Supplemental Digital Content is available in the text.
Abstract
Background:
Electronic health records (EHRs) should help physicians stay organized, improve patient safety, and facilitate communication with both patients and fellow healthcare providers. However, few studies have directly evaluated physician satisfaction with EHR and its perceived impact on patient care. This study assessed trends and perceptions of EHR within the American plastic surgery community.
Methods:
An Institutional Review Board–approved survey that assessed demographics, patterns of EHR use, and attitudes toward EHR was deployed by the American Society of Plastic Surgeons Member Survey Research Services. Statistical analyses were performed using Stata 14.2 and QDA Miner Lite software (Version 2.0; Provalis, Montreal, Canada). Significance level was P < 0.05.
Results:
Among plastic surgeons who use EHR, EPIC Systems software (Epic, Verona, Wisc.) was the most common vendor, with users noting a net positive effect on the quality of care they provided to patients. Younger age and less years of experience were correlated with a more positive attitude toward EHR. Positive attitude was closely linked to shared responsibility among support staff over data entry, whereas negative attitude was tightly tied to the perceived time wasted because of EHR, followed by poor technical support and design.
Conclusions:
EHR use among plastic surgeons was more common in academic-associated specialties and larger practice groups. Overall, age and practice type had weak associations with perceptions of EHR usage. On average, there were slightly more positive perceptions of EHR usage than negative. The most commonly perceived issues with EHR were wasted time and barriers to user-friendliness. These findings suggest the need for greater physician involvement in EHR optimization.
INTRODUCTION
“This EHR fiasco was the worst governmental intrusion into Medicine since managed care of the 1990s and Medicare Act of 1964. We are now data collection agents of the government so Washington can know how overweight we are and how much we smoke as Americans”
“EMR is a major reason I am retiring at age 67”
The quotes above were 2 of the 164 responses to an optional question in our survey about electronic health record (EHR) use among plastic surgeons.
EHRs were developed and implemented to help physicians stay organized, improve patient safety by maintaining confidentiality and reducing medical errors, and facilitate communication with both patients and fellow healthcare providers.1,2 In addition, from a purely clinical perspective, EHRs were intended to improve the overall quality of care provided by the physician.
Although there are no federal requirements for physicians to use EHR, they are incentivized to do so.3 As delineated by the Medicare Access and Children’s Health Insurance Program Reauthorization Act4 and Health Information Technology for Economic and Clinical Health Act,5 the federal government rewards physicians with subsidies for the “meaningful use” of EHR.6,7 The American Recovery and Reinvestment Act of 2009 described the 3 central characteristics of meaningful use as (1) using the EHR for a meaningful purpose (ex. prescribing medications); (2) exchanging health information electronically to improve healthcare quality; and (3) using EHR to submit clinical measures and quality.8 The goals of widespread implementation are noble, but over the past decade, EHR has been met with either staunch resistance or mixed results and satisfaction.5,9–11
In 2016, Martin and Sinsky12 published an article presenting several salient issues faced by clinicians and their use of EHR. In particular, they stressed that contemporary EHR systems prioritized the near-verbatim documentation of care over the actual delivery of care to the patient, resulting in “increased cognitive workload, strained clinician-patient relationships, and burnout.”12 Strong emphasis on structured data entry into EHR is useful for billing and reimbursement purposes, but seldom has this translated into an intuitive, effective system for physicians seeking to improve the quality of their patient care or conduct clinical research.13,14
Previous studies in a variety of medical disciplines have analyzed the trends in EHR implementation15 and physician wellbeing, especially with regard to physician burnout.16–18 Furthermore, few studies on EHR use and perception have been conducted within surgical specialties.2,3,19 Through this survey study, we sought to address the current lack of literature on trends and attitudes toward EHR within the plastic surgery specialty.
MATERIALS AND METHODS
Survey Instrument
We created an 18-question survey that assessed demographic data, patterns of EHR use, and perceptions of EHR within each plastic surgeon’s practice setting. The survey was piloted with plastic surgery residents and faculty at the Johns Hopkins School of Medicine Department of Plastic and Reconstructive Surgery. Completion of the survey took approximately 5 minutes. The full survey can be found in Supplemental Digital Content 1 (see appendix, Supplemental Digital Content 1, which displays the full survey which assessed demographics, patterns of EHR use, and attitudes, http://links.lww.com/PRSGO/B393).
This survey received Johns Hopkins School of Medicine Institutional Review Board approval and was distributed through the American Society of Plastic Surgeons (ASPS) Member Survey Research Services. The survey was chosen for distribution to the membership of ASPS through a standardized peer review process.
The survey was deployed via a SurveyMonkey e-mail link 3 times over 2 months to a random cohort of 2,500 active ASPS members. Characteristics of the cohort were reviewed by ASPS Member Survey Research Services to ensure that it was representative of the entire ASPS active membership with regard to practice type, practice demographic, and sex. In addition, this survey was also representative of membership with regard to geographic distribution of survey respondents. Completion of the survey was incentivized through randomized drawing for a $100 Amazon gift card.
Data Analysis
Data were summarized descriptively and graphically. Data analysis was divided into 3 focuses, and significance level was set at a P value of <0.05.
First, differences in characteristics of those who use EHR and those who do not use EHR were evaluated. The normality of continuous variables was assessed graphically and using Shapiro–Wilk test of normality. Continuous variables were found to have not met normality; therefore, Wilcoxon rank sum test was used. Specialty area of practice was a categorical variable that was not mutually exclusive and was evaluated for independence related to EHR use using a χ2 test of independence or a Fisher’s exact test as appropriate.
Second, differences in both age and years in practice when compared with attitude toward EHR were evaluated using Kruskal–Wallis test. It is important to note that normality was not achieved and assessed in the same fashion as described above.
Third, independence of both a switch in EHR vendor within the last 6 months and physician entering data primarily were tested as they related to attitude toward current EHR vendor using χ2 test of independence. It is important to note that variable of Primary Data Entry into EHR was converted from a categorical variable with 3 categories to a binary variable by sorting into Physician Primary Entry and Non-Physician Primary Entry. This variable related to question 13 in the survey and the 2 categories of Shared Responsibility Evenly and Support Staff were combined and categorized as Non-Physician Primary Entry.
QDA Miner Lite software (Version 2.0.5; Provalis, Montreal, Canada) was used for thematic analysis of responses provided for question 18. Major categories or “codes” for thematic analysis were chosen based on tone of response: negative, positive, or neutral. Each occurrence of a distinctly negative, positive, or neutral comment was labeled a “case” that fell under a more specific category, such as “time wasted” (negative) or “improved image management” (positive).
All quantitative data analysis was performed using Stata 14.2 (StataCorp, College Station, Tex.).
RESULTS
We received responses from 349 out of the 2,500 plastic surgeons (14% response rate) who were contacted for this survey. The average age of survey respondents was 53.26 years old (SD, 10.5 years), and the average number of years in practice was 19.11 (SD, 10.7). Detailed demographic characteristics and perceptions related to EHR of all respondents can be referenced in Tables 1 and 2, respectively.
Table 1.
Summary of Respondents' Characteristics
| Mean | SD | Range | |
|---|---|---|---|
| Age | 53.26 | 10.52 | 33–83 |
| No. providers in practice | 36.6 | 139.54 | 1–999 |
| Years in practice | 19.11 | 10.74 | 1–48 |
| Years respondent has used EHR | 6.72 | 5.29 | 0–29 |
Table 2.
Summary of Respondents’ Characteristics and Perceptions Related to EHR
| N (%) | |
|---|---|
| Respondents that currently use EHR | 349 (71.06) |
| Respondents who used paper records | 337 (98.81) |
| Factors that convinced respondents to use EHR | |
| Requirement | 337 (58.46) |
| Ease/efficiency | 337 (31.45) |
| Financial incentives | 337 (12.17) |
| Security | 337 (9.20) |
| Colleague | 337 (2.97) |
| Do not plan on using EHR | 337 (22.55) |
| Staff involved in entering data into medical record | |
| Physician | 305 (92.13) |
| Scribes | 305 (10.16) |
| Nurses | 305 (52.79) |
| Medical assistant | 305 (53.44) |
| Technician | 305 (11.48) |
| Secretary | 305 (47.21) |
| Staff that primarily enters data into medical record | |
| Physician | 313 (53.04) |
| Support staff | 313 (14.70) |
| Responsibility shared evenly | 313 (32.27) |
| Respondents that have changed EHR in last 6 months | 302 (10.60) |
| Respondents overall attitude toward current EHR vendor | |
| Positive | 317 (42.27) |
| Negative | 317 (39.75) |
| Does not use EHR | 317 (17.98) |
| Opinion of quality of care with EHR vs paper record | |
| Worse with EHR | 321 (23.99) |
| Same with EHR | 321 (25.86) |
| Better with EHR | 321 (32.40) |
| No paper record use | 321 (0.93) |
| No EHR use | 321 (16.82) |
There were several key differences between plastic surgeons who used and did not used EHR (Table 3). First, practice size among those who used EHR (50.37 practitioners) tended to be much larger than those of surgeons who did not used EHR (2.78 practitioners). Not only was this difference in mean values high, but the range and maximum values for both groups were quite varied with those who use EHR tending to report that they were in much larger practices (no EHR use, 1–50 practitioners; EHR use, 1–999 practitioners). Furthermore, of all the EHR vendors respondents currently used, EPIC Systems software (Epic, Verona, Wisc.) was by far the most common, although a wide variety of other vendors were also found to be used (Fig. 1). Of those respondents who used EHR, the majority reported that EHR had a net positive effect on the quality of care they provided to patients (Fig. 2).
Table 3.
Characteristics of Plastic Surgeons with or without EHR Use
| Characteristics According to EHR Use | EHR Use n = 248, Mean (SD) | No EHR Use n = 100, Mean (SD) | P |
|---|---|---|---|
| Age | 51.23 (10.4) | 58.36 (9.02) | <0.001 |
| Year in practice | 16.94 (10.53) | 24.60 (9.26) | <0.001 |
| Practice size | 50.37 (163.60) | 2.78 (5.23) | <0.001 |
Fig. 1.
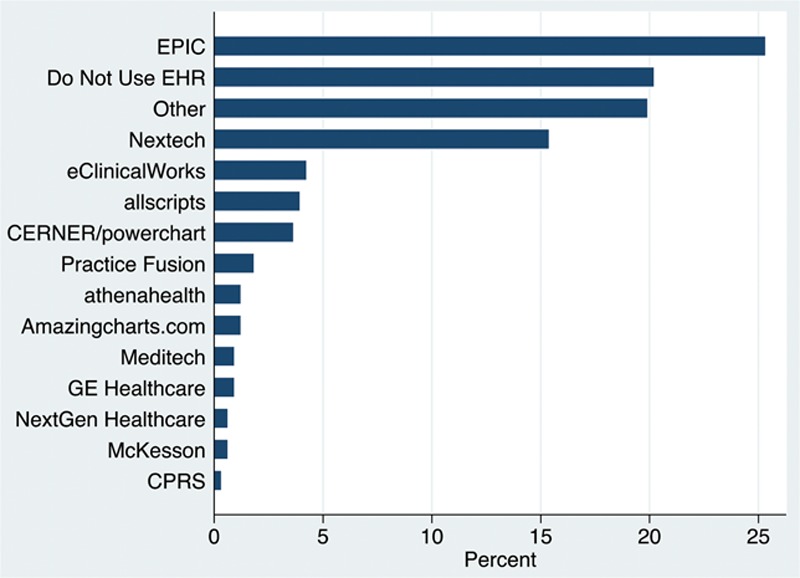
EHR vendors that respondents currently use.
Fig. 2.
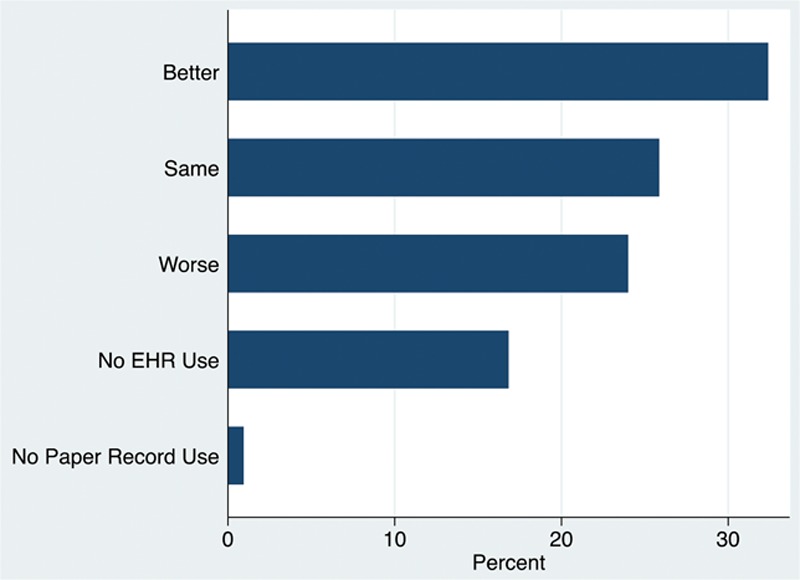
Respondents’ perceived effect of EHR on quality of care.
In addition, plastic surgeons who did not use EHR at all were found to be older than those who do use EHR (58.36 versus 51.23 years old, respectively). This could potentially be a result of younger surgeons being more accustomed to a technology-centered world, although this age gap was not so large that a significant generational gap could account for this trend. A similar gap related to years in experience between those who do not use EHR and those who do (24.60 versus 16.94 years, respectively).
EHR use within different plastic surgery subspecialties is summarized in Table 4. Plastic surgeons who primarily worked in esthetics are shown to use EHR less often when compared with those who did not specialize in esthetics (65.8% versus 93.2% of the time). Overall, those who practiced in esthetics had the lowest proportion of EHR use when compared with all other specialties. Conversely, plastic surgeons who specialized in microsurgery are shown to use EHR the most often (94.52% of the time).
Table 4.
EHR Use According to Practice Specialty
| Specialty Area | Practicing in Specialty Area Using EHR (%) | Not Practicing in Specialty Area Using EHR (%) | P |
|---|---|---|---|
| Esthetics | 65.78 | 93.24 | 0.000* |
| Burn | 85.71 | 69.83 | 0.032* |
| Craniofacial | 82.05 | 70.47 | 0.131 |
| General | 77.92 | 58.49 | 0.000* |
| Hand | 77.45 | 69.36 | 0.129 |
| Microsurgery | 94.52 | 65.53 | 0.000* |
| Pediatric | 78.43 | 70.63 | 0.254 |
| Other | 70.27 | 72 | 0.825 |
*Meeting statistical significance.
Among those who use EHR, we observed that certain surgeon characteristics were associated with positive and negative perceptions of EHR vendors (Table 5). On average, those who had a positive attitude toward EHR were younger than those who had a more negative attitude toward EHR (50.09 and 53.09 years old, respectively). In addition, surgeons with a negative attitude toward EHR were in practice longer than those with a positive attitude (18.98 versus 16.43 years, respectively). There was no statistically significant association between attitude toward EHR vendor and a recent change in EHR vendor (P = 0.054). Finally, it was found that surgeons had a more positive attitude toward their EHR vendor if data entry into the medical record was better shared among the support staff, rather than being the principle burden of the physician (51.8 versus 38.1 surgeons with a positive attitude, respectively).
Table 5.
Attitude toward Current EHR Vendor by Surgeon Characteristics
| Respondent Characteristics | Positive Attitude, n = 134, Mean (SD) | Negative Attitude, n = 125, Mean (SD) | No EHR Use, n = 42, Mean (SD) | P |
|---|---|---|---|---|
| Age | 50.09 (10.63) | 53.09 (10.01) | 58.16 (9.76) | 0.0002* |
| Years in practice | 16.43 (10.80) | 18.98 (10.21) | 24.72 (9.62) | 0.0001* |
| Recent change in EHR vendor, proportion | 0.054 | |||
| No change | 43.49 | 40.89 | 15.61 | |
| Change | 53.12 | 46.88 | 0 | |
| Who primarily enters data in medical record, proportion | 0.29* | |||
| Physician | 38.12 | 43.75 | 18.12 | |
| Support staff/shared responsibility | 51.8 | 38.13 | 10.07 |
*Meeting significance.
One hundred sixty-four respondents (47% of the total respondents) answered question 18, which allowed respondents to provide anonymous comments or concerns. Most respondents provided negative comments about EHR. In analyzing negative respondent comments, 15.10% (53 cases) focused on the amount of time wasted because of EHR, 8.60% (30 cases) emphasized the poor technical and information technology (IT) support or nonintuitive design of EHR as a dissatisfier, and 6.60% (23 cases) focused on the cost of adopting EHR. Although few of the comments made were positive, the majority at 5.10% (18 cases) were made with respect to how thorough documentation had become with the use of EHR.
DISCUSSION
The application of technology in medical settings continues to evolve and alter the practice of medicine in rapid fashion. EHRs, medical devices, and therapeutics routinely inundate the practice of medicine with challenges for dogmatic practices both for care and organization. The EHR is one such technologic advancement that has drastically shifted the ways in which physicians interact with patients and medical data. Medical culture is being radically being altered. Anecdotal experience and discussion suggest that plastic surgeons, physicians who inherently focus on patient perception and physical examination, are often dissatisfied with their EHR systems. In collaboration with ASPS, we sought to investigate the nationwide perceptions of EHR by surveying a large, diverse cohort of plastic surgeons from a variety of practice types.
To date, this is the first survey-based study specifically investigating the perception of EHR systems in the field of plastic surgery. Our final response rate was 14%, which was slightly higher than the average response rate for unsolicited member surveys deployed through ASPS Member Research Services.
We initially expected plastic surgeons using EHR to be more heavily represented by those physicians in academic medical centers as opposed to those respondents representing esthetic, private practice settings. Instead, we observed a diverse mix of practice types and specialties. Furthermore, previous studies indicated that adoption and the use of EHR among solo or private practice physicians were generally lower than that among practices with numerous physicians.8 In our study, this trend seemed to hold true and we found that lacking choice over the EHR system in use was a feature of not only academic medical centers but private practices as well. In addition, EPIC was the most commonly used vendor, but it was clear that many other vendors exist and were used by plastic surgeons. This may account for issues in cross-platform communication among plastic surgeons at differing practices. There also appeared to be no relationship between attitude toward EHR vendor and a recent change in EHR vendor. This was in direct contrast to initial beliefs that a recent change in vendor would cause a more negative attitude toward the vendor because lack of acclimation to the system could potentially influence attitude.
The primary limitation of this study is the relatively low 14% response rate, although this was still higher than the average for ASPS-sponsored surveys. The survey was deployed 3 spread out, separate times over a couple months, which could explain the overall low response rate. To supplement our demographic data, we could have also examined trends specific to differences in gender or geographic region. If we analyzed usage in relation to sex, we may have been able to elucidate potential social or professional pressures that could influence EHR usage in the clinic. However, plastic surgery is a heavily male-dominated specialty; thus, this modification to our study would require us to oversample the female plastic surgeons to draw any statistically significant data measuring the effect of sex on EHR usage and perception.20 Furthermore, questions that pertained more to personal aspects of the surgeon’s quality of life and specific to burnout may have elicited more responses overall and provided useful information related to the relationship of burnout and quality of life as they pertain to EHR use. A 2014 survey regarding burnout that was administered to 708 randomly sampled plastic surgeons from the ASPS national membership garnered a 71% response rate.21 This particularly high response rate could speak to the value of asking questions intimately more relevant to the plastic surgeon’s lifestyle.
Moving forward, training or attending plastic surgeons at academic medical centers could benefit substantially from fostering productive connections with EHR support staff or vendors. Ham et al19 reported decreased time spent preparing for rounds, more time spent in direct patient care, and even more time for educational activity among 23 surgery residents by using a tailored EHR tool made by health information technology developers and surgeons themselves. This sort of collaboration could potentially result in one of the intended effects of the EHR, which is to streamline the workflow of physicians and improve patient care.
In the adoption of any new technology, there is a fundamental learning curve built into its use. In some instances, this is called the “valley of death” in technology adoption. Users go through a period where efficiency predictably drops to a level worse than initial starting parameters. How the technology is adopted, learned, and assimilated into clinical practice can hasten this valley of death that is typically seen with the adoption of an EHR into a private practice or academic facilities. This survey taken at a period in time could very much reflect the valley of death seen in the adoption of a new platform of technology. What will be interesting to see is the sentiments observed and recorded as time moves forward and EHRs become ubiquitous across all practice types.
In addition, we could structure a follow-up survey to focus more on EHR and its effects on physician quality of life or physician burnout. Previous studies have highlighted how EHR has had the unintended effect of distancing physicians from their patients.18,22 Users complete overly extensive templates not to improve their delivery of care but to avoid malpractice lawsuits and other legal battles.11 The stress of having to meticulously document every detail about a surgery or clinical encounter has made maintaining “work-life balance” far too difficult to achieve among many physicians.16 This points to the potential efficacy of training medical scribes to relieve some of the burden that plastic surgeons feel in documenting everything they do in practice. Because the main objective of this study was to provide a thorough overview of EHR usage and perceptions in the plastic surgery community, we did not find it necessary to focus on burnout at length; however, it is a popular topic worthy of investigation in future surveys.
The road forward will undoubtedly include EHR because there is no going back toward a world of paper medical records. Regulatory forces in present time do not support this classical pathway. Iteration of the EHR by users and makers of the system will allow optimization of this electronic tool to improve and optimize healthcare delivery. Surveys such as this will allow all stakeholders to better understand the implementation of the EHR among patient, provider, and medical practices. It is critical that information is gleaned from both the user and the makers of these systems to further improve the overall quality of the system.
CONCLUSIONS
In this study, we found that EHR use was more common in academic-associated specialties and larger practice groups. Contrary to our initial predictions, age and practice had little association with perceptions of EHR usage. There were marginally more positive perceptions of EHR usage than negative. We recognized several key reasons for the negative perceptions, including the feeling of excessively wasted time and barriers to ease of use. Providing data entry assistance to plastic surgeons may partially alleviate the aforementioned issues; however, these results indicate that physicians should be involved, in some capacity, with the research and development needed to improve user interfaces, time management, and workflow with EHR.
Table 6.
Effect of EHR on the Following Aspects of Practice Proportions
| Aspects of Practice | Negative (%) | No Impact (%) | Positive (%) | Not Sure (%) |
|---|---|---|---|---|
| Chart review, n = 273 | 21.25 | 8.79 | 61.54 | 8.42 |
| Documenting, n = 271 | 30.63 | 8.86 | 54.24 | 6.27 |
| Prescribing medications, n = 272 | 14.71 | 24.26 | 50.74 | 10.29 |
| Clinical decision-making, n = 274 | 12.04 | 63.50 | 14.96 | 9.49 |
| Patient communication, n = 272 | 14.34 | 45.59 | 30.88 | 9.19 |
| Operating costs, n = 273 | 58.24 | 9.89 | 12.09 | 19.78 |
| Work flow, n = 272 | 50.74 | 11.76 | 29.04 | 8.40 |
Supplementary Material
Footnotes
Published online 24 April 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Tubaishat A. The effect of electronic health records on patient safety: a qualitative exploratory study. Informatics Heal Soc Care. 2017;44:79–91. [DOI] [PubMed] [Google Scholar]
- 2.Naam NH, Sanbar S. Advanced technology and confidentiality in hand surgery. J Hand Surg Am. 2015;40:182–187. [DOI] [PubMed] [Google Scholar]
- 3.Frazee R, Harmon L, Papaconstantinou HT. Surgeons’ perspective of a newly initiated electronic medical record. Proc (Bayl Univ Med Cent). 2016;29:21–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Squitieri L, Chung KC. Value-based payment reform and the Medicare access and children’s health insurance program reauthorization act of 2015: a primer for plastic surgeons. Plast Reconstr Surg. 2017;140:205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yanamadala S, Morrison D, Curtin C, et al. Electronic health records and quality of care: an observational study modeling impact on mortality, readmissions, and complications. Medicine (Baltimore). 2016;95:e3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmgren AJ, Adler-Milstein J, McCullough J. Are all certified EHRs created equal? Assessing the relationship between EHR vendor and hospital meaningful use performance. J Am Med Informatics Assoc. 2017;25:654–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inverso G, Flath-Sporn SJ, Monoxelos L, et al. What is the cost of meaningful use? J Oral Maxillofac Surg. 2016;74:227–229. [DOI] [PubMed] [Google Scholar]
- 8.Kokkonen EWJ, Davis SA, Lin HC, et al. Use of electronic medical records differs by specialty and office settings. J Am Med Informatics Assoc. 2013;20:33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kruse CS, Kothman K, Anerobi K, et al. Adoption factors of the electronic health record: a systematic review. JMIR Med Informatics. 2016;4:e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Inform. 2014;83:779–796. [DOI] [PubMed] [Google Scholar]
- 11.Palabindala V, Pamarthy A, Jonnalagadda NR. Adoption of electronic health records and barriers. J Community Hosp Intern Med Perspect. 2016;6:32643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin SA, Sinsky CA. The map is not the territory: medical records and 21st century practice. Lancet. 2016;388:2053–2056. [DOI] [PubMed] [Google Scholar]
- 13.Bush RA, Kuelbs C, Ryu J, et al. Structured data entry in the electronic medical record: perspectives of pediatric specialty physicians and surgeons. J Med Syst. 2017;41:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doberne JW, Redd T, Lattin D, et al. Perspectives and uses of the electronic health record among US pediatricians: a national survey. J Ambul Care Manage. 2017;40:59–68. [DOI] [PubMed] [Google Scholar]
- 15.Boland MV, Chiang MF, Lim MC, et al. ; American Academy of Ophthalmology Medical Information Technology Committee. Adoption of electronic health records and preparations for demonstrating meaningful use: an American Academy of Ophthalmology Survey. Ophthalmology. 2013;120:1702–1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Domaney NM, Torous J, Greenberg W. Exploring the association between electronic health record use and burnout among psychiatry residents and faculty: a pilot survey study. Acad Psychiatry. 2018;42:648–652. [DOI] [PubMed] [Google Scholar]
- 17.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516–529. [DOI] [PubMed] [Google Scholar]
- 18.Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO study. J Am Med Inform Assoc. 2014;21:e100–e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ham PB, III, Anderton T, Gallaher R, et al. Development of electronic medical record-based “rounds report” results in improved resident efficiency, more time for direct patient care and education, and less resident duty hour violations. Am Surg. 2016;82:853–859. [PubMed] [Google Scholar]
- 20.Halperin TJ, Werler MM, Mulliken JB. Gender differences in the professional and private lives of plastic surgeons. Ann Plast Surg. 2010;64:775–779. [DOI] [PubMed] [Google Scholar]
- 21.Streu R, Hansen J, Abrahamse P, et al. Professional burnout among US plastic surgeons: results of a national survey. Ann Plast Surg. 2014;72:346–350. [DOI] [PubMed] [Google Scholar]
- 22.McKenna KM, Hashimoto DA, Maguire MS, et al. The missing link: connection is the key to resilience in medical education. Acad Med. 2016;91:1197–1199. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


