Abstract
In this unique historic period afflicted by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pandemic, radiation therapy treatments cannot be delayed or suspended. We report the case of a 73-year-old woman with recently diagnosed extensive-stage small cell lung cancer with metastatic liver and bone lesions. A SARS-CoV-2 test was performed upon hospital admission and was negative. After 5 days she underwent radiation therapy on T6 and T11 with single fractions of 8 Gy each. Before treatment a cone beam computed tomography (CBCT) scan was performed to check the setup of the patient. Some suspected lung areas of ground glass opacities (GGOs) were clearly visible in the CBCT without any counterpart in the previous computed tomography (CT) simulation scan 3 days before. A new high-quality chest CT scan confirmed the previously suspected GGOs. The exam revealed multiple bilateral areas of subpleural GGOs, which are the primary findings on CT scan in the early phases of coronavirus disease 2019 (COVID-19) lung infection, in addition to pleural effusions, a finding that may occur as a complication of COVID-19. The patient then urgently repeated the SARS-CoV-2 test, which was positive and confirmed the infection. In conclusion, daily CBCT can be effective for early detection of COVID-19 lung disease in asymptomatic or mildly symptomatic patients.
Introduction
In this unique, historic period affected by a severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pandemic, radiation therapy (RT) treatments cannot be delayed or suspended. Several consensus papers regarding the delivery of RT in different settings and cancer histologies have been published on the topic of limiting the spread of coronavirus disease 2019 (COVID-19) infection in radiation oncology departments, suggesting that patients should be treated using hypofractionated schemes and that radical treatments should be prioritized over adjuvant treatments.1,2 The development of image guided radiation therapy during the last 2 decades has allowed radiation oncologists to fix any set-up error, to verify the target position, and even to perform adaptive RT, but it can also be useful to assess healthy lung tissue.3
Case Description
We report the case of a 73-year-old woman with recently diagnosed extensive-stage small cell lung cancer, with metastatic liver and bone lesions. In the oncological anamnesis she had right breast cancer 15 years before, treated with surgery and postoperative RT, plus 5 years of hormone therapy, with negative follow-up.
She was admitted to our hospital on March 21, 2020, to start systemic treatment and was then referred for RT for two pathologic vertebral lesions with an initial spread to the spinal canal. A SARS-CoV-2 test was performed at the hospital admission and was negative.
On March 23 the patient was sent to the radiation oncology department for computed tomography (CT) simulation to treat the bone lytic lesions affecting the bodies of the 6th and 11th thoracic vertebrae. She did not have neurologic symptoms, so she first started chemotherapy (carboplatin AUC5 + etoposide q3w) from March 23 to 25. On the 26th she underwent RT on T6 and T11 with single fractions of 8 Gy each. The treatment was delivered on a TrueBeam STX (v2.5), with a multiple field static intensity modulated radiation therapy technique. Before treatment a cone beam CT (CBCT) was performed to check the setup of the patient. The acquisition protocol used for CBCT imaging was half fan and full rotation (125 kV and 270 mAs), half bow-tie filter applied, and no iterative reconstruction applied.
The next day the radiation oncologist performed the offline review of treatment setup comparing the CBCT acquired in the RT treatment room with the CT simulation. Some suspected lung areas of ground glass opacities (GGOs) were clearly visible in the CBCT without any counterpart in the previous scan (Fig 1); after discussion with the radiologist, it was decided to perform a new chest CT scan that confirmed the previously suspected GGOs (Fig 2). In fact, the examination revealed multiple bilateral areas of subpleural GGOs, which are the primary findings on CT scan in the early phases of COVID-19 lung infection, and also pleural effusions, a finding that may occur as a complication of COVID-19. The patient then urgently repeated the SARS-CoV-2 test, which was positive and confirmed the infection. On March 28 she was transferred to the infective disease COVID-19 department, where she is still hospitalized as we write this article.
Figure 1.
Computed tomography (CT) simulation scan on March 23, 2020, (A1-A2) versus cone beam CT (CBCT) (B1-B2) acquired March 26, 2020, as registered before treatment delivery. Red arrows highlight the development of ground glass opacities (GGOs).
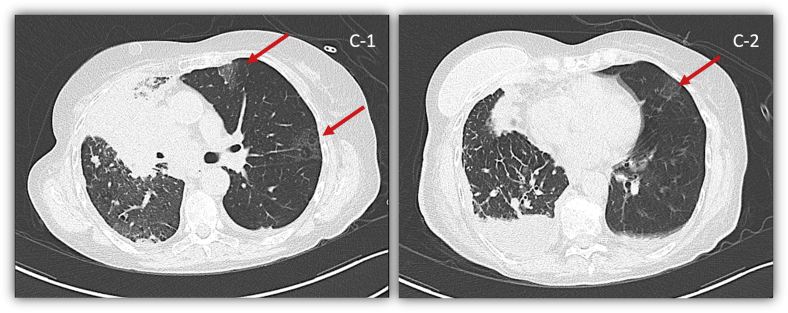
Figure 2.
Chest computed tomography (CT) scan (C1-C2) acquired on March 27, 2020. Red arrows confirm the presence of ground glass opacities (GGOs) correlated with the initial onset of coronavirus disease 2019 (COVID-19) pneumonitis.
Discussion
At the earliest stage of COVID-19 disease, a noncontrast chest CT scan has high sensitivity for the detection of GGOs in the SARS-CoV-2 infection,4 and this could justify its use in the early imaging in the acute phase in selected cases. This is relevant because early detection could improve patient outcome for COVID-related pneumonia, characterized by a release of proinflammatory cytokines followed by activation and production of active mediators of lung inflammation, fever, and fibrosis.5
During this pandemic COVID-19 infection, the role of hypofractionated RT has grown because of its advantages in reducing the spread of the disease by limiting patient access.1 In this setting, the routine use of CBCT allows radiation oncologists to perform customized treatments with higher dose per fraction.2 In an article soon to be published, the authors found that CBCT has the potential to detect early COVID-19 lung disease.6
In this case report the patient first had a negative SARS-CoV-2 test and took a second one after the appearance of GGOs on the CT scan, the day after RT, owing to findings on CBCT.
Conclusions
In conclusion, daily CBCT can be effective for early detection of COVID-19 lung disease in asymptomatic or mildly symptomatic patients, helping to prevent the diffusion of this contagious disease to the care providers and other patients in the radiation oncology department.
Footnotes
Sources of support: The authors received no financial support for the research, authorship, and publication of this article. This work was supported by Italian Ministry of Health (Ricerca Corrente 2020).
Disclosures: None of the authors has any conflict of interest with the published data.
References
- 1.National Institute for Health and Care Excellence; London: 2020. National Institute for Health and Care Excellence. COVID-19 Rapid Guideline. Delivery of Radiotherapy. NICE UK Guidelines [NG162] [Google Scholar]
- 2.Guckenberger M, Belka C, Bezjak A, et al. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus statement [epub ahead of print]. Radiother Oncol 2016. 10.1016/j.radonc.2020.04.001. Accessed June 4, 2020. [DOI] [PMC free article] [PubMed]
- 3.Duffton A., Harrow S., Lamb C. An assessment of cone beam CT in the adaptive radiotherapy planning process for non-small-cell lung cancer patients [epub ahead of print] Br J Radiol. 2016 doi: 10.1259/bjr.20150492. Accessed June 4, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases [epub ahead of print]. Radiology 2020. 10.1148/radiol.2020200642. Accessed June 4, 2020. [DOI] [PMC free article] [PubMed]
- 5.Huang G, Gong T, Wang G, et al. Timely diagnosis and treatment shortens the time to resolution of coronavirus disease (COVID-19) pneumonia and lowers the highest and last CT scores from sequential chest CT [epub ahead of print]. Am J Roentgenol 2020. 10.2214/AJR.20.23078. Accessed June 4, 2020. [DOI] [PubMed]
- 6.Suppli MH, de Blanck SR, Elgarrd T, Josipovic M, Pohl M. Early appearance of COVID-19 associated pulmonary infiltrates during daily radiotherapy imaging for lung cancer [epub ahead of print]. J Thoracic Oncol 2020. 10.1016/j.jtho.2020.04.004. Accessed June 4, 2020. [DOI] [PMC free article] [PubMed]