Summary:
Ledderhose disease (LD) is a rare plantar fibromatosis of the foot, frequently associated with Dupuytren disease. Collagenase of Clostridium hystoliticum has recently revolutionized the way to treat Dupuytren disease. Nevertheless, the literature is still critically lacking about the use of collagenase injection in LD. We report a case of a man with bilateral symptomatic LD treated with collagenase. Injections (0.58 mg of collagenase of C. hystoliticum) were performed into nodules. Forced extension after injection was not performed. The patient could walk normally immediately after procedure. The procedure was a complete success without side effects or complications on either foot. Currently, at 14 months after treatment of the right foot and 12 months after treatment of the left foot, no recurrence has been observed. Collagenase injection was only effective in treating symptomatic LD in this one patient we reported on.
Ledderhose disease (LD) is a benign and rare fibromatosis of the foot, involving the plantar aponeurosis. LD has been described as similar to Dupuytren disease (DD).1
It can occur more commonly in males, at all ages, especially between third and fifth decades, often with bilateral involvement.1
Unlike DD, LD is often symptomatic, with frequent pain episodes, plantar swelling, and in advanced cases, retractions and fascial contractures.1–3
Surgical treatment is sometimes burdened with wound dehiscence, pathologic and painful scars, and possible recurrence.2 Furthermore, patients are forbidden to walk until the wounds are closed.
Several nonsurgical treatments have been proposed to avoid complications from surgical operation, with some convincing results.1–4
We report a case of bilateral symptomatic LD successfully treated with intranodular injection of collagenase of Clostridium hystoliticum (CCH). The patient was permitted to walk immediately after the injection. No significant side effects were observed.
CASE REPORT
A 59-year-old male patient, affected by recurrent bilateral DD, reported smoking, diabetes, and systemic arterial hypertension. The patient reported a 5-year onset LD of the right foot and 3-year onset of the left foot. Both sides presented with a nodule of the first ray, just proximally to metatarsophalangeal joint. Until surgical treatment both feet were symptomatic. Pain limited walking and even worse running (Visual Analogue Scale right: 6.2; Visual Analogue Scale left: 5.1). He tried orthotics for 1 year without benefits. No more treatments were previously performed.
In our institution, we are experienced in surgical treatment of LD. However, for a short time now, we have been using CCH to treat DD with very promising results. Hence CCH has become the first choice for treatment of DD in our institution. CCH was proposed to our patient suffering from LD as an alternative to traditional surgical therapy. The patient was completely informed about the unusual application of the drug. He refused surgery, considering postoperative walking limitation unacceptable, and approved the CCH injection.
The right side, which was the most painful one, was injected first. The injection was performed according to traditional technique.4 The procedure was performed in the operating room. The patient remained awake with anesthesiologic assistance. We injected 0.58 mg of reconstituted drug in a volume of 0.25 mL into the palpable nodule (intranodular injection) (Fig. 1). No passive extension was provided after injection, unlike DD treatment. After the procedure, a soft dressing was applied. The patient was allowed to load the lower limb until tolerance level. Two hours of clinical observation followed infiltration (to check for systemic reactions related to the procedure). The patient was dismissed with recommendation of wearing large running shoes that permit walking and accommodation of the dressing.
Fig. 1.
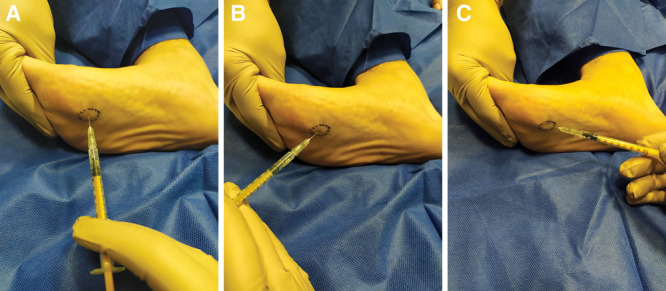
Drug (0.25 mL) was injected into the nodule, dividing the dose into 3 parts, according to the standard technique. A, First part is shown. B, Second part is shown. C, Third one is shown.
The patient was assessed postoperatively 3 days after injection; he complained of plantar pain (site of injection) that remitted after acetaminophen assumption. Clean bandages were not removed; no bruising or swelling of the foot and/or the ankle was detected. After 3 days, the patient reported a decrease in plantar pain. The dressing was removed revealing a medium plantar ecchymosis, up to the medial aspect of the foot. There was no pathologic swelling of the foot. The previously palpable nodule of the metatarsophalangeal joint of the first ray was not detectable yet.
The patient was satisfied with the treatment. He asked for the same treatment for the left foot. Currently, after 12 months from left side treatment and 14 from right, no recurrence has been observed.
DISCUSSION
LD could be treated in several ways, depending on the severity of the disease, with uncertain outcomes.1–3,5 Steroid injections, physiotherapy, extracorporeal shock wave therapy, and radiotherapy are currently used.1,2 Even if nonoperative treatments may not completely heal LD, they should be tried before surgical treatment.2 Surgical treatment is reserved for nonresponsive patients, advanced and critically symptomatic disease with walking or balancing impairment.2,3 Surgery consists in a complete or partial resection of the aponeurosis; in some cases, exclusively nodules resection can be performed.3,5 Wound closure should be realized with particular care to avoid recurrences, pathologic and painful scars, and wound dehiscence. In case of surgery, patients should not walk until wound closure.
An endoscopic approach could minimize complications such as wound dehiscence, pathologic scars, or infections, but nerves injuries, arteries injuries, and disease recurrence more easily occur.5
Only open surgical treatment (complete fasciectomy) can completely eradicate the disease.3 However, recurrence rate is not clearly known.2
The use of CCH for DD is effective with acceptable recurrence rates.6 Recurrence rates after CCH injection are comparable with recurrence rates after surgical operation.7
CCH injections should be performed by expert hand surgeons, and complications can occur (eg, hematoma, skin laceration, neurovascular damage, and tendon rupture).4
Unlike LD, DD nodules are rarely symptomatic. However, intranodular injection has been already investigated in DD, reducing hardness and size of nodules.8
About the use of CCH in LD, the literature is very poor.2,9 Only one study reported a case of CCH injection in a LD nodule.9 However, the patient previously underwent plantar fasciectomy and several steroid injections, and finally, CCH was injected for 3 times without benefits.9
Hammoudeh9 attributed the failure to the anatomo-pathologic properties of LD that differ from those of DD. Differently from our case, CCH injection was performed in a previously treated foot (surgery and steroid injections). In our non-previously treated patient, the absence of scar tissue can explain the positive result.
In this study, we report the results from CCH injections in a previously untreated patient.
We performed an intranodular injection as first treatment, according to the standard injection technique and standard dosage used for DD.4 CCH injection seems to have various positive points:
Intranodular injection seems to be safe and effective. The nodule, which causes pain, is wide enough to avoid the spreading of the drug out of it.
Forced extension after injection is not necessary. Walking can improve the spreading of the drug into the nodule; the plantar aponeurosis will hold its function.
Patient can return immediately to normal life, reducing the costs of hospitalization and medical care.
Painful scars are avoided.
Up to 14- and 12-month follow-up, no recurrence was observed. CCH has represented the ultimate solution only in one injection to the present day.
Unfortunately, we do not possess enough data to consider CCH the gold standard for treatment of LD.
In our experience, differently from Hammoudeh,9 CCH worked, although we reported the results from a single patient (2 injections).
CONCLUSIONS
We wish to emphasize that positive effects cannot be neglected. However, the effects of CCH injection in LD are poorly documented and little understood. We hope that more studies will improve the knowledge about this technique. The effects of CCH on very severe LD contracture should be further investigated.2,3,9 CCH injection is a low-invasive but effective treatment for symptomatic LD.
Footnotes
Published online 27 April 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Carroll P, Henshaw RM, Garwood C, et al. Plantar fibromatosis: pathophysiology, surgical and nonsurgical therapies: an evidence-based review. Foot Ankle Spec. 2018;11:168–176. [DOI] [PubMed] [Google Scholar]
- 2.Young JR, Sternbach S, Willinger M, et al. The etiology, evaluation, and management of plantar fibromatosis. Orthop Res Rev. 2019;11:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neagu TP, Ţigliş M, Popescu A, et al. Clinical, histological and therapeutic modern approach of Ledderhose disease. Rom J Morphol Embryol. 2018;59:691–697. [PubMed] [Google Scholar]
- 4.Hurst LC, Badalamente MA, Hentz VR, et al. ; CORD I Study Group. Injectable collagenase Clostridium histolyticum for Dupuytren’s contracture. N Engl J Med. 2009;361:968–979. [DOI] [PubMed] [Google Scholar]
- 5.Lui TH. Endoscopic subtotal fasciectomy of the foot. Arthrosc Tech. 2016;5:e1387–e1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Werlinrud JC, Hansen KL, Larsen S, et al. Five-year results after collagenase treatment of Dupuytren disease. J Hand Surg Eur Vol. 2018;43:841–847. [DOI] [PubMed] [Google Scholar]
- 7.Peimer CA, Blazar P, Coleman S, et al. Dupuytren contracture recurrence following treatment with collagenase Clostridium histolyticum (CORDLESS [Collagenase Option for Reduction of Dupuytren Long-Term Evaluation of Safety Study]): 5-year data. J Hand Surg Am. 2015;40:1597–1605. [DOI] [PubMed] [Google Scholar]
- 8.Costas B, Coleman S, Kaufman G, et al. Efficacy and safety of collagenase Clostridium histolyticum for Dupuytren disease nodules: a randomized controlled trial. BMC Musculoskelet Disord. 2017;18:374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammoudeh ZS. Collagenase Clostridium histolyticum injection for plantar fibromatosis (Ledderhose disease). Plast Reconstr Surg. 2014;134:497e–498e. [DOI] [PubMed] [Google Scholar]


