Abstract
Background
There is concern in Germany that the capacity of intensive care unit (ICU) beds may not be sufficient for the COVID-19 pandemic. The aim was to determine the maximum daily number of COVID-19 cases requiring intensive care from 11 April through 30 June 2020.
Methods
We assumed three non-exponential scenarios for the development of the cumulative case numbers up to 30 June 2020 (linear, slow quadratic, and fast quadratic). We assumed that 3–10% of of patients would require intensive care, that 8 days would elapse from a positive test to the need for intensive care, and that intensive care would be necessary for 14 or 20 days.
Results
Extrapolation of the maximum registered daily COVID-19 cases reveals a range of 4133 to 12 233 cases. Assuming that 3–10% of newly detected COVID-19 cases become intensive care patients and the average length of ICU stay is between 14 and 20 days, we arrive at a maximum daily number of ICU cases between 1989 (linear extrapolation, 3% ICU, 14 days in ICU) and 20 966 (fast quadratic extrapolation, 10% ICU, 20 days in ICU).
Discussion
Our results give no rise for concern that triage of COVID-19 patients may become necessary in Germany. However, the occupancy of ICU beds should be managed centrally to ensure optimal use of bed capacity. If, contrary to expectations, an exponential increase in case numbers should occur after all, our results will become invalid.
In the context of the current development of the SARS-CoV-2 pandemic in Germany, there is concern that the number of intensive care unit (ICU) beds in hospitals will not suffice for the COVID-19 case volume. Television companies have been broadcasting triage scenarios from Italy in which doctors have to decide which patients will be ventilated and which not. There is fear that when the pandemic reaches its peak in Germany, a similar triage situation will arise. Press headlines such as “RKI: not enough intensive care beds” [1] lead to anxiety and uncertainty in the population.
According to the intensive care registry maintained by the German Interdisciplinary Association for Intensive Care and Emergency Medicine (Deutsche Interdisciplinäre Vereinigung für Intensiv- und Notfallmedizin, DIVI), as of 9 April 2020 there were 16 734 intensive care beds at the 680 hospital sites that had supplied data to the registry, of which 9695 (58%) were occupied and 7038 (42%) were free. On the same day there were 1888 COVID-19 patients in ICUs, of whom 1464 (78%) were being ventilated [2]. The DIVI data from 17 April 2020 show a total of 2601 COVID-19 patients being treated in ICUs, with 73.7% receiving oxygenation or artificial ventilation [3].
The aim of this study was to determine the maximum numbers of COVID-19 cases requiring intensive care in the period 11 April to 30 June 2020 with different non-exponential extrapolations of the development in reported COVID-19 cases over time.
Material and methods
We extracted the cumulative number of laboratory-confirmed COVID-19 infections in Germany for the period 2 March 2020 to 10 April 2020 (4). Using the daily cumulative case numbers, we calculated the daily number of newly detected COVID-19 cases.
For the period 11 April to 30 June 2020, we assumed three different scenarios for the development of the cumulative case numbers, based on the cumulative number of 117 658 cases detected by 10 April 2020 and the 4133 new cases detected on 10 April 2020:
Linear growth of the cumulative case numbers
A slow quadratic increase in cumulative case numbers
A fast quadratic increase in cumulative case numbers
The quadratic extrapolation follows the formula f = a × i2+ (b + a) × i + 117 658, with f being the extrapolated cumulative number of COVID-19 cases, a being a quadratic component of the slope, b being the daily number of new cases (e.g., 4133), i being the rescaled calendar date with the first calendar date rescaled to 1, and 117 658 being the cumulative number of COVID-19 cases before extrapolation. We used values of 0 (linear extrapolation), 25 (slow quadratic extrapolation), and 50 (fast quadratic extrapolation) for a. Since the number of daily reported new COVID-19 cases did not continue increasing after 27 March 2020, we did not include exponential growth of cumulative case numbers.
Using the extrapolated daily cumulative case numbers, we estimated the daily number of newly detected COVID-19 cases. Subsequently, we assumed different proportions of new patients needing intensive care (3–10%), based on the experience in Spain (6.2%) [5], Italy (9–11%) [6], and the USA (8.2%) [7]. Based on the calibration study (see below) for the German data, we assumed a proportion of 3%.
In addition, we assumed an average period of 8 days from detection of COVID-19 to the need for intensive care. We assumed the duration of intensive care to be either 14 or 20 days. The estimated number of daily ICU cases up to 18 April is based on the daily numbers of new COVID-19 infections reported by the Robert Koch Institute (RKI) up to 10 April 2020. The assumed interval of 8 days between reporting and the requirement for intensive care explains why the daily ICU cases until 18 April could be estimated from empirical data. Thereafter, the estimated numbers are based on the extrapolated new COVID-19 case numbers as yielded by the three scenarios mentioned above for the period 11 April through 30 June 2020. The number of COVID-19 patients requiring oxygenation or ventilation in the ICU can be calculated by multiplying our case numbers for COVID-19 patients needing ICU treatment by 73.7%, which corresponds to the proportion of COVID-19 patients in the ICU requiring oxygenation or ventilation.
The DIVI intensive care registry reported for 9 April 2020 that 1888 COVID-19 cases were being treated in German ICUs [2]. We used this number to determine the calibration of our projection of COVID-19 patients requiring daily intensive care. All calculations were performed with SAS 9.4 (Cary, NC, USA).
Results
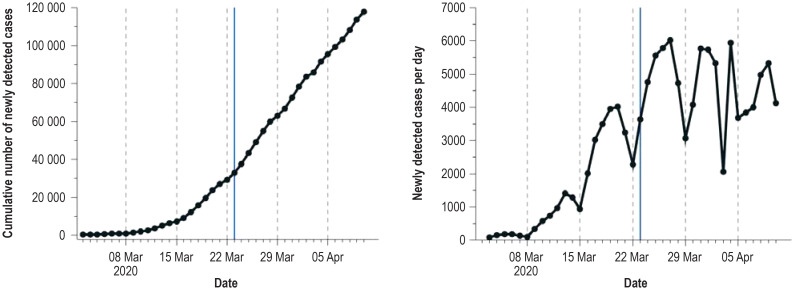
Since the nationwide measures to reduce interpersonal contact (lockdown) from 23 March to 10 April 2020 there has been an almost linear increase in the cumulative number of confirmed COVID-19 cases in Germany. The daily number of confirmed new cases has not shown any pronounced increase since the lockdown; it has fluctuated between 2051 and 6014 cases with a median of 4757 cases. The lower numbers of new cases reported on Sundays arise from the fact that not all health authorities report new cases to the Robert Koch Institute on Sundays and therefore represent an artifact (figure 1).
Figure 1.
Observed cumulative and daily numbers of newly confirmed COVID-19 cases up to 10 April 2020 (data from Robert Koch Institute [4]) Vertical blue line: start of lockdown on 23 March 2020; vertical dotted lines: Sundays
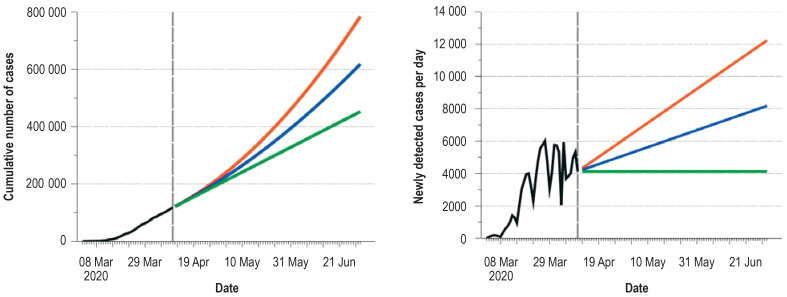
The extrapolation of newly registered COVID-19 cases yields a maximum of 4133 (linear extrapolation) to 12 233 cases (fast quadratic extrapolation) per day up to 30 June 2020, with a total number of between 452 431 (linear extrapolation) and 784 531 (fast quadratic extrapolation) newly registered COVID-19 cases by that date (Figure 2).
Figure 2.
Observed (up to 10 April 2020) and extrapolated cumulative and daily numbers of newly confirmed COVID-19 cases
Green line: linear extrapolation of the cumulative number of newly confirmed COVID-19 cases
Blue line: slow quadratic extrapolation of the cumulative number of newly confirmed COVID-19 cases
Red line: fast quadratic extrapolation of the cumulative number of newly confirmed COVID-19 cases
Vertical dashed line: after this line the daily numbers are based on the extrapolated number of newly diagnosed COVID-19 cases.
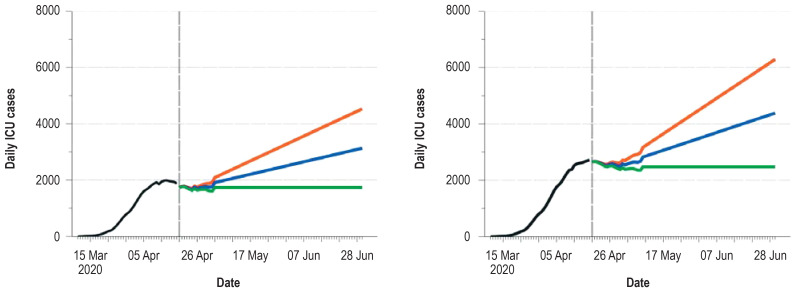
If a linear temporal trend of cumulative case numbers continues and 3% of the patients with COVID-19 come to need intensive care, the maximum daily ICU bed occupancy is reached around the middle of April (14 April for 14 days of intensive care, 20 April for 20 days of intensive care). The maximum number of patients requiring intensive care at the same time would be 1989 (14 days’ intensive care) or 2790 (20 days’ intensive care). With a fast quadratic increase in cumulative case numbers, the maximum utilization would be reached on 30 June 2020, with 4529 (14 days of intensive care) or 6290 patients (20 days of intensive care) (Figure 3, Table 1). The proportion of ICU patients requiring oxygenation or artificial ventilation is expected to be 73.7%. For example, if 6290 patients require intensive care on 30 June 2020, 4636 of them can be expected to need oxygenation or artificial ventilation.
Figure 3.
Estimated daily numbers of patients with COVID-19 requiring ICU treatment
Left: the proportion requiring 14 days of ICU treatment, starting on average 8 days after diagnosis (3%)
Right: the proportion requiring 20 days of ICU treatment, starting on average 8 days after diagnosis (3%)
Green line: linear extrapolation of the cumulative number of newly confirmed COVID-19 cases
Blue line: slow quadratic extrapolation of the cumulative number of newly confirmed COVID-19 cases
Red line: fast quadratic extrapolation of the cumulative number of newly confirmed COVID-19 cases
Vertical dashed line: to the right of this line (19 April 2020) the estimated daily ICU cases are based on extrapolated numbers of daily registered COVID-19 cases.
Table 1. Estimation of the daily number of COVID-19 cases requiring treatment in an intensive care unit (ICU) in Germany from 11 April to 30 June 2020 (assuming 8 days from report to need for intensive care)*.
| Trend | Need for ICU care (%) | Maximum number of COVID-19 cases needing ICU care | Date |
|
Linear Average ICU stay 14 days |
3 4 5 6 7 8 9 10 |
1989 2652 3315 3978 4641 5304 5967 6630 |
14 April |
| Average ICU stay 20 days |
3 4 5 6 7 8 9 10 |
2790 3720 4650 5580 6510 7440 8370 9300 |
20 April |
|
Slow quadratic Average ICU stay 14 days |
3 4 5 6 7 8 9 10 |
3132 4176 5221 6265 7309 8353 9397 10 441 |
30 June |
| Average ICU stay 20 days |
3 4 5 6 7 8 9 10 |
4385 5846 7308 8770 10 231 11 693 13 154 14 616 |
|
|
Fast quadratic Average ICU stay 14 days |
3 4 5 6 7 8 9 10 |
4529 6038 7548 9058 10 567 12 077 13 587 15 096 |
30 June |
| Average ICU stay 20 days |
3 4 5 6 7 8 9 10 |
6290 8386 10 483 12 580 14 676 16 773 18 869 20 966 |
|
* Maximum daily COVID-19 cases within the time interval; if the maximum extends over a longer period, the first date of occurrence of the maximum is presented
Under the assumption of a constant daily number of reported new cases of COVID-19, the proportion of all ICU beds in Germany that is needed each day for COVID-19 patients depends heavily on the other assumptions made. Assuming 20 000 new cases daily (around five times as many cases as observed on 10 April 2020) and 6% of patients requiring intensive care for 14 days, 16 800 ICU beds would be needed, i.e., 56% of the current capacity (table 2).
Table 2. Number of intensive care unit (ICU) beds needed per day in relation to the daily number of new COVID-19 cases, the proportion of patients requiring intensive care, and the length of ICU stay.
| Daily number of new cases | Need for intensive care (%) | Length of ICU stay | ICU beds needed per day | Proportion of overall ICU bed capacity in Germany (%) | Length of ICU stay | ICU beds needed per day | Proportion of overall ICU bed capacity in Germany (%) | ||
| 4133 | 3 | 14 days | 1736 | 6 | 20 days | 2480 | 8 | ||
| 8000 | 3360 | 11 | 4800 | 16 | |||||
| 12 000 | 5040 | 17 | 7200 | 24 | |||||
| 16 000 | 6720 | 22 | 9600 | 32 | |||||
| 20 000 | 8400 | 28 | 12 000 | 40 | |||||
| 40 000 | 16 800 | 56 | 24 000 | 80 | |||||
| 4133 | 4 | 14 days | 2314 | 8 | 20 days | 3306 | 11 | ||
| 8000 | 4480 | 15 | 6400 | 21 | |||||
| 12 000 | 6720 | 22 | 9600 | 32 | |||||
| 16 000 | 8960 | 30 | 12 800 | 43 | |||||
| 20 000 | 11 200 | 37 | 16 000 | 53 | |||||
| 40 000 | 22 400 | 75 | 32 000 | 107 | |||||
| 4133 | 5 | 14 days | 2893 | 10 | 20 days | 4133 | 14 | ||
| 8000 | 5600 | 19 | 8000 | 27 | |||||
| 12 000 | 8400 | 28 | 12 000 | 40 | |||||
| 16 000 | 11 200 | 37 | 16 000 | 53 | |||||
| 20 000 | 14 000 | 47 | 20 000 | 67 | |||||
| 40 000 | 28 000 | 93 | 40 000 | 133 | |||||
| 4133 | 6 | 14 days | 3472 | 12 | 20 days | 4960 | 17 | ||
| 8000 | 6720 | 22 | 9600 | 32 | |||||
| 12 000 | 10 080 | 34 | 14 400 | 48 | |||||
| 16 000 | 13 440 | 45 | 19 200 | 64 | |||||
| 20 000 | 16 800 | 56 | 24 000 | 80 | |||||
| 40 000 | 33 600 | 112 | 48 000 | 160 | |||||
| 4133 | 7 | 14 days | 4050 | 13 | 20 days | 5786 | 19 | ||
| 8000 | 7840 | 26 | 11 200 | 37 | |||||
| 12 000 | 11 760 | 39 | 16 800 | 56 | |||||
| 16 000 | 15 680 | 52 | 22 400 | 75 | |||||
| 20 000 | 19 600 | 65 | 28 000 | 93 | |||||
| 40 000 | 39 200 | 131 | 56 000 | 187 | |||||
| 4133 | 8 | 14 days | 4629 | 15 | 20 days | 6613 | 22 | ||
| 8000 | 8960 | 30 | 12 800 | 43 | |||||
| 12 000 | 13 440 | 45 | 19 200 | 64 | |||||
| 16 000 | 17 920 | 60 | 25 600 | 85 | |||||
| 20 000 | 22 400 | 75 | 32 000 | 107 | |||||
| 40 000 | 44 800 | 149 | 64 000 | 213 | |||||
| 4133 | 9 | 14 days | 5208 | 17 | 20 days | 7439 | 25 | ||
| 8000 | 10 080 | 34 | 14 400 | 48 | |||||
| 12 000 | 15 120 | 50 | 21 600 | 72 | |||||
| 16 000 | 20 160 | 67 | 28 800 | 96 | |||||
| 20 000 | 25 200 | 84 | 36 000 | 120 | |||||
| 40 000 | 50 400 | 168 | 72 000 | 240 | |||||
| 4133 | 10 | 14 days | 5786 | 19 | 20 days | 8266 | 28 | ||
| 8000 | 11 200 | 37 | 16 000 | 53 | |||||
| 12 000 | 16 800 | 56 | 24 000 | 80 | |||||
| 16 000 | 22 400 | 75 | 32 000 | 107 | |||||
| 20 000 | 28 000 | 93 | 40 000 | 133 | |||||
| 40 000 | 56 000 | 187 | 80 000 | 267 |
* Newly reported COVID-19 case as of 10 April 2020: n=4.133; all calculations assume that the daily number of newly reported cases remains constant over time; the total ICU bed capacity in Germany is assumed to be n=30 005 beds.
With 3.0% of patients needing intensive care, an interval of 8 days between the reporting of a positive test and intensive care becoming mandatory, and a 14-day stay in intensive care, our projection for 9 April 2020 yields 1879 patients requiring intensive care, while the DIVI registry reported 1888 patients with COVID-19 being treated in ICUs on that day. However, the DIVI intensive care registry was not at that time receiving data for all ICU beds in Germany. The registry covered about 83% of all hospitals, particularly the larger hospitals and university clinics. We speculate that circa 90% of the COVID-19 cases requiring intensive care at that time were included in the registry. That would imply a complete total of around 2098 patients. With 3.3% of patients needing intensive care, an interval of 8 days between the reporting of a positive test and intensive care becoming mandatory, and a 14-day stay in intensive care, our projection amounts to 2066 patients.
Discussion
We used three pessimistic non-exponential scenarios of the development of numbers of newly diagnosed COVID-19 cases in Germany, despite the fact that the number of newly detected COVID-19 cases has not been increasing, but rather stagnating, since the end of March 2020. Under the assumptions that 3–10% of newly detected COVID-19 patients require intensive care and their average length of ICU stay is either 14 or 20 days, we arrive at maximum daily case numbers in ICUs between 1989 (linear extrapolation, 3% ICU, 14 days in the ICU) and 20 966 (fast quadratic extrapolation, 10% ICU, 20 days in the ICU). Calibration with the COVID-19 ICU occupancy figures numbers from the DIVI registry for 9 April 2020 indicates a maximum daily number of COVID-19 patients requiring intensive care that is closer to the low than to the high end of this range.
From our point of view, the results of the extrapolation give no rise for concern about an impending necessity for triage of COVID-19 patients requiring intensive care. It should be noted, however, that not all ICU beds are available for COVID-19 cases. On 17 April 2020, for example, 51% of the ICU beds were occupied by patients other than those with COVID-19. Furthermore, the occupancy of ICU beds in hospitals in Germany is not uniform, so in the absence of nationwide coordination the ICUs of some hospitals may be overloaded while others have low occupancy.
In contrast to our non-exponential extrapolations, Meares and Jones used an exponential extrapolation of the COVID-19 case numbers in Australia to estimate the required ICU capacity [8]. We chose not to use this approach, because since 27 March 2020, numbers of newly reported COVID-19 cases in Germany have stagnated or declined. Furthermore, a gradual, controlled loosening of the lockdown with continued compliance with hygiene measures and an anticipated rapid response in the event of an increase in the number of new COVID-19 cases makes a future exponential increase in the number of new cases in Germany unlikely. Although it does not at the moment seem very likely that exponential growth will resume for an extended period of time, policies are needed to ensure that this will not happen. It should be noted that our results do not contain any recommendations for action to ease the lockdown.
There are several factors that limit our results. First, we could only use laboratory-confirmed COVID-19 cases from the period 2 March through 20 April 2020 for our estimation. Due to the limited availability of COVID-19 test kits and therefore restricted use of this test, and due to its limited sensitivity, the true number of COVID-19 cases in Germany will be considerably larger than officially reported by the Robert Koch Institute. Li et al. recently estimated that 86% of all COVID-19 infections in China went undocumented [9]. Second, the development of the cumulative number of newly registered COVID-19 cases up to the end of June 2020 is a projection. However, we used three different pessimistic non-exponential scenarios of the development in Germany despite the fact that the daily number of newly reported COVID-19 cases has not been increasing, but rather stagnating, since the end of March 2020. Third, we could not distinguish between COVID-19 patients requiring intensive care with or without artificial ventilation. Our estimated case numbers for COVID-19 cases requiring intensive care can be used to estimate the numbers of patients requiring non-invasive ventilation, mechanical ventilation, high-flow oxygen therapy, or extracorporeal membrane oxygenation on the basis of our assumption, from DIVI intensive care registry data, that 73.7% of COVID-19 patients admitted to German ICUs need one or other of these treatments.
Key Messages.
Provided there is no exponential increase in COVID-19 cases numbers in Germany, the country’s existing intensive care bed capacity seems sufficient.
In view of the course the COVID-19 pandemic is taking in Germany, there appears to be no need for a debate about triage; intensive care bed occupancy should be coordinated on a nationwide basis, however, particularly at times of high case numbers.
If 16 000 new cases of COVID-19 were detected daily, 6% of the patients needed intensive care, and all of these stayed in the intensive care unit for 20 days, 19 200 intensive care beds (64% of all such beds in Germany) would be needed each day for patients with COVID-19.
Acknowledgments
Acknowledgment
Dr. Stang receives a research grant from the German Federal Ministry of Education and Science (BMBF), project number 01ER1305.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Gillmann B. RKI: Zahl der Intensivbetten wird nicht reichen. Handelsblatt. 3. April 2020. www.handelsblatt.com/politik/deutschland/corona-epidemie-rki-zahl-der-intensivbetten-wird-nicht-reichen/25712008.html?ticket=ST-3270452-GX9WyecmTh5JaI6nXhqJ-ap1 (last accessed on 5 April 2020) [Google Scholar]
- 2.Täglicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19) Aktualisierter Stand für Deutschland 9.4.2020: www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-04-07-de.pdf?__blob=publicationFile (last accessed on 10 April 2020) [Google Scholar]
- 3.DIVI-Intensivregister. www.intensivregister.de/#/intensivregister (last accessed on 17 April 2020) [Google Scholar]
- 4.Robert Koch-Institut. COVID-19-Dashboard. https://experience.arcgis.com/experience/478220a4c454480e823b17327b2bf1d4 (last accessed on 11 April 2020) [Google Scholar]
- 5.Centro de Coordinación de Alertas y Emergencias Sanitarias. Actualización nº 52. Enfermedad por el coronavirus (COVID-19). 22.03.2020 (datos consolidados a las 21:00 horas del 21.03.2020). Madrid: Centro de Coordinación de Alertas y Emergencias Sanitarias; 2020. www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/Actualizacion_52_COVID-19.pdf (last accessed on 11 April 2020) [Google Scholar]
- 6.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC COVID-19 Response Team. Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meares HDD, Jones MP. When a system breaks: a queuing theory model for the number of intensive care beds needed during the COVID-19 pandemic. Med J Aust (preprint): www.mja.com.au/journal/2020/212/10/when-system-breaks-queuing-theory-model-number-intensive-care-beds-needed(last accessed on 18 April 2020) 2020:1–9. [Google Scholar]
- 9.Li E, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020 doi: 10.1126/science.abb3221. eabb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]