA |
| Urea (mmol/L) | NA | normal | NA | NA |
| COVID-19 samples | ||||
| Nasopharyngeal/ | positive 5/5 | positive 10/10 | positive (171/171) | positive |
| throat swab | 100% | 100% | 100% | |
| stool | NA | positive | NA | positive |
| 8/10 (80%) | ||||
| Urine | NA | NA | NA | Negative |
| Serum | NA | NA | NA | Negative |
Abbreviations: ICU, intensive care unit; ALT; alanine aminotransferase; AST, aspartate aminotransferase; CK-MB, creatine kinase myocardial band; NA, not available.
(4,5,13,14,20,29–35).
The median age was 6.5 years (0-12 years). Among those patients, males were 59% (147 cases, 95% CI: 53-65%) and females were 41% (104 cases, 95% CI: 35 – 47%). There was no statistically significant difference between males and females (p = 0.7).
Most of patients presented with either cough 49% (122 cases, 95% CI: 42 – 55%) or fever 47% (118 cases, 95% CI: 41- 53%). Some children presented with sore throat 36% (90 patients, 95% CI: 30 – 42%); gastrointestinal (GIT) symptoms in the form of vomiting or diarrhoea were present in 17% (42 cases, 95% CI: 12 – 21%). Other symptoms include a rhinorrhoea 9% (22 cases, 95% CI: 5 – 12%) and a few cases presented with sneezing and fatigue. Pneumonia was recorded in 60% (151 cases, 95% CI: 54 – 66%). However, many studies have recorded that most of the children present with mild pneumonia which could be unilateral or bilateral [13,14]. The majority of the cases had mild disease, with only 4% (9 cases - 95% CI: 1 – 6%) were admitted to the ICU. The case fatality rate was 0%.
According to laboratory findings, full blood count showed the following: Leucopenia and leucocytosis were present in 19% (15 cases, 95% CI: 10 – 27%) and 11% (9 cases, 95% CI: 4 – 18%) respectively. Lymphopenia and lymphocytosis were present in 21% (17 cases, 95% CI: 12 – 30%) and 5% (4 cases, 95% CI: 0 – 10%) respectively; thrombocytopenia was found in only 4% (3 cases, 95% CI: 0 – 8%). Raised C-reactive protein concentrations were present in 28% (22 cases, 95% CI: 18 – 37%). Procalcitonin (PCT) concentrations were raised in 28% (22 cases, 95% CI: 18 – 37%). Raised transaminase and lactate dehydrogenase activities were demonstrated in 13% (10 cases, 95% CI: 5 – 20%) and 5% (4 cases, 95% CI: 0 – 10%) respectively.
Su et al. and Sun et al. [5,34] analysed circulating cytokine concentrations, as well as those of lymphocyte surface markers. CD4+ was raised in 6 out of 15 patients (95% CI: 15 – 65%). Concentrations of the pro-inflammatory cytokines IL-6 and IFN-γ were increased in two patients (13%) and concentrations of the anti-inflammatory IL-10 were raised in 33% (5 patients, 95% CI: 9 – 57%).
4. Discussion
4.1. COVID-19 prevalence in Paediatric age group
A large case series was published by The Chinese Center for Disease Control and Prevention; this study included 72,314 cases which were classified as either confirmed, suspected, clinically diagnosed cases, or asymptomatic cases. Amongst the confirmed cases group, there were 416 (0.93%) less than 10 years old and 549 (1.2%) aged between 10 and 19 years old; the case fatality rate in children younger than 9 years old was 0% [1]. However, on the 31st of March 2020, a child aged 13 years old was the first UK death from COVID-19 at this age, the child died at London Hospital trust but no details are available (BBC news,2020). On the same day, 13-Year-Old-Belgian girl died with COVID-19 (Euro news, 2020).
A study in China reviewed all affected infants under one-year-old in the period between 6 December 2019 and 8 February 2020 [29]. They found that only nine infants were affected. This figure reflects the rarity of COVID-19 in infants. Additionally, all cases were mild enough so that none of them required intensive care admission, mechanical ventilation nor developed complications.
There are many factors that could explain why SARS-Cov-2 is not primarily a disease with large consequences for paediatric populations. Firstly, it could be explained by the distribution of ACE2 receptors in fetal lung compared to adult lung tissue. Hoffmann et al. in their study inoculated different cell lines with pseudo-particles harbouring SARS-CoV-2 glycoprotein then measured the luciferase activity; it was shown that Calu-3 cells (adult human lung adenocarcinoma cells) demonstrated higher luciferase activity 105.5 cps compared to MRC-5 cells (human fetal lung cells) with 102 cps [6]. This finding infers that foetal lung ACE2 receptors have different characteristics than mature lung tissue (e.g. lower binding capacity). Secondly, the children are exposed to other respiratory viruses such as respiratory syncytial virus, Influenza A and Influenza B viruses, which enhance their serum antibody levels and could provide cross protection [4]. Children’s immune system is not fully mature and they respond to infections in a manner different from adult’s response. Finally, it is worth mentioning that the actual number of COVID-19 in children may be higher than the published figures. Nonetheless, due to the mild symptoms or even asymptomatic cases, it may be underdiagnosed. Widening the screening scale may pick up larger number of childhood cases.
4.2. COVID-19 disease characteristics in neonates and children
The incubation period for the SARS-CoV-2 ranges between 2 – 14 days [7]. Nonetheless, this incubation period varies according to disease severity [36]. No age is immune against COVID-19 infection; nevertheless, elderly people, pregnant females and those with impaired immunity are liable to more sever disease sequelae than the paediatric age group [37].
Childhood COVID-19 disease usually runs a mild course. The children can be a symptomatic or present with cough, fever and fatigue. Some studies have reported low grade fever or even no fever at all [14,35]. This is usually accompanied by upper respiratory tract symptoms like nasal congestion and headache [7]. The affected children can also present with gastrointestinal manifestations such as diarrhoea, vomiting or abdominal distension [35]. The disease has good prognosis in children with most of the cases are recovered after a mild disease course and it is very uncommon to progress to severe lower respiratory disease [38]. Data from adult patients showed that they can develop difficulty breathing one week after the initial symptoms which can progress to severe acute respiratory distress syndrome, respiratory failure, septic shock, metabolic acidosis and coagulopathy [7]. However, this trajectory is extremely rare in children [38]. Sun et al. [34] described eight critically/severely ill patients who were admitted to the ICU. One patient had underlying immuno-suppression from acute lymphoblastic leukaemia which made him more susceptible to critical COVID19 disease. In this study four patients developed complications in the form of septic shock, multi organ system failure, kidney stones, hydronephrosis, coagulopathy, DIC, intussusception, status epilepticus, and hypoglobulinemia.
A ten-month old female developed encephalopathy and her circulating cytokines were high as a complication of COVID-19 infection [34]. Additionally, One study reported a case of Acute necrotizing encephalopathy (ANE) in an adult female patient with COVID-19 [39]. ANE is a rare complication of influenza and other viral respiratory infections and has been related to intracranial cytokine storms, which result in blood-brain-barrier breakdown [40]. SARS-CoV-2 seems to behave like these respiratory viruses as reported in the adult and infant cases.
Dong et al. performed a retrospective study of 2,141 paediatric patients with confirmed or suspected to have COVID-19 in China. They found that most of the patients (1,091 - 50.9%) had mild illness, whereas 831 (38.8%) of the children had moderate disease. This means that about 90% of the children in this study had a mild or moderate disease. Only 13 (0.6%) patients were critically ill and most of them (7 – 0.3%) were infants (53.8%). This study elucidated that childhood illness is generally not severe and that children less than one-year-old are the most vulnerable group to critical illness and ICU admission [4]. Moreover, this study pooled the data of disease severity amongst suspected and confirmed cases, this means that the 0.6% who showed critical illness could have a respiratory disease other than COVID-19 e.g.: RSV, influenza virus type A or B.
4.3. Vertical transmission of COVID-19
Studies done so far revealed that vertical transmission of COVID19 is yet to be established either by normal vaginal delivery or caesarean section [[10], [11], [12],[25], [26], [27]]. Several studies have investigated vertical transmission of COVID-19 via examining the throat swab of the newborns of COVID-19 positive pregnant women who underwent caesarean section [10,11,25,26]. Additionally, Chen et al. [10] examined the amniotic fluid, cord blood and the first breast milk after delivery. All samples tested negative for COVID-19. Other studies investigated the possibility of vertical transmission via vaginal delivery, they found that all tested neonates had negative throat swab [11,25,27]. However, a recently published study [12] investigated the possibility of COVID-19 vertical transmission via screening all neonates (n = 33) born to confirmed COVID-19 mothers, 3 neonates (9%) experienced positive nasopharyngeal and throat swabs of COVID-19, this means that the possibility of vertical transmission cannot be precluded. The limitation of these studies are: 1) the small sample size; 2) maternal infection occurred at the third trimester of pregnancy, so little is known about the possibility of neonatal affection in the first or second trimesters. So, further studies are required.
The clinical picture of neonates born to COVID19 positive mothers was variable and included mainly fever, upper respiratory tract symptoms and gastrointestinal symptoms. Premature birth was present in 50% of the reviewed studies. This prematurity may be explained by COVID-19 induced hypoxemia or may be attributed to other factors such as the preeclampsia, premature rupture of membranes, history of previous CS or still birth[10,25]. Neonatal death was reported in only one case born to COVID-19 positive mother. This child had thrombocytopenia, impaired coagulation profile and elevated level of transaminases. He developed multiorgan failure and DIC to which he received packed RBCs, platelets and plasma transfusion, but he did not respond to the treatment and eventually died at the age of 9 days. The cause of death is not clear, it may be related to poor neonatal immunity, high maternal viral load or severe maternal clinical picture.
One study reported a neonate with positive COVID-19 born to a mother with confirmed COVID-19. However, considering this as a vertical transmission is controversial. First, the sample was taken 36 hours after delivery, so the child could be infected by direct contact [27]. Secondly, both cord blood and placenta samples were tested negative for SARS-CoV-2. On the other hand, vertical transmission could not be ruled out completely as the negative screening in the cord blood and placenta can be attributed to low viral load at the time of delivery that was below the detection limit of the PCR. So, further studies are needed.
4.4. COVID-19 and breast feeding
Whether breast milk feeding is prohibited in COVID-19 confirmed lactating women is yet to be established. Nevertheless, two studies examined breast milk in COVID19 positive females and the milk was tested negative [10,26]. This indicates that the virus is not transmitted to breast milk and that breast milk feeding may be safe in this situation, although further studies with larger sample sizes are needed to prove this.
5. Conclusion
Paediatric age group are liable to infection by COVID-19. However, the disease usually has a mild course with fever and cough are the most frequently observed symptoms. Intensive care unit and death are extremely rare. Vertical transmission and virus shedding in breast milk are yet to be established.
Funding
This study did not require fund.
Declaration of Competing Interest
The authors have indicated that they have no conflicts of interest to disclose.
Websites
WHO website: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200401-sitrep-72-covid-19.pdf?sfvrsn=3dd8971b_2. Accessed 04/04/2020 1:25 am.
BBC news website: https://www.bbc.co.uk/news/uk-52114476. Accessed 02/04/2020 at 12:30 am
Euro news website: https://www.euronews.com/2020/03/31/coronavirus-doctors-devastated-as-covid-19-claims-life-of-12-year-old-girl-in-belgium. Accessed 02/04/2020 at 12:32 am
CRediT authorship contribution statement
Naira M Mustafa: Conceptualization, Methodology, Software, Data curation, Visualization, Writing - review & editing. Laila A Selim: Conceptualization, Supervision, Writing - review & editing.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jcv.2020.104395.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Wu Zunyou, McGoogan Jennifer M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Neuman Benjamin W., Buchmeier Michael J. vol. 96. Academic Press; 2016. Supramolecular architecture of the coronavirus particle; pp. 1–27. (Advances in virus research). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jombart Thibaut, Zandvoort Kevin van, Russell Tim, Jarvis Christopher, Gimma Amy, Abbott Sam, Clifford Samuel. Inferring the number of COVID-19 cases from recently reported deaths. medRxiv. 2020 doi: 10.1101/2020.03.10.20033761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong Yuanyuan, Mo Xi, Hu Yabin, Qi Xin, Jiang Fang, Jiang Zhongyi, Tong Shilu. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. [DOI] [Google Scholar]
- 5.Su Liang, Ma Xiang, Yu Huafeng, Zhang Zhaohua, Bian Pengfei, Han Yuling, Sun Jing. The different clinical characteristics of corona virus disease cases between children and their families in China–the character of children with COVID-19. Emerging Microbes & Infections. 2020;9(1):707–713. doi: 10.1080/22221751.2020.1744483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., Müller M.A. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020 doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Zhi-Min, Fu Jun-Fen, Shu Qiang, Chen Ying-Hu, Hua Chun-Zhen, Li Fu-Bang, Lin Ru. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World journal of pediatrics. 2020:1–7. doi: 10.1007/s12519-020-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Doremalen Neeltje, Bushmaker Trenton, Morris Dylan H., Holbrook Myndi G., Gamble Amandine, Williamson Brandi N., Tamin Azaibi. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothan Hussin A., Byrareddy Siddappa N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. 2020 doi: 10.1016/j.jaut.2020.102433. 102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Yang, Zhao Ruihong, Zheng Shufa, Chen Xu, Wang Jinxi, Sheng Xiaoli, Zhou Jianying. Lack of Vertical Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, China. Emerging infectious diseases. 2020;26(6) doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan Suliman, Peng Liangyu, Siddique Rabeea, Nabi Ghulam, Xue Mengzhou, Liu Jianbo, Han Guang. Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infection Control & Hospital Epidemiology. 2020:1–9. doi: 10.1017/ice.2020.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeng Lingkong, Xia Shiwen, Yuan Wenhao, Yan Kai, Xiao Feifan, Shao Jianbo, Zhou Wenhao. Neonatal Early-Onset Infection With SARS-CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan. China." JAMA pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu Yi, Li Xufang, Zhu Bing, Liang Huiying, Fang Chunxiao, Yu Gong Qiaozhi Guo. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nature Medicine. 2020:1–4. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cai Jiehao, Xu Jing, Lin Daojiong, Xu Lei, Qu Zhenghai, Zhang Yuehua, Zhang Hua. A Case Series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Zhixin, Xiao Xiao., Wei Xiuli, Li Jian, Yang Jing, Tan Huabing, Zhu Jianyong, Zhang Qiwei, Wu Jianguo, Liu Long. Composition and divergence of coronavirus spike proteins and host ACE2 receptors predict potential intermediate hosts of SARS‐CoV‐2. Journal of medical virology. 2020 doi: 10.1002/jmv.25726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagata Noriyo, Iwata Naoko, Hasegawa Hideki, Fukushi Shuetsu, Yokoyama Masaru, Harashima Ayako, Sato Yuko, Saijo Masayuki, Morikawa Shigeru, Sata Tetsutaro. Participation of both host and virus factors in induction of severe acute respiratory syndrome (SARS) in F344 rats infected with SARS coronavirus. Journal of virology. 2007;81(4):1848–1857. doi: 10.1128/JVI.01967-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Fang, Li Wenhui, Farzan Michael, Harrison Stephen C. Structure of SARS coronavirus spike receptor-binding domain complexed with receptor. Science. 2005;309(5742):1864–1868. doi: 10.1126/science.1116480. [DOI] [PubMed] [Google Scholar]
- 18.Kanne Jeffrey P., Little Brent P., Chung Jonathan H., Elicker Brett M., Ketai Loren H. 2020. Essentials for radiologists on COVID-19: an update—radiology scientific expert panel. 200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mossa-Basha Mahmud, Meltzer Carolyn C., Kim Danny C., Tuite Michael J., Pallav Kolli K., Tan Bien Soo. Radiology Department Preparedness for COVID-19: Radiology Scientific Expert Panel. Radiology. 2020 doi: 10.1148/radiol.2020200988. 200988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xia Wei, Shao Jianbo, Yu Guo Xuehua Peng, Li Zhen, Hu Daoyu. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatric pulmonology. 2020 doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ianniello Stefania, Piccolo Claudia Lucia, Buquicchio Grazia L., Trinci Margherita, Miele Vittorio. First-line diagnosis of paediatric pneumonia in emergency: lung ultrasound (LUS) in addition to chest-X-ray (CXR) and its role in follow-up. The British journal of radiology. 2016;89(1061) doi: 10.1259/bjr.20150998. 20150998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng Q.Y., Wang X.T., Zhang L.N., Critical C., Ultrasound C., Group S. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019 – 2020 epidemic. Intensive Care Med. 2020:6–7. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rodrigues J.C.L., Hare S.S., Edey A., Devaraj A., Jacob J., Johnstone A., McStay R., Nair A., Robinson G. An update on COVID-19 for the radiologist-A British society of Thoracic Imaging statement. Clinical Radiology. 2020 doi: 10.1016/j.crad.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kanne Jeffrey P., Little Brent P., Chung Jonathan H., Elicker Brett M., Ketai Loren H. 2020. Essentials for radiologists on COVID-19: an update—radiology scientific expert panel. 200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu Huaping, Wang Lin, Fang Chengzhi, Peng Sicong, Zhang Lianhong, Chang Guiping, Xia Shiwen, Zhou Wenhao. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Translational pediatrics. 2020;9(1):51. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fan Cuifang, Di Lei Congcong Fang, Li Chunyan, Wang Ming, Liu Yuling, Bao Yan. Perinatal Transmission of COVID-19 Associated SARS-CoV-2: Should We Worry? Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Shaoshuai, Guo Lili, Chen Ling, Liu Weiyong, Cao Yong, Zhang Jingyi, Feng Ling. A case report of neonatal COVID-19 infection in China. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeng Lingkong, Xia Shiwen, Yuan Wenhao, Yan Kai, Xiao Feifan, Shao Jianbo, Zhou Wenhao. Neonatal Early-Onset Infection With SARS-CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan, China. JAMA pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wei Min, Yuan Jingping, Yu Liu Tao Fu, Yu Xue, Zhang Zhi-Jiang. Novel coronavirus infection in hospitalized infants under 1 year of age in China. Jama. 2020 doi: 10.1001/jama.2020.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kam Kai-qian, Yung Chee Fu, Cui Lin, Tzer Raymond, Lin Pin, Mak Tze Minn, Maiwald Matthias, Li Jiahui. A Well Infant with Coronavirus Disease 2019 with High Viral Load. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Wei, Cui Huaqian, Li Kunwei, Fang Yijie, Li Shaolin. Chest computed tomography in children with COVID-19 respiratory infection. Pediatric radiology. 2020:1–4. doi: 10.1007/s00247-020-04656-04657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu Xiaoxia, Zhang Liqiong, Hui Du, Zhang Jingjing, Li Yuan Y., Jingyu Qu, Zhang Wenxin. SARS-CoV-2 infection in children. New England Journal of Medicine. 2020 doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Weiyong, Zhang Qi, Chen Junbo, Xiang Rong, Song Huijuan, Shu Sainan, Chen Ling. Detection of Covid-19 in children in early January 2020 in Wuhan, China. New England Journal of Medicine. 2020 doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sun Dan, Li Hui, Lu Xiao-Xia, Xiao Han, Ren Jie, Zhang Fu-Rong, Liu Zhi-Sheng. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World Journal of Pediatrics. 2020:1–9. doi: 10.1007/s12519-020-00354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ji Li-Na, Chao Shuang, Wang Yue-Jiao, Li Xue-Jun, Mu Xiang-Dong, Lin Ming-Gui, Jiang Rong-Meng. Clinical features of pediatric patients with COVID-19: a report of two family cluster cases. World Journal of Pediatrics. 2020:1–4. doi: 10.1007/s12519-020-00356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lauer Stephen A., Grantz Kyra H., Bi Qifang, Jones Forrest K., Zheng Qulu, Meredith Hannah R., Azman Andrew S., Reich Nicholas G., Lessler Justin. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Annals of internal medicine. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shen Kunling, Yang Yonghong, Wang Tianyou, Zhao Dongchi, Jiang Yi, Jin Runming, Zheng Yuejie. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts’ consensus statement. World journal of pediatrics. 2020:1–9. doi: 10.1007/s12519-020-00343-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hong Hao, Wang Yuan, Chung Hung-Tao, Chen Chih-Jung. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatrics & Neonatology. 2020 doi: 10.1016/j.pedneo.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Poyiadji Neo, Shahin Gassan, Noujaim Daniel, Stone Michael, Patel Suresh, Griffith Brent. COVID-19–associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI Features. Radiology. 2020 doi: 10.1148/radiol.2020201187. 201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Desforges Marc, Le Coupanec Alain, Dubeau Philippe, Bourgouin Andréanne, Lajoie Louise, Dubé Mathieu, Talbot Pierre J. Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses. 2020;12(1):14. doi: 10.3390/v12010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.