We read with interest the manuscript by Dr. Singhal and share similar opinion regarding the difficulties to balance the benefits and risks of a surgical exploration in case of suspected internal hernia (IH) after Roux-en-Y gastric bypass (RYGB) during the present context of COVID-19 pandemic [1].
Indeed, as stated by Dr. Singhal, internal hernia (IH) represents a frequent cause of obstruction after RYGB leading to potentially severe consequences [2]. IH clinical presentation is nonspecific and commonly associates intermittent gastrointestinal symptoms usually worsened by food intake, subsequently leading to anorexia [2]. Noteworthy, COVID-19 infection can also be diagnosed upon various nonspecific digestive symptoms in 3 to 79% of cases according to the published series. These symptoms include anorexia (39.9–50.2%), vomiting (3.6–66.7%), diarrhea (2–49.5%), and/or abdominal pain (2.2–6%) [3]. However, little is currently known on these gastrointestinal symptoms in the context of patients previously operated from bariatric surgery and especially after procedures that modify the gastrointestinal tract anatomy (i.e., RYGB).
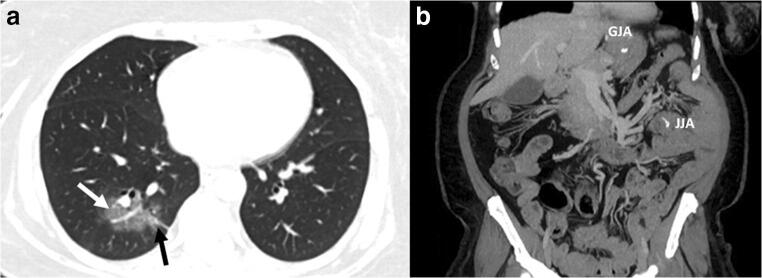
We recently admitted a 57-year-old female patient who had undergone a RYGB 5 years and 1 month earlier for grade III obesity (112 kg; body mass index: 42 kg/m2) associated with type 2 diabetes, hypertension, and obstructive sleep apnea syndrome. Based on the patient charts, mesenteric defects were left open during the procedure. The initial postoperative course and the follow-up were uneventful. At her planned 5-year postoperative follow-up appointment (February 2020), she weighed 85 kg (BMI: 31.8 kg/m2) and had a normal physical examination. Two months later (April 2020), she presented with transient and unspecific episodes of acute abdominal pain aggravated by food intake followed by anorexia and absence of flatus. She displayed neither signs of pulmonary infection nor general signs of severity or fever. On laboratory tests, white blood cell count and PCT were within normal ranges, and CRP was slightly increased (13.7 mg/L N < 5 mg/l). Since the clinical history was highly suggestive of an IH, we performed an emergent abdominal CT scan. While abdomen imaging was normal, we incidentally found, on chest CT images, signs typically suggestive of COVID-19 infection (Fig. 1) [4]. The nasopharyngeal swab, analyzed by real-time polymerase chain reaction (RT-PCR) testing, proved positive for severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2; i.e., COVID 19). The patient was hospitalized and benefitted from COVID-19 symptomatic treatment and further discharged after 2 days of observation with favorable clinical evolution. Two weeks later, she no longer complained from any digestive symptom and was recovering in spite of persisting asthenia.
Fig. 1.
a Axial chest CT showing features of COVID-19: multiple ground-glass opacities with interlobular septal thickening (white arrow) and vascular enlargement (black arrow) in the peripheral of the right lung. b Coronal abdominal CT scanner showing no direct/indirect signs of internal hernia or obstructions. GJA, gastro-jejunal anastomosis; JJA, jejuno-jejunal anastomosis
RYGB is a procedure that allows an important and sustainable weight loss [5]. It enables major improvement in obesity and its related complications, thus leading to reduced premature death [6]. Nevertheless, since the mean BMI loss 12 years after RYGB reaches 11.5 kg/m2, a non-negligible amount of patients remain with a postoperative BMI ≥ 30 kg /m2. Importantly, obesity whatever its grade represents a known risk factor of severe forms of COVID-19, whether or not it is associated with other demonstrated risks factors such as hypertension or type 2 diabetes [7].
Findings from this case report combined with recent knowledge on the various clinical presentations of COVID-19 may justify a systematic chest and abdominal CT in patients operated from RYGB, seen in the emergency room with acute and nonspecific digestive symptoms. This would help provide optimal management and avoid potentially dangerous surgical procedure in the times of this pandemic.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Louis Betton, Email: betton.louis@gmail.com.
Deborah Benchetrit, Email: deborah.benchetrit@aphp.fr.
Judith Aron-Wisnewsky, Email: judith.aron-wisnewsky@aphp.fr.
Jean-Michel Oppert, Email: jean-michel.oppert@aphp.fr.
Adriana Torcivia, Email: adriana.torcivia@aphp.fr.
Jean-Christophe Vaillant, Email: jean-christophe.vaillant@aphp.fr.
Laurent Genser, Email: laurent.genser@aphp.fr.
References
- 1.Singhal R. Internal Hernia in the Times of COVID-19: to Laparoscope or Not to Laparoscope? OBES SURG [Internet]. 2020 [cited 2020 Apr 17]; Available from: 10.1007/s11695-020-04598-x [DOI] [PMC free article] [PubMed]
- 2.Stenberg E, Szabo E, Ågren G, Ottosson J, Marsk R, Lönroth H, Boman L, Magnuson A, Thorell A, Näslund I. Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet. 2016;387:1397–1404. doi: 10.1016/S0140-6736(15)01126-5. [DOI] [PubMed] [Google Scholar]
- 3.Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li M. Chest CT features and their role in COVID-19. Radiol Infect Dis 2020; [DOI] [PMC free article] [PubMed]
- 5.Adams TD, Davidson LE, Litwin SE, Kim J, Kolotkin RL, Nanjee MN, Gutierrez JM, Frogley SJ, Ibele AR, Brinton EA, Hopkins PN, McKinlay R, Simper SC, Hunt SC. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377:1143–1155. doi: 10.1056/NEJMoa1700459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Global BMI Mortality Collaboration Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). 2020; [DOI] [PMC free article] [PubMed]