Dear Editor,
We read with interest the report by Zoia et al. [3], and we would like to widen the picture by sharing our experience in Madrid’s COVID-19 reference center, one of the hardest hit areas in Europe. As neurosurgeons, we never would have imagined being in the eye of the storm. We hope our humble experience can be helpful to colleagues in other countries.
On 27 April 2020, Spain represented the hardest hit European country by the COVID-19 pandemic with 219,764 cases and 48.2 deaths per 100,000 inhabitants. Madrid became the epicenter of the outbreak, with 59,126 cases diagnosed, and a death toll of 7,922 hospitalized victims.
The national reference center for contagious diseases housed within our institution, Carlos-III Microbiologic National Center, registered its first SARS-CoV-2 positive patient on 25 February 2020 and by mid-March, our hospital was already collapsed, becoming the Spanish epicenter.
A field hospital and private hospitals sheltered many patients and our 1,153 beds hospital capability increased by an extra 180 beds. The usual 72 intensive care unit (ICU) beds have been extended to 150, by utilizing the pediatric and cardiac ICU and most operating rooms (ORs), sheltering up to 145 COVID-19 patients.
Emergency unit expanded from its 100-bedded regular capacity to 160 and our six emergency assessment units became eleven. A triage system to separate patients with clear or suspicious symptoms attended by emergency physicians—from patients with symptoms that do not suggest COVID-19—attended by the proper specialists—was created in a tent-hospital outside with its own CT scanner, as highly suspicious patients with negative test undergo CT scan.
Relinquishing specialty ward space for the COVID-19 patients was necessary, and avoidance of elective surgery is highly recommended [1].
We initially prioritized our patients into three groups:
Group A: Severe or life-threatening emergencies.
Group B: Oncological pathologies where treatment cannot be postponed.
Group C: Regular elective surgeries.
We are managing group A cases, group B is diverted to another hospital, and group C are suspended until further notice. We also became one of two reference centers for pediatric neurosurgical emergencies. Interestingly, the number of patients with all emergency pathologies has worryingly reduced.
Five neurosurgical ORs were re-assigned for adult emergencies in general, two of them dedicated to COVID-19 patients as over 50% of patients are testing positive when we carry out routine preoperative swabs.
The strain on our internal medicine colleagues makes their work challenging, worsened as several of them tested positive and went into isolation. To help them, while covering our departmental workload, we reorganized our neurosurgical staff while maintaining physical distancing amongst ourselves and ensuring a fortnight of self-isolation after working on COVID-19 units, a main concern being that viral transmission amongst our department could dramatically limit the number of us available.
Four groups of two neurosurgeons were established:
Group A: Neurosurgeons with potential vulnerability to COVID-19. They assumed daily neurosurgery inpatient care.
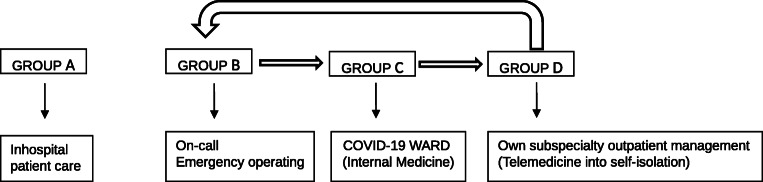
Groups B, C, and D: Other consultants organized on a rotating schedule to work on different activities for 14 days (Fig. 1).
“Urgent neurosurgery”: Only visiting emergency patients and using the OR.
COVID-19 wards.
Telemedicine. Outpatient clinical consultations and own subspecialty patients.
Fig. 1.
Workflow at our department during the COVID-19 outbreak. Thick arrows: Flow direction. Thin arrows: Activity assigned to every group
As neurosurgeons of any grade, we are working side by side with internists. At first, we started with easy tasks, such as reviewing patients, ordering CT scans, and informing families; now we are more involved, able to make autonomous decisions in patient management. We have together overcome several setbacks, like the anguishing possibility that personal protective equipment or essential medicines might run out soon and they are infinitely thankful.
The stress of catching the virus or infecting a loved one caused anxiety and many of us moved away from home to apartments or hotel rooms. But patients and their gratitude are the best motivation to carry on.
They are struggling against the loneliness and the fear, as they are absolutely alone in their rooms. Some of them can manage to use the phone and talk with the family, but others and especially the elderly cannot. Often the only human contact they have are nurses and doctors with the protective “alien-like” suits. Some of these patients die alone. At the same time, we too feel the anxiety of their families, equally lonely at home, unable to say goodbye to their loved ones.
As doctors, we are used to seeing people die, but we are not used to this high number of people dying every single day. Many of the frontline staff, ourselves included, cannot avoid crying when returning home, feeling guilty of being away from the hospital [2]. Yet at the same time, we have never experienced such depth of humanity amongst ourselves and amongst multitudes of colleagues abroad who have been sending their best thoughts. There is no doubt of this tragedy will mark our lives, making us a stronger community.
Acknowledgments
We would like to thank to Andreas Demetriades FRCS, Edinburgh, who contributed substantially to the conception of this work and provided critical revision of the manuscript.
Authors’ contributions
MLGG wrote the manuscript, MSA contributed to write the manuscript, and JMR provided critical revision of the manuscript. All authors reviewed the final manuscript.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lei S, Jiang F, Su W, Chen C, Chein J, Mei W et al (2020) Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 10.1016/j.eclinm.2020.100331 [DOI] [PMC free article] [PubMed]
- 2.Sasangohar F, Jones SL, Masud FN, Vahidy FS, Kash BA (2020) Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesth Analg. 10.1213/ANE.0000000000004866 [DOI] [PMC free article] [PubMed]
- 3.Zoia C, Bongetta D, Veiceschi P (2020) Neurosurgery during the COVID-19 pandemic: update from Lombardy, Northern Italy (2020). Acta Neurochir. 10.1007/s00701-020-04305-w [DOI] [PMC free article] [PubMed]