Abstract
BACKGROUND:
Despite significant progress in primary prevention, the rate of myocardial infarction has not decreased in young adults. We sought to compare the risk factor profiles and outcomes between individuals who experienced a first myocardial infarction at a very young (≤40 years) and a young (age 41-50 years) age.
METHODS:
We evaluated all patients ≤50 years of age admitted with a Type 1 myocardial infarction to 2 large academic hospitals from 2000 to 2016. Risk factors were determined by review of electronic medical records. The primary outcomes of interest were all-cause and cardiovascular mortality.
RESULTS:
Among 2097 consecutive young patients with myocardial infarction, 431 (20.5%) were ≤40 years of age. When compared with their older counterparts, very young patients had similar risk profiles, with the exception of greater substance abuse (17.9% vs 9.3%, P < .001) and less hypertension (37.9% vs 50.9%, P < .001). Spontaneous coronary artery dissection was more prevalent in very young patients (3.1% vs 1.1%, P = .003). Over a median follow-up of 11.2 years, very young myocardial infarction patients had a similar risk of all-cause and cardiovascular mortality.
CONCLUSIONS:
Despite being, on average, 10 years younger and having a lower prevalence of hypertension, very young myocardial infarction patients had similar 1-year and long-term outcomes when compared with those aged 41 to 50 years at the time of their index infarction. Our findings suggest the need for aggressive secondary prevention measures in very young patients who experience a myocardial infarction.
Keywords: Premature coronary artery disease, Risk factors, Very young adults
INTRODUCTION
The incidence of myocardial infarction is increasing among younger individuals.1–3 While developing a myocardial infarction at an early age is significant, as there are more productive years of life at risk, the source of this phenomenon is not well understood. One possible explanation is the rising prevalence of conventional cardiovascular disease risk factors such as hypertension, dyslipidemia, diabetes, and smoking among younger individuals.4 Other studies focusing on young individuals, however, have explored the role of additional risk factors such as illicit substance use5 and hemostatic dysfunction.6
Nonetheless, even in studies focused on younger populations, few studies have specifically focused on individuals younger than age 40 suffering from a myocardial infarction,7,8 with most evaluating those younger than 50,9 55,1 or even 60 years of age.10 A better understanding of risk factors and outcomes among young patients is needed because age remains the dominant risk factor for 10-year atherosclerotic cardiovascular disease (ASCVD) risk prediction. In particular, the calculation of the ASCVD risk score and subsequent treatment with a statin are generally reserved for individuals over the age of 40 years, while for those under the age of 40 there is more emphasis on lifestyle interventions. Furthermore, it has been shown that current guidelines underestimate cardiovascular risk among individuals who developed a myocardial infarction at a young age.11
Therefore, our aim was to compare the baseline characteristics, risk factors, and outcomes of very young patients (age ≤40 years) who experienced a myocardial infarction with other, older patients (ages 41-50) within the Partners YOUNG-MI Registry. In addition, we evaluated angiographic characteristics of these patients to determine whether very young patients had a similar extent and severity of coronary artery disease when compared with those patients who were older at the time of their myocardial infarction.
METHODS
Study Population
The design of the YOUNG-MI registry has been previously described.9 In summary, this is a retrospective cohort study from 2 large academic medical centers (Brigham and Women’s Hospital and Massachusetts General Hospital) including all patients who experienced a first myocardial infarction at or prior to 50 years of age between the years 2000 and 2016. All medical records were adjudicated by a team of study physicians, as previously described9 using the Third Universal Definition of Myocardial Infarction.12 For the present analysis, only patients who experienced a Type 1 myocardial infarction on index admission were included. Individuals with known coronary artery disease (defined as a prior myocardial infarction or revascularization) were excluded from this analysis.
Risk Factors
The presence of cardiovascular risk factors was ascertained through a detailed review of electronic health records corresponding to the period of time up to and including the index admission. The definitions of all risk factors, household income, and the Charlson Comorbidity Index have been previously described and are detailed in the online supplement.9,11,13
Angiographic Findings
Invasive angiographic findings were ascertained through a review of cardiac catheterization images by a single interventional cardiologist blinded to all patient outcomes and risk factors. Both culprit lesions and nonculprit lesions were identified. For each lesion, the location and severity of stenosis (assessed visually, ranging from 20% to 100%) were classified.14
The extent of coronary artery plaque was determined by the segment involvement score (SIS) calculated as the total number of coronary artery segments exhibiting plaque, irrespective of the degree of luminal stenosis. For each patient, the SIS ranged from 0 to 16. Additionally, the Gensini score was used as a method of quantifying the overall severity of coronary stenosis while accounting for lesion location, as previously described.15 Patients with a Gensini score >20 (a score corresponding to approximately a single lesion of ≥70% in the proximal left anterior descending artery) were defined as possessing severe coronary artery disease.16
Outcomes
The primary outcomes of interest were all-cause and cardiovascular death. Vital status was assessed by means of the Social Security Administration Death Master File, the Massachusetts Department of Vital Statistics, and the National Death Index. Cause of death was adjudicated independently by 2 cardiologists, with instances of disagreement reviewed by an adjudication committee and decisions reached by consensus. Death was classified as cardiovascular or noncardiovascular, as per published criteria.9,17 If death certificates were not available, deaths were conservatively classified as noncardiovascular.
In an exploratory secondary analysis, we also evaluated the incidence of a short-term composite outcome comprised of all-cause mortality and re-infarction within 1-year post-myocardial infarction. Ascertainment of re-infarction was determined by review of all available records following the index admission. For an event to be classified as a re-infarction, discharge with a hospitalization diagnosis of myocardial infarction was required.18
Statistical Analysis
All analyses were performed using Stata version 15.1 (StataCorp, College Station, Texas). Categorical variables are reported as frequencies and proportions, and compared with chi-squared or Fisher’s exact tests, as appropriate. Continuous variables are reported as means or medians and compared with t-tests or Mann-Whitney U tests, as appropriate. The proportional hazards assumption was assessed by analyzing the Schoenfeld residuals. Survival curves were compared using the log-rank test.
To evaluate the impact of age on the 3 outcomes in question, individuals were stratified into 2 groups based on their age at the time of the index myocardial infarction. Specifically, those patients who were at or below the age of 40 years were classified as “very young,” while others, all aged 41 to 50, were classified as “young.” Univariate Cox proportional hazards modeling was performed for survival free from all-cause mortality, cardiovascular mortality, and a composite outcome consisting of all-cause mortality and re-infarction within 1-year post-myocardial infarction. In each case, multivariable adjustment was then made using all baseline covariates that had a significant (P ≤ .05) univariate association with the outcome in question. Individuals who died during their index hospital stay were excluded from both the univariate and multivariate analyses.
RESULTS
Proportion of Very Young Myocardial Infarction Patients
The cohort consisted of 2097 patients who experienced a Type 1 myocardial infarction, of whom 443 (21%) were at or below the age of 40 years (very young) at the time of their event (Table 1). The proportion of individuals presenting with a Type 1 myocardial infarction at or prior to the age of 40 increased over the study period (2000-2016), although the increase was statistically significant only during the last 10 years of the study (2007-2016), where there was an average increase of 1.7% per year (P for trend .022) (Figure 1).
Table 1.
Baseline Characteristics Stratified by Age at Index Myocardial Infarction
| Factor | 40 < Age ≤50 Years (n = 1666, 79%) | Age ≤40 Years (n = 431, 21%) | P Value |
|---|---|---|---|
| Demographics | |||
| Age at time of MI, median (IQR) | 46 (44, 48) | 36 (34, 39) | < .001 |
| Female | 317 (19.0%) | 87 (20.2%) | .59 |
| White | 1225 (73.5%) | 312 (72.4%) | .63 |
| Income (thousands $), median (IQR) | 71.4 (53.6, 87.4) | 71.6 (50.9, 85.5) | .060 |
| Insurance category | |||
| None | 148 (9.9%) | 43 (11.7%) | .15 |
| Public | 239 (16.0%) | 71 (19.2%) | |
| Private | 1107 (74.1%) | 255 (69.1%) | |
| ST-elevation myocardial infarction | 884 (53.1%) | 237 (55.0%) | .47 |
| Length of stay, median (IQR) | 3 (2, 5) | 3 (2, 6) | .95 |
| Risk factors | |||
| Hypertension | 841 (50.9%) | 161 (37.9%) | < .001 |
| Hyperlipidemia | 1519 (91.2%) | 391 (90.7%) | .77 |
| Diabetes mellitus | 335 (20.1%) | 81 (18.8%) | .54 |
| Premature CAD in 1st degree relative | 478 (28.7%) | 135 (31.3%) | .37 |
| Obesity | 591 (35.5%) | 159 (36.9%) | .58 |
| Current smoking | 844 (51.1%) | 222 (52.2%) | .68 |
| Alcohol use | 226 (13.7%) | 43 (10.1%) | .049 |
| Illicit substance use | 154 (9.3%) | 76 (17.9%) | < .001 |
| Marijuana use | 103 (6.3%) | 58 (13.7%) | < .001 |
| Cocaine use | 69 (4.2%) | 30 (7.1%) | .013 |
| Angina | 1444 (88.7%) | 393 (92.9%) | .012 |
| Peripheral vascular disease | 39 (2.4%) | 2 (0.5%) | .012 |
| ASCVD score, median (IQR) | 5.3 (3.2, 9.2) | 3.9 (1.9, 6.7) | < .001 |
| Charlson Comorbidity Index, mean (SD) | 1 (1, 2) | 1 (1, 2) | .099 |
| Laboratory values | |||
| Total cholesterol mg/dL, mean (SD) | 192.7 (57.1) | 190.6 (54.4) | .51 |
| HDL cholesterol mg/dL, mean (SD) | 37.3 (10.3) | 35.4 (9.9) | .001 |
| LDL cholesterol mg/dL, mean (SD) | 118.9 (46.4) | 119.9 (48.5) | .72 |
| Triglycerides mg/dL, median (IQR) | 150 (103, 223) | 148 (102, 225) | .71 |
| Creatinine mg/dL, median (IQR) | 1 (0.9, 1.1) | 1 (0.9, 1.1) | .13 |
| Estimated glomerular filtration rate mL/min/1.73 m2, mean (SD) | 78.9 (20.5) | 84.9 (22.3) | < .001 |
ASCD = atherosclerotic cardiovascular disease; CAD = coronary artery disease; HDL = high-density lipoprotein; IQR = interquartile range; LDL = low-density lipoprotein; MI = myocardial infarction.
Figure 1.
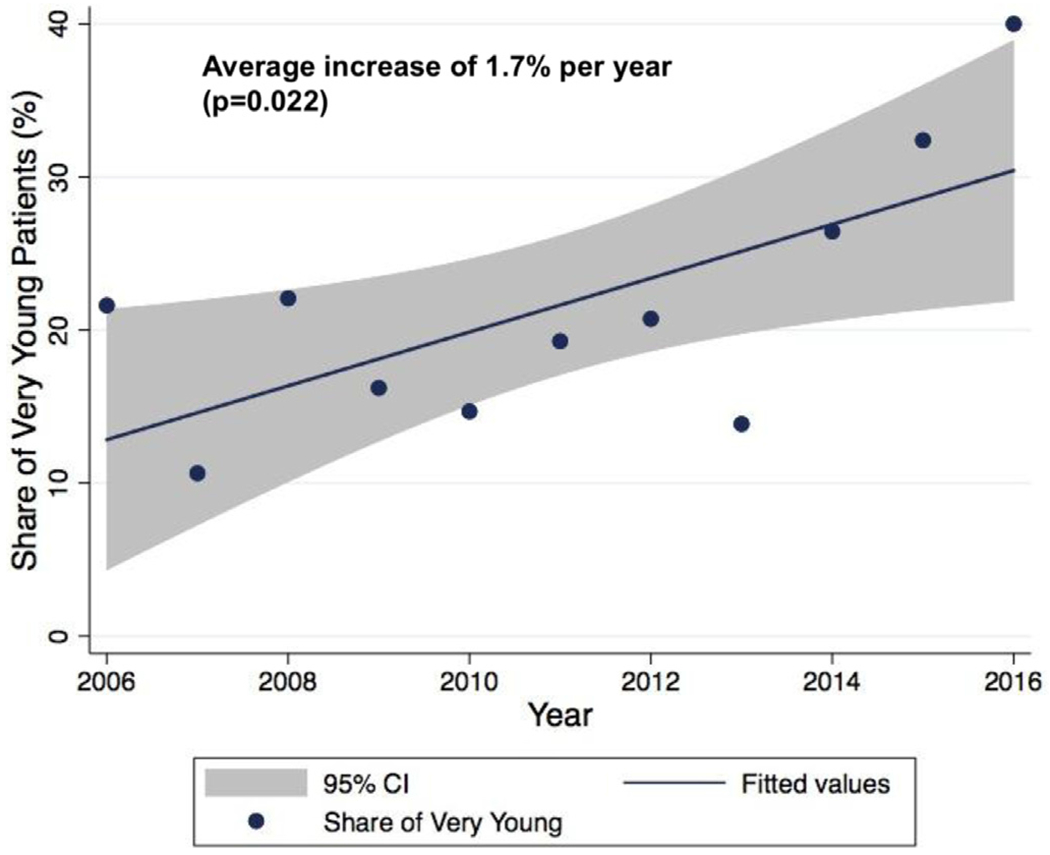
Trend in the percentage of very young presenting with myocardial infarction from 2006-2016.
Baseline Characteristics
The baseline characteristics of very young patients vs those who experienced their index myocardial infarction between the ages of 41 and 50 years are shown in Table 1. Patients who experienced their myocardial infarction at or below the age of 40 had a median age that was 10 years lower than that of their older counterparts (36 vs 46, P < .001). When compared with older patients, very young individuals were more likely to use both marijuana (P < .001) and cocaine (P = .013) and present with chest pain (P = .012). Conversely, patients aged 41 to 50 years upon admission were more likely to be diagnosed with hypertension (P < .001) or peripheral vascular disease (P = .012), use alcohol (P = .049), and have a higher ASCVD risk score (P < .001). A comparison of the full set of characteristics is provided in Table 1.
In-hospital cardiac procedures, including cardiac catheterization, coronary revascularization, and coronary artery bypass grafting, were similar across both groups (Table 2). While the use of antiplatelet therapies and beta-blockers, as well as angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers, was similar between the 2 groups, there was a small but statistically significant difference in the rate of aspirin (P = .011), statin (P = .017), and diuretic (P = .012) prescriptions upon discharge between very young and older members of the cohort (Table 2).
Table 2.
Medical Therapy Stratified by Age at Index Myocardial Infarction
| Factor | 40 < Age ≤50 Years (n = 1666, 79%) | Age ≤40 Years (n = 431, 21%) | P Value |
|---|---|---|---|
| Patient management | |||
| Cardiac catheterization | 1561 (93.7%) | 410 (95.1%) | .27 |
| Coronary revascularization | 1382 (83.0%) | 353 (81.9%) | .61 |
| Coronary artery bypass grafting | 147 (8.8%) | 30 (7.0%) | .21 |
| Factor | 40 < Age ≤50 Years (n = 1629, 79%) | Age ≤40 Years (n = 425, 21%) | |
| Medical therapy | |||
| Statin at discharge | 1465 (89.9%) | 365 (85.9%) | .017 |
| Statin intensity | |||
| None | 164 (10.1%) | 60 (14.1%) | .056 |
| Low intensity/unknown dose | 55 (3.4%) | 16 (3.8%) | |
| Moderate intensity | 619 (38.0) | 140 (32.9%) | |
| High intensity | 791 (48.6%) | 209 (49.2%) | |
| Ezetimibe | 19 (1.2%) | 7 (1.6%) | .43 |
| Aspirin at discharge | 1550 (95.2%) | 391 (92.0%) | .011 |
| P2Y12 inhibitor at discharge | 1338 (82.1%) | 338 (79.5%) | .22 |
| Beta-blocker at discharge | 1490 (91.5%) | 385 (90.6%) | .57 |
| ACE inhibitor/ARBs at discharge | 1002 (61.5%) | 265 (62.4%) | .75 |
| Diuretic at discharge | 192 (11.8%) | 32 (7.5%) | .012 |
ACE = angiotensin-converting enzyme; ARB = angiotensin II receptor blockers.
Invasive angiography was performed in 1985 patients (95%; Table 3). Single-vessel disease was more common in those who experienced their index myocardial infarction at or prior to the age of 40 years (56% vs 64%, P = .006). Spontaneous coronary artery dissection was also more prevalent among the very young (1.1% vs 3.1%, P = .003). Finally, those individuals at or under the age of 40 had lower extent of plaque, as measured by the SIS (P < .001), and lower overall plaque burden, as measured by the Gensini score (P = .035), than patients aged 41 to 50 years. The full set of angiographic findings can be found in Table 3.
Table 3.
Angiographic Findings Stratified by Age at Index Myocardial Infarction
| Factor | 40 < Age ≤50 Years (n = 1577, 79%) | Age ≤40 Years (n = 408, 21%) | P Value |
|---|---|---|---|
| Any plaque or stenosis | 1517 (97.2%) | 383 (96.2%) | .29 |
| Spontaneous dissection | 16 (1.1%) | 12 (3.1%) | .003 |
| Female | 14 (5.1%) | 11 (14.9%) | .009 |
| Male | 2 (0.2%) | 1 (0.3%) | .50 |
| MICAD | |||
| No obstructive CAD | 77 (4.9%) | 29 (7.1%) | < .001 |
| Single-vessel disease | 885 (56.1%) | 260 (63.7%) | |
| Multi-vessel disease | 615 (39.0%) | 119 (29.2%) | |
| Segment involvement score, median (IQR) | 3 (1, 4) | 2 (1, 3.5) | < .001 |
| Gensini score | |||
| Single-vessel disease | 32 (20, 47) | 32 (20, 43.5) | .83 |
| Multi-vessel disease | 58 (42, 83) | 56 (42, 88) | .65 |
| Total | 40 (24, 62) | 36.5 (20, 58) | .035 |
CAD = coronary artery disease; IQR = interquartile range; MICAD = myocardial infarction with CAD.
Long-Term Outcomes
All-cause death.
Of the original 2097 patients, 6 of the 431 patients (1.4%) classified as very young died during their hospital stay, compared with 37 (2.2%) of the patients aged 41 to 50 years at the time of their index admission (P = .49). The remaining 2054 patients had a median follow-up of 11.2 years, during which 36 (8.5%) of the very young patients and 175 (10.7%) of their older counterparts died (P = .17). The annual death rate post discharge among the very young was 0.85 deaths per 100 person-years, while the rate for the older members of the cohort was 1.06 deaths per 100 person-years (P = .23). Being at or below the age of 40 upon index admission had an unadjusted hazard ratio of 0.80 (95% confidence interval [CI], 0.56-1.15; P = .22) (Figure 2A). After adjusting for sex, income, presentation with ST-elevation myocardial infarction, length of stay, hypertension, diabetes mellitus, alcohol use, illicit substance use, angina, peripheral vascular disease, ASCVD risk score, Charlson Comorbidity Index (CCI), high-density lipoprotein, total triglycerides, creatinine, estimated glomerular filtration rate, cardiac catheterization, revascularization, and medications upon discharge, the hazard ratio (HR) remained nonsignificant (1.06; 95% CI, 0.69-1.64; P = .79) (Figure 2A).
Figure 2.
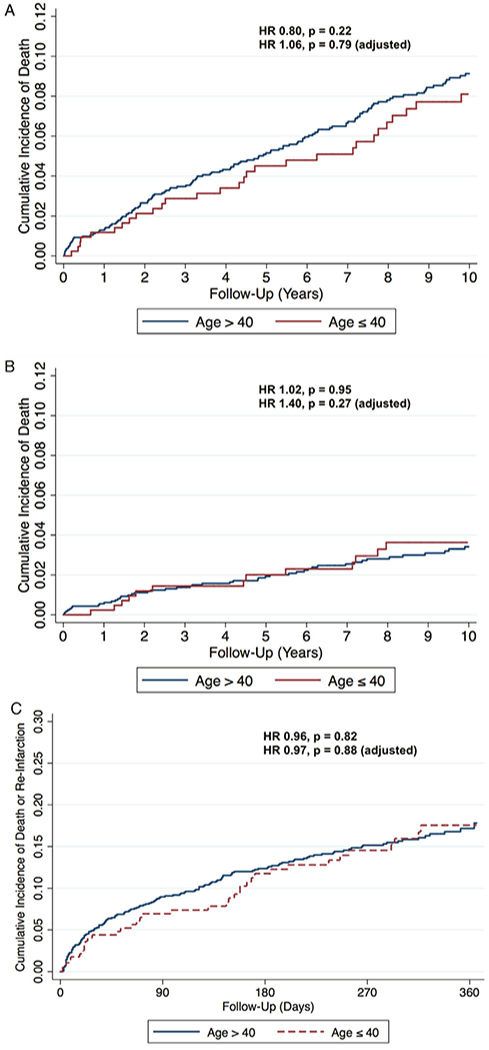
(A) Kaplan-Meier survival curves for all-cause mortality stratified by age at index myocardial infarction (MI). (B) Kaplan-Meier survival curves for cardiovascular mortality stratified by age at index MI. (C) Kaplan-Meier survival curves for the composite of all-cause mortality and reinfarction within 1-year post-MI stratified by age at index myocardial infarction.
Cardiovascular death.
Over the same follow-up period, very young individuals had a similar incidence of cardiovascular mortality post discharge compared with their older counterparts (4.2% vs 4.2%, P = 1.00). The cardiovascular death rate among those who experienced their myocardial infarction at or below the age of 40 years was 0.41 deaths per 100 person-years, while that of patients aged 41 to 50 was 0.42 deaths per 100 person-years (P = .93). The unadjusted hazard ratio of those experiencing a first myocardial infarction at or below the age of 40 was 1.02 (95% CI, 0.61-1.71; P = .95) (Figure 2B). Following adjustment for income, length of stay, hypertension, diabetes mellitus, obesity, alcohol use, illicit substance use, angina, peripheral vascular disease, ASCVD risk score, CCI, creatinine, estimated glomerular filtration rate, and medications upon discharge, the HR remained nonsignificant (1.40; 95% CI, 0.77-2.56; P = .270) (Figure 2B).
Short-Term Outcomes
Following discharge, 37 (8.7%) of the very young patients died or experienced a reinfarction within 1 year of their myocardial infarction, compared with 154 (9.5%) of those patients aged 41 to 50 years (P = .64). Those experiencing a myocardial infarction at or prior to the age of 40 had an unadjusted hazard ratio of 0.96 (95% CI, 0.67-1.37; P = .82) for the composite outcome of death or reinfarction (Figure 2C). After adjusting for the CCI, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, creatinine, cardiac catheterization, and coronary revascularization, the hazard ratio remained nonsignificant (0.97; 95% CI, 0.67-1.44, P = .879) (Figure 2C).
DISCUSSION
Among the 2097 patients who experienced a myocardial infarction at or prior to the age of 50 years, we found that approximately 21% were at or below the age of 40 at the time of hospitalization. These very young patients were similar to their older counterparts within our cohort in terms of their baseline characteristics, with the exception of a lower prevalence of hypertension and more frequent use of both marijuana and cocaine. While the 2 age groups were similar with respect to in-hospital cardiovascular procedures, younger patients were less likely to be prescribed aspirin or statins upon discharge. Finally, relative to the older members of the cohort, very young patients demonstrated less extensive coronary artery disease. However, despite being, on average, 10 years younger, having similar risk factor profiles, and having less coronary artery disease, younger patients had a similar incidence of both all-cause and cardiovascular mortality over a median follow-up of more than 11 years.
To the best of our knowledge, this is the largest study to compare the baseline characteristics, angiographic findings, and long-term outcomes of very young (age ≤40 years) and young (age 41-50) adults with myocardial infarction. Although a number of other studies have examined patients who experienced a myocardial infarction at a young age, they do not specify the upper age limit of the older or control group, often leading to comparisons between individuals who differ significantly in age.19–24 Even in those cases where very young individuals were compared with an intermediate-aged control group, not only was the division between the 2 groups higher at age 4525 or 50,26 but the upper limit of the control group was significantly higher.25,26 Moreover, among studies focused on myocardial infarction in younger patients, ours represents one of very few that have included long-term outcomes.19,27 Finally, our study is one of the largest to examine the angiographic findings encountered in such a patient population. In particular, prior works examining the angiographic characteristics of young patients with myocardial infarction have often been limited to samples of several hundred or fewer individuals.8,19,22
Clinical Implications
A concerning trend that we observed was a significant increase in the proportion of very young patients experiencing a myocardial infarction during the last 10 years of the study period. Because the overall burden of traditional risk factors was similar between very young and young patients, it is plausible that there are additional risk factors among the very young in our cohort. For example, in the present study, more substance use was detected among very young individuals who experienced a myocardial infarction. This is not only an important risk factor in very young adults,28 but one that seems to be increasing over time.5 However, the association between substance use and adverse outcomes can also be due to a correlation between substance use and other risky health-related habits (eg, sedentary behavior and poor diet).30 Another explanation for the excess risk in very young adults is a genetic predisposition; however, we would not expect the prevalence of this risk factor to change over time.29
In keeping with prior research, those patients who experienced their myocardial infarction at a very young age had a lower extent of coronary artery disease when compared with the older members of the cohort. 19,20,22 Additionally, we found that spontaneous coronary dissection was significantly more frequent in very young myocardial infarction adults, and mostly present in women. These findings are consistent with previous work, which has shown that spontaneous coronary dissection occurs at a mean age of 43 years, and mostly among young females.31
The vast majority of patients who experienced a myocardial infarction at or under the age of 40 years had a low ASCVD risk score prior to their event, and most had a low burden of traditional risk factors such as hypertension. These results highlight the challenges that are present in identifying risk in very young individuals and suggest that future research is needed to identify and treat cardiovascular risk in young adults, particularly those under the age of 40 who are only rarely candidates for statin therapy.
Limitations
The primary limitation of our study was its retrospective nature. However, this aspect provided us with the opportunity to examine a substantial number of individuals who experienced a myocardial infarction at a young age. A similar prospective study would have required at least 10 years to allow for the recruitment of the same number of patients. Our study was also restricted to those individuals who suffered a myocardial infarction. Therefore, it was not possible to examine either the prevalence of myocardial infarction within the full, at-risk population, or the relative rates of myocardial infarction among the 2 different age groups of at-risk individuals. In addition, we do not have data on genetics or lifestyle factors, which are known to be associated with cardiovascular risk, and which may be even more important in the determination of cardiovascular risk among younger individuals. Finally, in terms of methodology, our study was limited in that we relied on a visual analysis to determine the angiographic characteristics of all patients within the cohort. Although arguably less precise than a quantitative assessment of obstruction, visual assessment has been widely used in prior studies.
CONCLUSION
Despite being, on average, 10 years younger and having less extensive coronary artery disease, very young myocardial infarction patients had similar 1-year and long-term outcomes when compared with those who were aged 41 to 50 years. Our findings suggest the need for aggressive secondary prevention measures in very young patients who experience a myocardial infarction and underscore the need for future efforts to improve risk assessment among young adults, particularly those under the age of 40, who are only rarely candidates for statin therapy.
CLINICAL SIGNIFICANCE.
Despite comparable risk factor profiles, being, on average, 10 years younger, and having less extensive coronary artery disease, very young myocardial infarction patients (≤40 years of age) had a similar incidence of both all-cause and cardiovascular mortality over a median follow-up of more than 11 years.
Our findings suggest the need for aggressive lifestyle and pharmacological secondary prevention therapies among individuals who experience a myocardial infarction at a young age.
Acknowledgments
Funding: SD is supported by a T32 postdoctoral training grant from the National Heart, Lung, and Blood Institute (T32 HL094301). PN is supported by a grant from the National Heart, Lung, and Blood Institute (R01HL142711) and a Hassenfeld Scholar Award from the Massachusetts General Hospital. JLJ is supported in part by the Hutter Family Professorship.
Conflict of Interest: PN is a scientific advisor for Apple, and reports grant support from Amgen, Apple, and Boston Scientific. JLJ is a Trustee of the American College of Cardiology, has received grant support from Novartis Pharmaceuticals, Roche Diagnostics, Abbott, Singulex and Prevencio; consulting income from Roche Diagnostics, Critical Diagnostics, MyoKardia, Janssen and Novartis; and participates in clinical endpoint committees/data safety monitoring boards for Abbott, AbbVie, Amgen, Boehringer-Ingelheim, Janssen, and Takeda. DLB discloses the following relationships – Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, PhaseBio, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, TobeSoft; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim), Belvoir Publications (Editor-in-Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), HMP Global (Editor-in-Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Medtelligence/ReachMD (CME steering committees), Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, Eisai, Ethicon, Forest Laboratories, Idorsia, Ironwood, Ischemix, Lilly, Medtronic, PhaseBio, Pfizer, Regeneron, Roche, Sanofi Aventis, Synaptic, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Biotronik, Boston Scientific, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Fractyl, Merck, Novo Nordisk, PLx Pharma, Takeda. RB receives research support from Astellas Inc and Amgen Inc. The remaining authors have nothing to disclose.
SUPPLEMENTAL MATERIAL
Definition of Risk Factors
Diabetes was defined as having a fasting plasma glucose >126 mg/dL, a hemoglobin A1c ≥6.5%, or a documented diagnosis and/or treatment for diabetes. Hypertension was defined as a systolic blood pressure ≥140 mmHg, a diastolic blood pressure ≥90 mmHg, or a documented diagnosis and/or treatment of hypertension. Dyslipidemia was defined as having a total cholesterol ≥240 mg/dL, a serum triglyceride ≥150 mg/dL, a high-density lipoprotein (HDL) cholesterol <40 mg/dL in men or <50 mg/dL in women, or a documented diagnosis and/or treatment of dyslipidemia. Obesity was defined as having a body mass index (BMI) ≥30 kg/m2 or a documented diagnosis of obesity. Family history of premature CAD was defined as a fatal MI, a non-fatal MI, or a coronary revascularization occurring before 55 years of age in the case of first-degree male family members and before 65 years of age for first-degree female family members. Alcohol use was defined as having a positive toxicology report for alcohol during the index hospitalization or a documented diagnosis and/or treatment of alcohol use. Illicit substance use was defined as having a positive toxicology report during the index hospitalization for one or more of marijuana, cocaine, heroin, or methamphetamines or a documented diagnosis and/or treatment for use of these substances. Depression, anxiety, and psychotic disorders were defined as having a documented diagnosis and/or treatment for these conditions. In addition, we also calculated the atherosclerotic cardiovascular disease (ASCVD) risk score for each individual whenever possible.
In order to adjust for comorbidities, we calculated the Charlson Comorbidity Index (CCI), a method of predicting the risk of mortality based on co-morbidities, for each patient as determined by International Classification of Diseases, 9th Revision (ICD-9) diagnosis and billing codes associated with the index hospitalization.1 Additionally, because lower socioeconomic status is known to be associated with all-cause mortality, household income for each patient was estimated based on household zip codes in conjunction with the 2015 inflation adjusted median household income data provided by the US Census Bureau.2
References
1. Stagg V. CHARLSON: Stata module to calculate Charlson index of comorbidity2017.
2. U.S. Census Bureau. Median Household Income in the Past 12 Months (in 2015 inflation-adjusted dollars): U.S. Census Bureau; 2015.
References
- 1.Arora S, Stouffer GAR, Kucharska-Newton A, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction: the ARIC Community Surveillance Study. Circulation 2019;140(8):e331–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta A, Wang Y, Spertus JA, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol 2014;64(4):337–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390(10100):1151–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah N, Kelly AM, Cox N, Wong C, Soon K. Myocardial infarction in the “young”: risk factors, presentation, management and prognosis. Heart Lung Circ 2016;25(10):955–60. [DOI] [PubMed] [Google Scholar]
- 5.DeFilippis EM, Singh A, Divakaran S, et al. Cocaine and marijuana use among young adults with myocardial infarction. J Am Coll Cardiol 2018;71(22):2540–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davidson L, Wilcox J, Kim D, et al. Clinical features of precocious acute coronary syndrome. Am J Med 2014;127(2):140–4. [DOI] [PubMed] [Google Scholar]
- 7.Wiesbauer F, Blessberger H, Azar D, et al. Familial-combined hyperlipidaemia in very young myocardial infarction survivors (< or =40 years of age). Eur Heart J 2009;30(9):1073–9. [DOI] [PubMed] [Google Scholar]
- 8.Fournier JA, Cabezon S, Cayuela A, et al. Long-term prognosis of patients having acute myocardial infarction when </=40 years of age. Am J Cardiol 2004;94(8):989–92. [DOI] [PubMed] [Google Scholar]
- 9.Singh A, Collins B, Qamar A, et al. Study of young patients with myocardial infarction: Design and rationale of the YOUNG-MI Registry. Clin Cardiol 2017;40(11):955–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yandrapalli S, Nabors C, Goyal A, et al. Modifiable risk factors in young adults with first myocardial infarction. J Am Coll Cardiol 2019;73(5):573–84. [DOI] [PubMed] [Google Scholar]
- 11.Singh A, Collins BL, Gupta A, et al. Cardiovascular risk and statin eligibility of young adults after an MI: partners YOUNG-MI registry. J Am Coll Cardiol 2018;71(3):292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60(16):1581–98. [DOI] [PubMed] [Google Scholar]
- 13.Divakaran S, Singh A, Biery D, et al. Diabetes is associated with worse long-term outcomes in young adults after myocardial infarction: the partners YOUNG-MI registry [e-pub ahead of print]. Diabetes Care 2019. September 23 10.2337/dc19-0998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryan TJ, Bauman WB, Kennedy JW, et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American Heart Association/American College of Cardiology Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Committee on Percutaneous Transluminal Coronary Angioplasty). Circulation 1993;88(6):2987–3007. [DOI] [PubMed] [Google Scholar]
- 15.Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol 1983;51(3):606. [DOI] [PubMed] [Google Scholar]
- 16.Sinning C, Zengin E, Waldeyer C, et al. SYNTAX score-0 patients: risk stratification in nonobstructive coronary artery disease. Clin Res Cardiol 2016;105(11):901–11. [DOI] [PubMed] [Google Scholar]
- 17.Hicks KA, Tcheng JE, Bozkurt B, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol 2015;66(4):403–69. [DOI] [PubMed] [Google Scholar]
- 18.White HD, Reynolds HR, Carvalho AC, et al. Reinfarction after percutaneous coronary intervention or medical management using the universal definition in patients with total occlusion after myocardial infarction: results from long-term follow-up of the Occluded Artery Trial (OAT) cohort. Am Heart J 2012;163(4):563–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmerman FH, Cameron A, Fisher LD, et al. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry). J Am Coll Cardiol 1995;26(3):654–61. [DOI] [PubMed] [Google Scholar]
- 20.Schoenenberger AW, Radovanovic D, Stauffer JC, et al. Acute coronary syndromes in young patients: presentation, treatment and outcome. Int J Cardiol 2011;148(3):300–4. [DOI] [PubMed] [Google Scholar]
- 21.Morillas P, Bertomeu V, Pabon P, et al. Characteristics and outcome of acute myocardial infarction in young patients. The PRIAMHO II study. Cardiology 2007;107(4):217–25. [DOI] [PubMed] [Google Scholar]
- 22.Pineda J, Marin F, Roldan V, et al. Premature myocardial infarction: clinical profile and angiographic findings. Int J Cardiol 2008;126(1):127–9. [DOI] [PubMed] [Google Scholar]
- 23.Chua SK, Hung HF, Shyu KG, et al. Acute ST-elevation myocardial infarction in young patients: 15 years of experience in a single center. Clin Cardiol 2010;33(3):140–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bangalore S, Fonarow GC, Peterson ED, et al. Age and gender differences in quality of care and outcomes for patients with ST-segment elevation myocardial infarction. Am J Med 2012;125 (10):1000–9. [DOI] [PubMed] [Google Scholar]
- 25.Doughty M, Mehta R, Bruckman D, et al. Acute myocardial infarction in the young–the University of Michigan experience. Am Heart J 2002;143(1):56–62. [DOI] [PubMed] [Google Scholar]
- 26.Moccetti T, Malacrida R, Pasotti E, et al. Epidemiologic variables and outcome of 1972 young patients with acute myocardial infarction. Data from the GISSI-2 database. Investigators of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI-2). Arch Intern Med 1997;157(8):865–9. [PubMed] [Google Scholar]
- 27.Fullhaas JU, Rickenbacher P, Pfisterer M, et al. Long-term prognosis of young patients after myocardial infarction in the thrombolytic era. Clin Cardiol 1997;20(12):993–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ravi D, Ghasemiesfe M, Korenstein D, et al. Associations between marijuana use and cardiovascular risk factors and outcomes: a systematic review. Ann Intern Med 2018;168(3):187–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Natarajan P, Young R, Stitziel NO, et al. Polygenic risk score identifies subgroup with higher burden of atherosclerosis and greater relative benefit from statin therapy in the primary prevention setting. Circulation 2017;135(22):2091–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khera AV, Emdin CA, Drake I, et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med 2016;375 (24):2349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012;126(5):579–88. [DOI] [PubMed] [Google Scholar]


