Abstract
This study describes the availability of physical activity information in the electronic health record (EHR), explores how EHR documentation correlates with accelerometer-derived physical activity data, and examines whether measured physical activity relates to venous thromboembolism (VTE) prophylaxis use. Prospective observational data from community-dwelling older adults admitted to general medicine (n=65). Spearman’s correlations were used to examine association of accelerometer-based daily step count with documented walking distance and with duration of VTE prophylaxis. Only 52% of patients had walking documented in nursing and/or PT/OT notes during the first three hospital days. Median daily steps recorded via accelerometer was 1370 (IQR 854, 2387), and correlated poorly with walking distance recorded in PT/OT notes (median 33 feet/day (IQR 12, 100)), r=0.24, p=0.27). Activity measures were not associated with use or duration of VTE prophylaxis. VTE prophylaxis use does not appear to be directed by patient activity, for which there is limited documentation.
Keywords: Mobility, Older Adults, Inpatient, Electronic Health Record
Introduction
Prolonged periods of immobility during hospitalization are a contributor to functional decline and a marker of sicker individuals at risk for poor hospital outcomes (e.g., prolonged length of stay, falls, and discharge to skilled nursing facilities) (Covinsky, Pierluissi, & Johnston, 2011; Fisher, Graham, Ootenbacher, & Oster, 2010; Mudge et al., 2016). Interventions which increase the time spent walking during hospitalization have been shown to reduce the risk of death, in-hospital functional decline, and the need for post-acute care (Brown, Redden, Flood & Allman, 2009; Zisberg, Shadmi, Gur-Yaish, Tonkikh, & Sinoff, 2015). Some physician activity orders, such as “up ad lib” and “up with assist”, are meant to encourage out-of-bed activity, but it is unclear whether these translate to actual time out of bed. Brown and colleagues (2009), using body-worn accelerometers to continuously monitor patient activity during hospital stays, found that patients spent an average of 83% of their time in bed despite being able to walk independently. Incomplete physician awareness of actual walking activity (or inactivity) in the hospital could impact decision-making about fall safety, discharge planning, and risk for conditions such as delirium and venous thromboembolism (VTE).
The example of VTE is particularly salient because clinical practice guidelines explicitly recommend consideration of mobility status when making decisions about anticoagulant use. Many clinicians have adopted near-universal use of anticoagulants to prevent VTE; however, anticoagulation prophylaxis may not be beneficial or cost-effective in all cases as there is harm from bleeding in low-risk patients, and a costly component of hospital care for older adults is pharmacologic VTE prophylaxis (Decousus et al., 2011, Shorr, Jackson, Weiss, & Moores, 2007). The American College of Chest Physicians recommends discontinuing pharmacologic VTE prophylaxis once patient mobility is restored (Grade 2B recommendation), although a specific threshold is not specified (Linkins et al. 2012). We hypothesize that if clinical guidelines were being followed, number of steps would be negatively correlated with duration of VTE prophylaxis. Further, a proposed cause of VTE is venous stasis from bedrest and immobility. Early ambulation and progressive mobility interventions are encouraged to reduce bedrest and prevent VTE occurrence (Maynard, 2016). Despite the need for information about patient mobility, it is not clear how consistently activity data is collected and displayed in electronic health records (EHR). Here we examined 1) the availability of physical activity information in the EHR, 2) the correlation between available chart documentation and accelerometer-derived activity data, and 3) whether accelerometer-based activity relates to pharmacologic VTE prophylaxis use among medically ill, hospitalized older adults.
Methods
Subjects and Setting
Patients aged 60 years or older admitted to General Medicine at an academic medical center hospital were enrolled in a prospective cohort study from January 2016 through March 2017. A convenience sample was derived from a daily list of weekday general medicine admissions; weekend admissions were excluded as these patients could not be enrolled within 24 hours of hospital admission. Patients with activity orders of “strict bed rest” and those on contact and respiratory precautions were excluded because of expected limited activity. Additionally, patients with clear contraindications to pharmacologic VTE prophylaxis, on anticoagulation upon admission, receiving surgery during their hospital stay, and on observational status were excluded. All patients were enrolled within 24 hours of admission. Prior to enrollment, the aims of the research were reiterated, an opportunity to ask any questions was provided, and the informed consent form was signed. The Duke University institutional review board approved the study.
Chart documentation of activity
We reviewed the EHR from nursing, physical therapy (PT), and occupational therapy (OT) notes from the first three days of admission as decisions about VTE are typically made early in the course of hospitalization. Chart notes were reviewed for any documentation of out-of-bed mobility, walking activity, and walking distance (feet).
Accelerometer measurement of inpatient activity
We used the GT3x+ model ActiGraph (Pensacola, FL), a widely used triaxial accelerometer designed to measure and record physical activity. Accelerometers record the frequency and intensity of activity through raw acceleration signals. The ActiGraph has been validated in use among older adults with mobility limitations (Pruitt et al, 2008), and accelerometer step count reliability and accuracy has been validated in the inpatient setting (Brown, Roth & Allman, 2008). The ActiGraph was positioned on the ankle for all patients in our study to avoid interference with wrist intravenous lines and blood draws and because hospital gowns preclude secure placement around the hip. Accelerometers were applied within 24 hours of admission. Patients were instructed to wear the device continuously (even during sleep), removing only as needed for procedures, until the time of hospital discharge or for a maximum of seven days. The data collected from the accelerometer included: 1) time (hrs) spent in activity, 2) periods (hrs) of inactivity (sleep hours, sedentary), and 3) total number of steps.
Pharmacologic VTE prophylaxis use
Inpatient medication data for each day of hospitalization were abstracted from the EHR including class, name, route of administration, dose strength, and administration times. Low-molecular-weight heparin (LMWH), low-dose unfractionated heparin (LDUH), and fondaparinux were categorized as pharmacologic VTE prophylaxis. Although we collected data on mechanical VTE prophylaxis use, we did not include it in the analysis since guidelines are specific to only pharmacologic VTE prophylaxis use.
Analysis
Descriptive statistics were calculated for all variables, including physical activity information in the EHR defined as chart documentation of walking activity, accelerometer activity data, and use of pharmacological VTE prophylaxis. We examined correlations of total steps with 1) documented walking activity from patients’ charts and 2) duration of pharmacologic VTE prophylaxis, using the non- parametric Spearman’s correlation. Differences in activity time, sedentary time, and steps according to pharmacological VTE prophylaxis use were examined employing non-parametric analysis (Wilcoxon Rank-Sum tests) to deal with observed deviations from normality in these response variables. Due to severe deviation from normality for the length-of-stay measure, non-parametric analysis was also used. All analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC).
Results
There were 204 patients that met eligibility criteria and were approached for enrollment. Of these, 79 (39%) agreed to participate. Fourteen were excluded from subsequent analyses due to lack of accelerometer data. Therefore, a total of 65 patients with complete data were included in the final analysis.
Mean age for the sample was 73.4 years (SD 9.0); 43% were male and 20% were African-American, and median length of stay was 4.0 days (Table 1). Median activity time was 1.1 hrs/day (IQR 0.7, 1.7); Range 0.1 – 4.8 hrs/day). Medina time spent in sedentary activity (awake but not moving) was 14.8 hrs/day (IQR 12.4, 17.1); Range: 3 – 20 hrs/day). Median total daily step count was 1370 (IQR 854, 2387); Range: 86 – 6134 steps/day; Table 1, with single outlier excluded range: 86–5736). Accelerometers were worn for a mean of 4.1 days (SD 2.0), on average 64.8% of the day.
Table 1.
Patient Characteristics
| Overall sample, n= 65 | |
|---|---|
| Demographics | |
| Age, years | 73.4 ± 9.0 |
| Male | 28 (43) |
| African American | 13 (20) |
| Hospital Characteristics | |
| Length of stay, days, Median, (IQR) | 4 (2, 7) |
| Resident medicine care team | 43 (66) |
| Accelerometer Mobility Data | |
| Total time in activity, Median, (IQR)
(hours/day) range (0.08 – 4.8) |
1.1 (0.7, 1.7) |
| Total time sedentary, Median, (IQR)
(hours/day) range (3.4 – 20.6) |
14.8 (12.4, 17.1) |
| Total steps Median, IQR (steps/day) range (86 – 6134) |
1370 (854, 2387) |
| Chart Documentation of Mobilitya | |
| No Documentation of Mobility | 31 (48) |
| Nursing | 20 (31) |
| Physical Therapy/Occupational Therapy | 26 (40) |
| Documentation of walking distance | 23 (35) |
| # with PT/OT within first 3 days of Admission | 35 (54) |
| Venous Thromboembolism Prophylaxis | |
| Pharmacological | 40 (62) |
| Non-Pharmacological | 25 (38) |
| VTE Prophylaxis use duration, % of LOS, n=40 | 89 ± 21 |
Values represent mean (standard deviation), or number (%), unless otherwise indicated.
Totals add up to greater than 100% because documentation may have occurred in more than one location (e.g., nursing and PT/OT notes).
Chart Documentation of Activity
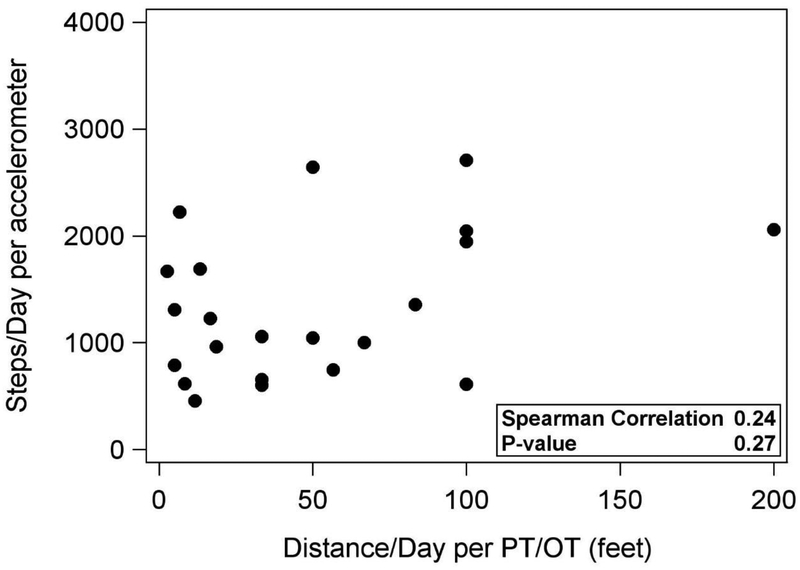
Within the first three days of admission, all participants had nursing notes and 54% had a PT or OT note. Only 52% (n=34) of patients had documentation of walking activity in nursing and/or PT/OT notes during the first three days of hospitalization. Walking distance though was not found in any nursing notes, whereas 35% (n=23) of patients had recorded walking distance in PT/OT notes (Table 1). Among those with recorded walking distance, the median daily distance recorded in the documentation was 33 feet (IQR 12, 100). The correlation of walking distance recorded in PT/OT notes with daily steps via accelerometer was r=0.34 (p=0.11). However, when a single outlier not representative of expected activity in hospitalized older adults was excluded (6134 steps/day), the correlation was r=0.24, p=0.27 (Figure 1).
FIGURE 1. Correlation between accelerometer step count and documented distance walked per day (with outlier excluded).
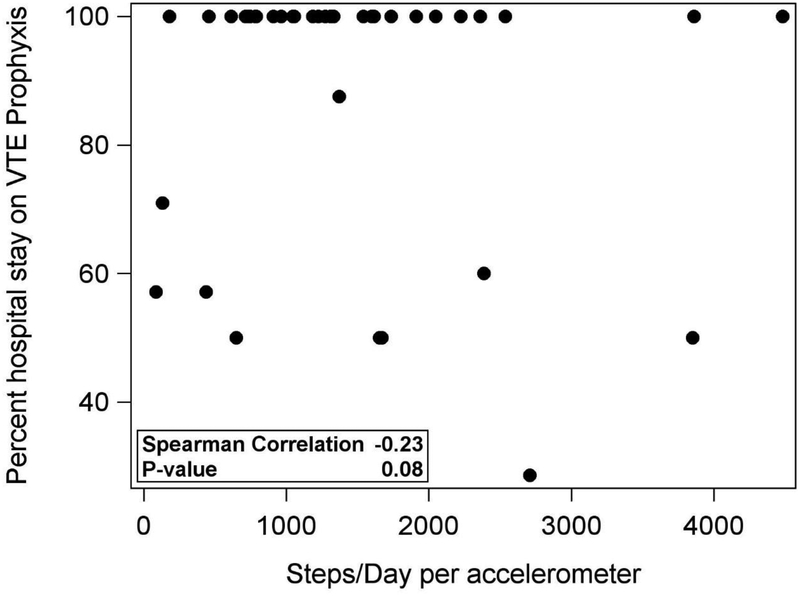
VTE prophylaxis use
Forty patients (62%) received pharmacological VTE prophylaxis during an average of 88.6% of their hospital stay (SD 46; Table 1). Patients receiving VTE prophylaxis had nearly 24 minutes less of activity time, 1 hour more of sedentary time, and 500 fewer steps per day than patients not receiving pharmacological VTE prophylaxis; these differences were not statistically significant. There was also no significant correlation between steps per day and duration of VTE prophylaxis (Table 2, Figure 2).
Table 2.
Mobility activity according to VTE prophylaxis use.
| Activity Variables | Pharm VTE PPX used (n = 40) | No Pharm VTE PPX used (n=25) | Wilcoxon p-value |
|---|---|---|---|
| Total time in activity (hours/day) | 1.0 (0.6, 1.5) | 1.2 (0.7, 1.8) | 0.2 |
| Total time sedentary (hours/day) | 14.8 (12.4, 17.1) | 14.4 (11.1, 16.9) | 0.4 |
| Total steps (steps/day) | 1320 (764, 2135) | 1809 (1126, 3207) | 0.1 |
Values represent median (interquartile range). PPX = prophylaxis, VTE = venous thromboembolism
FIGURE 2. Correlation between duration of pharmacologic VTE prophylaxis and accelerometer step count per day.
Discussion
Keeping patients up and moving is critical for preventing functional decline and reducing the risk of VTE. Our work and that of others suggest that hospitalized older adults spend 15–20 hours per day in sedentary activity and only 1 hour per day in standing or walking activity (Brown, Roth & Allman, 2008; Brown et al, 2009; Mudge et al, 2016). We observed limited documentation of walking in nursing and PT/OT notes and when it was present, there was poor correlation with accelerometer-measured step counts. Clinical guidelines recommend using mobility to guide patient selection and duration of pharmacologic VTE use (Linkins et al, 2012); however, we found no association between hospital activity and VTE prophylaxis.
One reason for the lack of correlation between chart-documented activity and accelerometer-measured activity is that documented walking activity in PT/OT notes represents only a fraction of all daily walking activity. For example, one patient with nearly 2000 steps/day of accelerometer-measured walking had only 10 feet/day of walking documented in PT/OT notes (Figure 1). Patients get an average of three PT/OT sessions per hospital stay (Young, Moonies, & Bungum, 2017) and much of this time is used for assessments, not necessarily walking activity. Therefore, whereas providers typically rely on chart documentation for knowledge of patients’ physical activity, PT/OT notes document only a fraction of daily activity. Our results suggest that there is very limited data on activity within the first three days of hospitalization to appropriately guide provider decision-making on important issues such as VTE prophylaxis.
One important clinical implication of poor activity awareness is its potential contribution to costly and inappropriate use of pharmacologic VTE prophylaxis in older adults (Pavon et al, 2018; Shorr et al, 2007). Use of pharmacologic VTE prophylaxis when not medically indicated may be harmful, especially for older adults who have a higher number of chronic conditions (Engbers, van Hylckama Vlieg, & Rosendall, 2010), take a higher number of potentially interacting medications (Pasina et al, 2013), and have higher risk of bleeding (; Decousus et al., 2011) than their younger counterparts. Clinician assessment of activity level is important for determining VTE risk in older adult inpatients and should factor into the decision for use and duration of pharmacologic VTE prophylaxis. For instance, although orders for “bed rest” are uncommon in patients hospitalized for medical illness, clinicians may still order VTE prophylaxis if they do not feel confident the patient will actually get out of bed and walk.7 This is supported by our finding that among patients who received pharmacologic VTE prophylaxis (n=40), the duration of use was 80% of their hospital stay regardless of activity level (Figure 2). If clinical guidelines were adhered to, we would have expected higher step counts to be associated with shorter duration of VTE prophylaxis.Alternatively, clinicians may fail to order VTE prophylaxis based on the false assumption that a patient with “ad lib” activity orders will walk enough to decrease the risk of VTE. These two clinical scenarios illustrate the importance of physical activity awareness, and they may explain why we did not find an association between patient activity and VTE prophylaxis use. Enhanced activity awareness could help improve appropriate pharmacologic VTE prophylaxis use as well as prevent VTE occurrence through physical activity. Early mobility and progressive ambulation can prevent VTE occurance by reducing venous stasis, which results from bedrest and immobility. Better activity awareness can also improve other key areas of hospital care such asdelirium reduction, falls prevention screening, and the identification of target patients for mobility intervention. A recent observational study found that a threshold of 900 steps was associated with functional decline in the hospital (Agmon et al, 2017), but more data is needed to determine clinically meaningful thresholds and differences in hospital activity levels.
We propose several steps to improve communication about hospital physical activity within the EHR: 1) Work toward consensus on how physical activity should be measured and reported in the hospital. The American Geriatrics Society Quality and Performance Measurement Committee recently called for consensus regarding mobility assessment by promoting assessments that are well-validated and provide actionable data (Wald et al., 2018). Decisions on measurement should involve input from key disciplines including nursing, PT/OT, and hospital medicine. 2) Measurement and reporting of patient activity needs to fit into the usual workflow (Bates et al, 2003). There first needs to be consensus on who should measure activity (nursing vs. PT/OT vs. both) so that it can be integrated into workflow and EHR documentation templates. This will ease the burden of activity assessment (Bates et al., 2003; Wald et al., 2018).Future qualitative work should examine how providers (clinicians, nurses, and physical and occupational therapists) prefer to interface with physical activity information so that interpretable structured data elements can be created. 3) Re-design of EHR applications can help bring physical activity information to end-users, such as clinicians, at the appropriate time. Documentation of activity may be in places in the chart that are not easily accessible to clinicians. It is not enough for the information needed by a provider to be available in the system (Bates et al., 2003)—EHR applications must anticipate clinician needs. For example, the placement of clinical guidelines and structured data on activity onto a single screen at the time the clinician orders VTE prophylaxis is likely to be impactful. 4) Mobile health (mHealth) technology, such as wearable accelerometers, can facilitate the acquisition, measurement, and reporting of walking activity during hospitalization. High-quality studies using implementation science are needed to understand how this technology can contribute to better communication and awareness about activity and improved clinical patient outcomes.
Limitations of this study include the relatively small sample size and involvement of only general medicine patients from a single health system. Further, although accelerometer reliability and accuracy has been validated in the inpatient setting, the use of a single ankle-worn device misses capturing other important physical activity measures, such as distance traveled and caloric expenditure. Despite these limitations, the findings may facilitate the development of interventions to improve activity documentation and adherence to clinical guidelines for VTE prophylaxis in hospitalized older adults.
Conclusions
Limited activity data is available in the EHR to guide clinical decision-making, such as VTE prophylaxis decisions. VTE prophylaxis use does not appear to be directed by patient activity, and documented activity correlates poorly with objective activity. Future work is needed to understand barriers and facilitators to activity documentation. Key next steps involve the development of consensus on who should measure activity, how it should be measured, and what source to use to gather that activity data, as well as the optimization of EHR elements, such as structured data fields and clinical decision tools, to facilitate awareness and communication about activity during hospitalization and to improve patient outcomes.
Funding Acknowledgements
This work was supported by the NIA GEMSSTAR Award (R03AG048007; Pavon); Duke Older Americans Independence Center (NIA P30 AG028716-01); Duke University Internal Medicine Chair’s Award; Duke Hartford Center of Excellence; The Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) at the Durham VA Health Care System (CIN 13-410; Hastings); T. Franklin Williams Scholars Program (Pavon); K24 NIA AG049077-01A1 (Colon-Emeric). The funding sources had no role in the design and conduct of the study, analysis or interpretation of the data, preparation or final approval of the manuscript before publication, or decision to submit the manuscript for publication.
Footnotes
Declaration of Conflicting Interests
The Authors declare that there is no conflict of interest.
References
- 1.Agmon M, Zisberg A, Gil E, Rand D, Gur-Yaish N, & Azriel M (2017). Association between 900 steps a day and functional decline in older hospitalized patients. JAMA Internal Medicine, 177(2), 272–274. [DOI] [PubMed] [Google Scholar]
- 2.Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, Spurr C, Khorasani R, Tanasijevic M, & Middleton B (2003). Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. Journal of the Medical Informatics Association, 10 (06), 523–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown CJ, Roth DL, & Allman R,M (2008). Validation of the use of wireless monitors to measure levels of mobility during hospitalization. Journal of Rehabilitation Research & Development, 45, 551–558 [DOI] [PubMed] [Google Scholar]
- 4.Brown CJ, Redden DT, Flood KL, & Allman RM (2009). The underrecognized epidemic of low mobility during hospitalization of older adults. Journal of the American Geriatrics Society, 57(9), 1660–1665. [DOI] [PubMed] [Google Scholar]
- 5.Covinsky KE, Pierluissi E, & Johnston CB (2011). Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA, 306(16), 1782–1793. [DOI] [PubMed] [Google Scholar]
- 6.Decousus H, Tapson VF, Bergmann JF, Chong BH, Froehlich JB, Kakkar AK, Merli GJ, Monreal M, Nakamura M, Pavanello R, Pini M, Piovella F, Spencer FA, Spyropoulos AC, Turpie AG, Zotz RB, Fitzgerald G, & Anderson FA (2011). IMPROVE Investigators. Factors at admission associated with bleeding risk in medical patients: findings from the IMPROVE investigators. Chest, 139(1):69–79. [DOI] [PubMed] [Google Scholar]
- 7.Engbers MJ, van Hylckama Vlieg A, & Rosendaal FR (2010). Venous thrombosis in the elderly: incidence, risk factors and risk groups. J Thromb Haemost. 8(10):2105–12. [DOI] [PubMed] [Google Scholar]
- 8.Fisher SR, Kuo YF, Graham JE, Ottenbacher KJ, & Ostir GV (2010). Early ambulation and length of stay in older adults hospitalized for acute illness. Archives of Internal Medicine, 170(21), 1942–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Linkins LA, Dans AL, Moores LK, Bona R, Davidson BL, Schulman S, & Crowther M. American College of Chest Physicians. (2012). Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest, 141(2 Suppl), e495S–530S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maynard G Preventing hospital-associated venous thromboembolism: a guide for effective quality improvement, 2nd ed. Rockville, MD: Agency for Healthcare Research and Quality; August 2016. AHRQ Publication No. 16–0001-EF. [Google Scholar]
- 11.Mudge AM, McRae P, McHugh K, Griffin L, Hitchen A, Walker J, Cruickshank M, Morris NR, & Kuys S (2016). Poor mobility in hospitalized adults of all ages. Journal of Hospital Medicine, 11(4), 289–291. [DOI] [PubMed] [Google Scholar]
- 12.Pasina L, Djade CD, Nobili A, Tettamanti M, Franchi C, Salerno F, Corrao S, Marengoni A, Iorio A, Marcucci M, & Mannucci P (2013). Drug-drug interactions in a cohort of hospitalized elderly patients. Pharmacoepidemiology and Drug Safety, 22(10),1054–1060. [DOI] [PubMed] [Google Scholar]
- 13.Pavon JM, Sloane RJ, Pieper CF, Colon-Emeric CS, Cohen HJ, Gallagher D, Morey MC, McCarthy M, Ortel TL, & Hastings SN (2018) Poor Adherence to Risk Stratification Guidelines Results in Overuse of Venous Thromboembolism Prophylaxis in Hospitalized Older Adults. Journal of Hospital Medicine,13(6), 403–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pruitt LA, Glynn NW, King AC, Guralnik JM, Aiken EK, Miller G, & Haskell WL (2008). Use of accelerometry to measure physical activity in older adults at risk for mobility disability. Journal of Aging and Physical Activity, 16(4):416–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shorr AF, Jackson WL, Weiss BM, & Moores LK (2007). Low-molecular weight heparin for deep vein thrombosis prophylaxis in hospitalized medical patients: results from a cost-effectiveness analysis. Blood Coagulopathy & Fibrinolysis, 18(4), 309–316. [DOI] [PubMed] [Google Scholar]
- 16.Wald HL, Ramaswamy R, Perskin MH, Roberts L, Bogaisky M, Suen W, & Mikhailovich A Quality and Performance Measurement Committee of the American Geriatrics Society. (2018). The Case for Mobility Assessment in Hospitalized Older Adults: American Geriatrics Society White Paper Executive Summary, Journal of the American Geriatrics Society. doi: 10.1111/jgs.15595. [DOI] [PubMed] [Google Scholar]
- 17.Young DL, Moonies S, & Bungum T (2017). Cross-Sectional Examination of Patient and Therapist Factors Affecting Participation in Physical Therapy in Acute Care Hospital Settings. Physical Therapy, 97(1), 3–12. [DOI] [PubMed] [Google Scholar]
- 18.Zisberg A, Shadmi E, Gur-Yaish N, Tonkikh O, & Sinoff G (2015). Hospital-associated functional decline: the role of hospitalization processes beyond individual risk factors. Journal of the American Geriatrics Society, 63(1), 55–62. [DOI] [PubMed] [Google Scholar]