Abstract
Purpose
To describe ICU stay, selected management aspects, and outcome of Intensive Care Unit (ICU) patients with traumatic brain injury (TBI) in Europe, and to quantify variation across centers.
Methods
This is a prospective observational multicenter study conducted across 18 countries in Europe and Israel. Admission characteristics, clinical data, and outcome were described at patient- and center levels. Between-center variation in the total ICU population was quantified with the median odds ratio (MOR), with correction for case-mix and random variation between centers.
Results
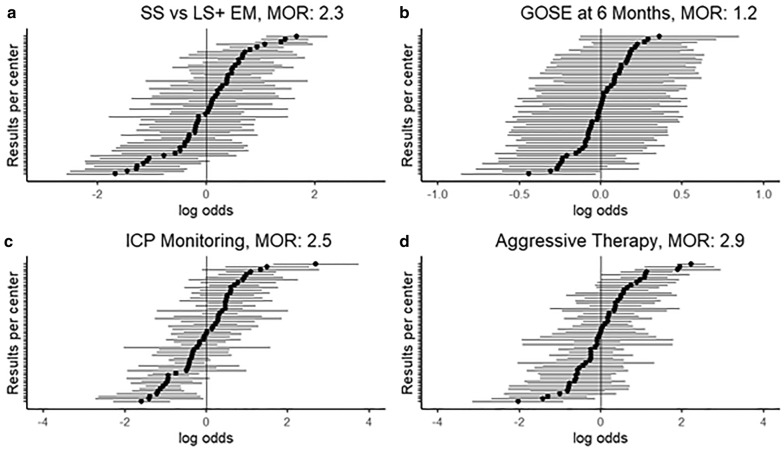
A total of 2138 patients were admitted to the ICU, with median age of 49 years; 36% of which were mild TBI (Glasgow Coma Scale; GCS 13–15). Within, 72 h 636 (30%) were discharged and 128 (6%) died. Early deaths and long-stay patients (> 72 h) had more severe injuries based on the GCS and neuroimaging characteristics, compared with short-stay patients. Long-stay patients received more monitoring and were treated at higher intensity, and experienced worse 6-month outcome compared to short-stay patients. Between-center variations were prominent in the proportion of short-stay patients (MOR = 2.3, p < 0.001), use of intracranial pressure (ICP) monitoring (MOR = 2.5, p < 0.001) and aggressive treatments (MOR = 2.9, p < 0.001); and smaller in 6-month outcome (MOR = 1.2, p = 0.01).
Conclusions
Half of contemporary TBI patients at the ICU have mild to moderate head injury. Substantial between-center variations exist in ICU stay and treatment policies, and less so in outcome. It remains unclear whether admission of short-stay patients represents appropriate prudence or inappropriate use of clinical resources.
Electronic supplementary material
The online version of this article (10.1007/s00134-020-05965-z) contains supplementary material, which is available to authorized users.
Keywords: Intensive care unit, Traumatic brain injury, Intracranial pressure, Outcome
Take-home message
| Patients with traumatic brain injury admitted to intensive care units are older and often less severe than in previous studies. Substantial between-center variation exists in ICU admission and treatment policies across Europe. |
Introduction
Traumatic brain injury (TBI) causes a social and economic global burden with about 82,000 deaths in Europe every year [1]. Patients with severe TBI often receive a highly intensive and multidisciplinary approach to prevent or mitigate both secondary brain injury and systemic complications [2]. For less severe TBI cases (without severe extracranial injury), clinicians have to estimate whether they will benefit from ICU admission, since guidelines with high-level evidence on ICU admission criteria are lacking. ICU admission is costly, and might also potentially be inappropriate for the patient, with risk of overtreatment and ICU-related complications, such as infections from multi-resistant bacteria [3].
In previous studies, intensive care admission was described merely for the most severe TBI cases, typically young male victims of high-energy road traffic incidents. In high-income countries, however, the aging population and the reduction of road traffic incidents have led to important changes in TBI epidemiology, which now includes older patients, who are often victims of falls, and present with frequent co-morbidities but less severe brain injury. Recent data suggest that the landscape of TBI in Europe is changing and that, correspondingly, ICU admission policies may have been modified, including a larger proportion of milder TBI patients [4, 5].
The aims of this study were:
to provide a general description of ICU stay, selected management aspects and outcome in TBI patients across Europe and,
to quantify variation across centers.
Methods
CENTER-TBI study
The Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI study, registered at clinicaltrials.gov NCT02210221), entails a longitudinal prospective collection of TBI patient data across 63 centers in Europe and Israel between December 19, 2014 and December 17, 2017. Inclusion criteria were: (1) clinical diagnosis of TBI; (2) indication for a brain CT scan; and (3) presentation to the hospital within 24 h post-injury. The presence of a severe preexisting neurological disorder, potentially confounding outcome assessment, was the only exclusion criterion. The CENTER-TBI study was approved by the medical ethics committees of all participating centers and informed consent from the patient or legal representative was obtained according to local regulations [4, 6].
ICU population and data collection
All patients directly admitted from the Emergency Room or transferred within 24 h of injury from another hospital to the ICU were analyzed [4]. Patients who deteriorated at the trauma, neurological or neurosurgical ward and were (re)admitted to the ICU were not included. Clinical data were collected at ICU admission, during ICU stay and at ICU discharge. For the current study, we extracted data on demographics, injury, imaging, admission, monitoring, treatment, and outcome characteristics. Patients were stratified using baseline GCS scores as mild (GCS 13–15), moderate (GCS 9–12), or severe TBI (GCS < 9) [4].
ICP and ICP-lowering treatments
Intracranial pressure and cerebral perfusion pressure (CPP) values were collected every 2 h. Intracranial hypertension was defined as a value above 20 mmHg, while 60 mmHg was chosen as a threshold for low CPP. To quantify the intensity of ICP-targeted therapies, a recently updated and validated version of the therapy intensity level (TIL) scale was used [7]. This scale summarizes in a score the number and the intensity of treatments. In addition, we analyzed the use of aggressive treatments for raised ICP as hypothermia, intense hypocapnia, barbiturates and decompressive craniectomy.
Outcome
Outcome was measured at 6 months after injury using the Glasgow Outcome Scale-Extended (GOSE), administered by interview or postal questionnaire. The categories ‘vegetative state (GOSE 2)’ and ‘lower severe disability (GOSE 3)’ were combined, resulting in a seven-point ordinal scale.
Statistical analysis
Patient characteristics are described as mean and standard deviation (SD) or as median and interquartile range (IQR). We defined three groups: early deaths (died within ≤ 72 h of ICU admission), short stay (≤ 72 h in the ICU) and long stay (> 72 h in the ICU). Patient characteristics, treatments and outcome were compared between these groups with χ2 tests for categorical variables, and ANOVA and t tests for continuous variables. We used the IMPACT Core model to calculate expected mortality and proportion with unfavorable outcome (GOSE < 5).
The variation between centers was quantified using random-effect logistic and ordinal regression models with a random intercept for center, and expressed as the median odds ratio [8] for:
The proportion of patients with a short stay (≤ 72 h in the ICU) versus long stay (> 72 h) and early deaths (≤ 72 h).
The proportion of cases having received ICP monitoring. Also, a sensitivity analysis of the proportion of cases having received ICP monitoring in a subset of patients with a GCS < 8 and CT abnormalities was performed.
The use of aggressive ICP-lowering treatments (any use of decompressive craniectomy, metabolic suppression, hypothermia therapy or intensive hypocapnia).
6-month GOSE outcome.
The MOR is a measure of variation in treatments or outcomes between hospitals that is not explained by factors in the model or attributable to chance. The MOR is related to τ2, which is the variance of the random effects:
The MOR can be interpreted as the odds ratio for comparing two randomly selected centers. For example, a MOR equal to one indicates no differences between centers. If there is considerable between-center variation, the MOR will be large. For example, a MOR of 2 for a certain treatment indicates that if two TBI patients with the same injury severity and characteristics presented to two random centers in our sample, one patient will have an over twofold probability to receive that treatment. To adjust for differences in baseline risk, we included the variables from the International Mission for Prognosis and Analysis of Clinical Trials in TBI (IMPACT) lab prognostic model [9] and any major extracranial injury [defined as an Abbreviated Injury Scale (AIS) > 3] [10]. The likelihood ratio test was used to determine the significance of the between-center variation, comparing a model with and without a random effect for center. The corresponding p values require a mixture distribution since the null hypothesis is on the boundary of the parameter space) [11].
Statistical analyses were performed in the R statistical software [12]. Multiple imputation was used to handle missing values, with use of the mice package in R [13]. These analyses were based on Version 2.0 of the CENTER-TBI core dataset, accessed using a bespoke data management tool, ‘Neurobot’ (http://neurobot.incf.org; RRID: SCR_01700).
Results
Patient characteristics
A total of 4509 patients were enrolled in the CENTER-TBI study, 2138 of whom were admitted to the ICU and included in this study. Patients were mostly men (73%). The median age was 49 years (IQR 29–65). A minority were children younger than 18 years (132, 6%), 552 (26%) were older than 65 years and 94 (4%) older than 80 years. Patients with severe TBI constituted 48% of the ICU admissions, while 720 cases (36%) were classified as mild. Major extra-cranial injuries were present in 1174 (55%) patients. (Table 1). More than half of the 54 ICUs have a neuro-ICU available (35, 65%). The median number of ICU beds available was 35 (28–45). Thirty-eight ICUs had a step-down unit available (70%). (Table S1) The median number of ICU patients recruited was 28 with an IQR of 15–50 (range 1–140). The median length of stay for the entire ICU cohort was 11 (IQR 3–26) days.
Table 1.
Baseline characteristics
| Total 2138 |
Short stay 636 |
Long stay 1372 |
Early deaths 128 |
p value | |
|---|---|---|---|---|---|
| Age (median (IQR)) | 49 (29–65) | 48 (28–64) | 49 (29–64) | 62 (40–75) | < 0.001 |
| ≥ 65 years | 552/2138 (26%) | 153/636 (24%) | 337/1372 (25%) | 62/128 (48%) | < 0.001 |
| ≥ 80 years | 94/2138(4.4%) | 29/636 (4.6%) | 52/1372 (3.8%) | 13/128 (10%) | 0.003 |
| Male sex | 1562/2138 (73%) | 443/636 (70%) | 1023/1372 (75%) | 94/128 (73%) | 0.07 |
| Severity TBI | < 0.001 | ||||
| Mild | 720/2009 (36%) | 394/607 (65%) | 319/1285 (25%) | 6/116 (5.2%) | |
| Moderate | 328/2009 (16%) | 107/607 (18%) | 213/1285 (17%) | 8/116 (6.9%) | |
| Severe | 961/2009 (48%) | 106/607 (18%) | 753/1285 (59%) | 102/116 (88%) | |
| Pupillary reactivity | < 0.001 | ||||
| Both reacting | 1636/2016 (81%) | 564/606 (93%) | 1040/1287 (81%) | 31/122 (25%) | |
| Both unreacting | 246/2016 (12%) | 16/606 (2.6%) | 150/1287 (12%) | 80/122 (65%) | |
| One reacting | 134/2016 (6.6%) | 26/606 (4.3%) | 97/1287 (7.5%) | 11/122 (9%) | |
| Hypoxia | 266/1981 (13%) | 38/593 (6.4%) | 191/1266 (15%) | 37/121 (31%) | < 0.001 |
| Hypotension | 267/1992 (13%) | 36/595 (6.1%) | 189/1274 (15%) | 42/122 (34%) | < 0.001 |
| ISS [median (IQR)] | 29 (25–41) | 24 (16–29) | 34 (25–43) | 58 (28–75) | < 0.001 |
| Any major extracranial injury (AIS ≥ 3) | 1174/2138 (55%) | 283/636 (45%) | 823/1372 (60%) | 67/128 (53%) | < 0.001 |
| CT characteristics | |||||
| Marshall CT classification | < 0.001 | ||||
| I | 204/1854 (11%) | 110/566 (19%) | 90/1179 (7.6%) | 3/108 (2.8%) | |
| II | 889/1854 (48%) | 330/566 (58%) | 553/1179 (47%) | 6/108 (5.6%) | |
| III | 152/1854 (8.2%) | 19/566 (3.4%) | 105/1179 (8.9%) | 28/108 (26%) | |
| IV | 28/1854 (1.5%) | 4/566 (0.7%) | 17/1179 (1.4%) | 7/108 (6.5%) | |
| V/VI | 581/1854 (31%) | 103/566 (18%) | 414/1179 (35%) | 64/108 (59%) | |
| Epidural hematoma | 369/1854 (20%) | 120/566 (21%) | 234/1179 (20%) | 15/108 (14%) | 0.22 |
| tSAH | 1347/1854 (73%) | 318/566 (56%) | 930/1179 (79%) | 99/108 (92%) | < 0.001 |
| Contusion | 1032/1854 (56%) | 244/566 (43%) | 730/1179 (62%) | 58/108 (54%) | < 0.001 |
| Acute subdural hematoma | 911/1854 (49%) | 192/566 (34%) | 633/1179 (54%) | 86/108 (80%) | < 0.001 |
| Midline shift | 404/1854 (22%) | 77/566 (14%) | 281/1179 (24%) | 54/108 (50%) | < 0.001 |
| Basal cistern absent or compressed | 586/1854 (32%) | 81/566 (14%) | 415/1179 (35%) | 94/108 (87%) | < 0.001 |
This table shows the baseline characteristics for short stay (stay ≤ 72 h), long stay (stay > 72 h), and early deaths (≤ 72 h). p values from ANOVA and Chi-square statistics for continuous and categorical characteristics, respectively
AIS Abbreviated Injury Scale, tSAH traumatic subarachnoid hemorrhage
ICU mortality and discharge rates were high in the first 72 h, but declined over time (Figs. 1, 2 ). There were 128 (6%) early deaths, 636 (30%) short-stay, and 1372 (64%) long-stay cases (Fig. 2).
Fig. 1.
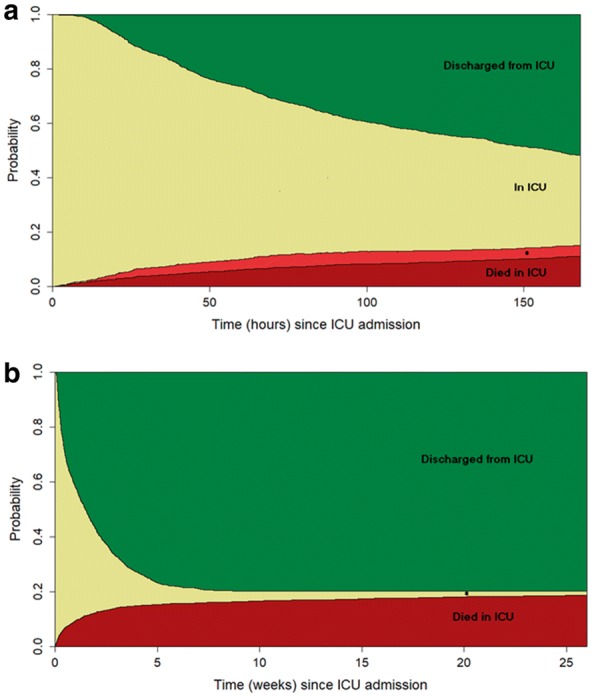
ICU patient flow over time. a Plot of the dynamic states of patients with TBI that were admitted to the ICU during the first seven days after ICU admission. The y-axis represents the probability to be in one of the possible states (i.e., alive or dead or discharged from ICU) at each time point from ICU admission. *Died after ICU discharge. b Plot of the dynamic states of patients with TBI that were admitted to the ICU during the first 6 months after ICU admission. The y-axis represents the probability to be in one of the possible states (i.e., alive or dead or discharged from ICU) at each point from ICU admission. *Still in ICU
Fig. 2.
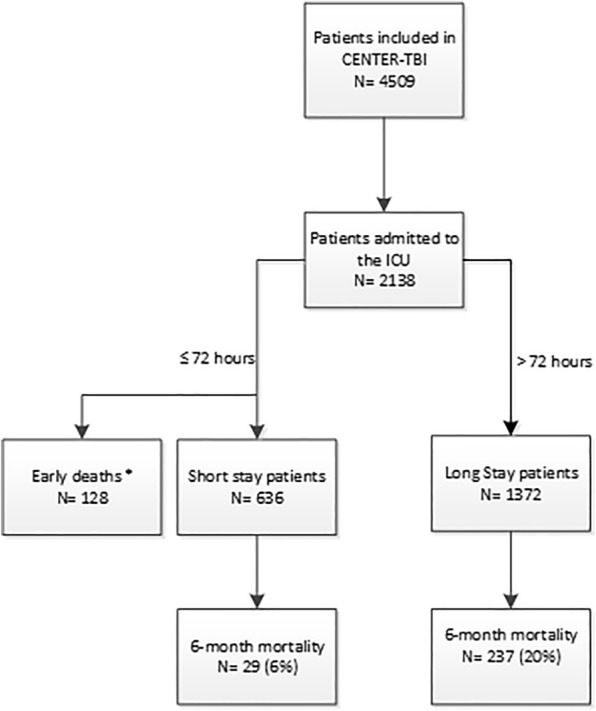
Flowchart of ICU patients. This figure shows the flow of patients at the ICU, based on their length of stay. *Patients who died within 72 h at the ICU
Early death patients had a higher median age (62 years) and more severe injuries, both intracranial and extracranial, compared to survivors. Demographic features were comparable between short-stay and long-stay groups, while significant differences were identified with respect to injury severity, CT findings, and pre-admission insults (Table 1). The main cause of mortality in early death patients was due to initial head injury (78, 81%) (Fig. S2).
The most frequent reasons for admission in short-stay patients were the need for frequent neurological observations (340; 54%) and mechanical ventilation (154; 24%) (Fig. S3). The long-stay patients included 319 patients (25%) classified as mild TBI in whom similar reasons for admission were mentioned (the need for neurological observations (152, 48%), mechanical ventilation (96, 30%).
Monitoring and treatment
Mechanical ventilation for at least 24 h was most often applied in long-stay patients and in patients who died early, when compared to short-stay patients (1164 [85%] and 91 [71%]; versus 201 [32%], respectively). A large difference was found in the use of ICP monitoring between long-stay and short-stay cases (837; 62% versus: 41; 7%, respectively). The main indication for ICP monitoring in short-stay patients was surveillance after intracranial operation (31, 76%). Invasive blood pressure monitoring was used in the majority of long-stay patients (1227; 90%) and in early deaths (113; 89%); but less frequently (388; 62%) in short-stay patients (Table S2).
Both neurosurgical interventions and extracranial surgery were more common in long-stay patients (634; 47% and 467; 34%, respectively) when compared to short-stay patients (139; 22% and 122; 19%, respectively). Patients in the short stay group rarely (≤ 5%) received aggressive ICP treatments (i.e., decompressive craniectomy, metabolic suppression, hypothermia, or intensive hypocapnia) (Table S2).
Complications and outcome
Long-stay patients suffered more complications compared with short-stay patients: most commonly ventilator acquired pneumonia (276; 21% versus 3; 0.5%) and cardiovascular complications (125; 9.3% versus 9; 1.5). The overall median hospital length of stay was 11 days (IQR: 3.4–26), while the median hospital length of stay for long-stay patients was 18 days (IQR: 7.7–35). When compared to long-stay patients, short-stay patients were less often discharged to a step-down unit (86 [14%] vs 255 [21%], respectively), and more often transferred to the ward (486 [78%] versus 616 [51%]). Long-stay patients were also often discharged to other hospitals (174; 14%) and rehabilitation units (95; 8%); while, other discharge locations (such as home, other ICU, or nursing home) were rare (Table 2).
Table 2.
Outcome and complications
| Total 2138 |
Short stay 636 |
Long stay 1372 |
p value | |
|---|---|---|---|---|
| Outcomes | ||||
| 6-month mortality | 394/1846 (21%) | 29/531 (5.5%) | 237/1187 (20%) | < 0.001 |
| 6-month unfavorable outcome (GOSE < 5) | 795/1846 (43%) | 77/531 (15%) | 590/1187 (50%) | < 0.001 |
| Hospital length of stay in days (median (IQR)) | 11 (3.4–26) | 6.3 (3–11) | 18 (7.7–35) | < 0.001 |
| Discharge location from ICU | < 0.001 | |||
| General ward | 1102/1840 (60%) | 486/623 (78%) | 616/1216 (51%) | |
| Home | 15/1840 (0.8%) | 11/623 (1.8%) | 4/1216 (0.3%) | |
| Nursing home | 4/1840 (0.2%) | 2/623 (0.3%) | 2/1216 (0.2%) | |
| Other | 36/1840 (2%) | 5/623 (0.8%) | 30/1216 (2.4%) | |
| Other hospital | 201/1840 (11%) | 27/623 (4.3%) | 174/1216 (14%) | |
| Other ICU | 43/1840 (2.3%) | 3/623 (0.5%) | 40/1216 (3.3%) | |
| Rehab unit | 98/1840 (5.3%) | 3/623 (0.5%) | 95/1216 (7.8%) | |
| Step-down/high-care unit | 341/1840 (19%) | 86/623 (13.8%) | 255/1216 (21%) | |
| Complications at the ICU | ||||
| Ventilator acquired pneumonia | 280/2090 (13%) | 3/616 (0.5%) | 276/1347 (21%) | < 0.001 |
| Cardiovascular complications | 155/2091 (7.4%) | 9/616 (1.5%) | 125/1348 (9.3%) | < 0.001 |
| Meningitis | 49/2090 (2.3%) | 0/616 (0%) | 48/1347 (3.6%) | < 0.001 |
| Seizures | 121/2089 (5.8%) | 17/616 (2.8%) | 99/1346 (7.4%) | < 0.001 |
This table shows the outcomes and ICU complications for patients surviving more than 72 h after ICU admission. The data are shown for short-stay (stay ≤ 72 h) or long-stay (stay > 72 h) patients. Early deaths are not included in this table as these patients represent the outcome in itself (death) and follow-up cannot be described. The categories ‘vegetative state (GOSE 2)’ and ‘lower severe disability (GOSE 3)’ were combined resulting in a seven-point ordinal scale’. p values from ANOVA and Chi-square statistics for continuous and categorical characteristics, respectively
GOSE Glasgow outcome scale extended, ICU intensive care unit, IQR interquartile range
In-hospital mortality for the ICU stratum was 15%; and at 6 months, mortality rose to 21% (data available for 1846 cases), which was lower than the expected mortality based on the IMPACT model (30%). Six-month mortality was higher in the long-stay-patient group compared with the short-stay group (20% versus 5.5%) (Fig. 3, Table 2).
Fig. 3.
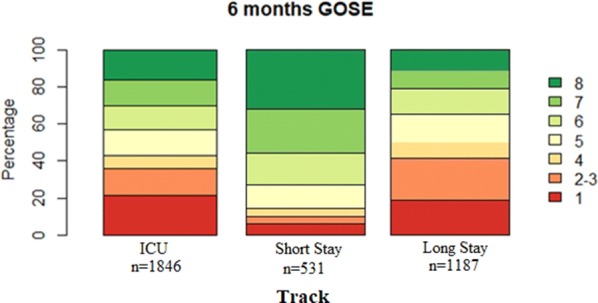
Six-month Glasgow outcome scale extended. This figure shows the distribution of the functional outcomes at the GOSE after 6 months for all ICU patients, short-stay patients, and long-stay patients
An unfavorable outcome at 6 months (GOSE < 5) was observed in 43% in the total ICU stratum, 50% (590) in long-stay group, and in 15% in short-stay group (77). The unfavorable outcome rate in the total ICU stratum was similar to the expected rate based on the IMPACT model (49%).
Between-center differences
Substantial between-center differences were found in the proportion of short stay, long stay and early deaths (MOR: 2.3, p < 0.001, Fig. 4). When adjusted for case-mix and random variation, between-center variation in the proportions of patients in the short-stay versus long-stay and early death groups was still substantial (MOR: 2.3, p < 0.001).
Fig. 4.
Between-center differences in ICU policies and outcome. This panel shows the adjusted differences (adjusted for case-mix with the IMPACT prognostic model) between centers by considering. a The proportion of patients with a short stay (≤ 72 h in the ICU) versus long stay (> 72 h) and early deaths (≤ 72 h); long stay and early deaths were treated as one group, since they resemble more severe patients and we aimed to study the proportion in each center of short-stay patients that were discharged alive within 72 h. b GOSE at 6 months for total ICU population. c ICP monitoring. d Aggressive therapy (any use of decompressive craniectomy, metabolic suppression, hypothermia therapy or intensive hypocapnia during ICU stay). A random-effect regression model was used to correct for random variation and adjusted for case-mix severity using the IMPACT variables and the presence of any major extracranial injury. The MOR reflects the between-center variation; a MOR equal to 1 represents no variation, the larger the MOR, the larger the variation. Significant differences (p value < 0.001) are present for data shown in a, c, and d for b (p = 0.01). GOSE Glasgow Outcome Scale extended, ICP intracranial pressure, MOR median odds ratio
Regarding ICP monitoring, after adjustment for case-mix, substantial and significant between-center variation persisted in the use of ICP monitoring (MOR: 2.5, p < 0.001, Fig. 4). A sensitivity analysis (with a subset of patient with a GCS ≤ 8 and CT abnormalities) confirmed this between-center variation (MOR: 2.6, p < 0.001). After case-mix adjustment, significant between-center differences were also found in the use of aggressive therapies (MOR: 2.9, p < 0.001, Fig. 4).
Between-center variation in outcome was smaller compared to the variation in treatment. The MOR in the total ICU population for six-month GOSE was 1.2 (p = 0.01, Fig. 4).
Discussion
The aims of this study were to describe ICU admission policies, selected management aspects, and outcome in TBI patients across Europe both at the patient and center levels. A substantial proportion of patients admitted to the ICU were classified on presentation as having a mild or moderate TBI. This is in strong contrast with historical TBI series, such as the USA Traumatic Coma Data Bank study [14] and other studies [15]. However, those series included only severe TBI patients, so that any evaluation of the general ICU admission policies at that time for milder cases is impossible. A more recent study, which analyzed data from 1648 mild TBI patients in 11 US level I trauma centers, showed that about 24 percent of them required admission to the ICU at some stage [16].
Even when compared to these latter data, our findings indicate quite liberal ICU admission rates for less severe cases. This is consistent with the strategies declared by the majority of centers participating in CENTER TBI. When centers were asked (in the Provider Profiling survey; see [5]) if they would admit “patients with a Glasgow Come Score (GCS) between 13 and 15 without CT abnormalities but with other risk factors”, 68% of responders reported this as consistent with their center policy.
Among the cases admitted, we looked at three different patient groups. Around 6% of patients died in the first 3 days after admission, with clearly severe intracranial and extra-cranial injuries. Patients in this group were significantly older, and only approximately half of those with documented intracranial mass lesions in this group received an operation. In survivors, we studied two distinct groups: those with a brief transition through the ICU and the second characterized by a prolonged ICU treatment. We selected the first 72 h as criterion to separate these two patient streams, triggered by the high ICU discharge rate during the first 3 days. This separation identified patients with different clinical characteristics, care pathways, and outcomes: long-stay patients were more severely injured, required more frequent invasive monitoring (including ICP) and therapies (both surgical and medical), and suffered a worse outcome. In contrast, short-stay patients were less severely injured, received less monitoring and treatments, and achieved better outcomes. The most frequently indicated reasons for ICU admission in this latter group were the need for strict neurological observation and mechanical ventilation (which, however, was continued for at least 24 h only in a third of cases). This may reflect current policy of early intubation at the scene of accident, and/or during initial assessment and evaluation. Cranial and extra-cranial surgery could also have been alternative indications for a short period of intense post-operative observation in the ICU.
These data can be interpreted in one of the two ways. On the one hand, the observed practice may represent a prudent strategy, offering close surveillance and assistance to patients at relatively low risk, but with the opportunity to ensure consistently good outcomes. The risk of deterioration in mild TBI is low but non-negligible. A recent meta-analysis, including 45 studies (for a total of 65,724 patients), estimated a 12% incidence of neurological deterioration and 3.5% neurosurgical intervention in mild TBI (characterized as GCS 13–15) [17]. Alternatively, the observed admission strategies may represent costly over-triage, because the ICU is an expensive resource, which should be used wisely. The fact that 11 patients in the short-stay group were discharged home directly from the ICU raises strong reservations on their need for intensive care. A previous study in mild TBI patients in the ICU in the USA showed that 17% of cases were over-triaged, with over triaged patients defined as “ICU stay ≤ 1 day; hospital stay ≤ 2 days; no intubation; no neurosurgery; and discharged to home” [18]. Our data on ICU admission of mild TBI patients are partially concordant with these findings, and while they do not permit accurate cost–benefit analysis, they clearly indicate a trend in ICU admission policies that deserves attention.
After adjustment for case-mix and random variation between centers, we found significant between-center proportion of short-stay patients discharged alive within 72 h. This confirms the results of earlier studies that found large variation in admission and discharge policies, primarily for mild TBI patients [5, 18]. This variation might reflect various factors: a search towards more individualized management [2], a lower adherence to guidelines [19], different availability of resources, or various combinations of these different factors. As for monitoring and management variations among centers, heterogeneity was not unexpected: previous studies [19–21] and surveys [22–24] found profound dissimilarities between centers in monitoring and treatment policies similar to our study.
The MOR for outcome between centers (1.2) was significant (p = 0.01), but smaller than the MOR for case-mix, ICP monitoring and aggressive therapies (2.5–2.9). This may reflect the small proportion of outcome variance modifiable by differences in management, and/or that differences in individual aspects of management may be discordant and make any outcome impact less easily detectable. Further, between-center variations in outcome that we demonstrated were smaller than previously reported [25, 26]. This may be because previous analyses were based on older data, collected across multiple studies, and heterogeneity in time and location explained the larger outcome variance in these older reports. It is also possible that over time, a more homogeneous standard of treatment has evolved in Europe and Israel.
Strengths and limitations
The CENTER-TBI study is unique for its extensive data collection in multiple centers, enrolling TBI patients with varying injury severity across a wide range of European centers. Limitations include that we focused on the ICU while an individual patient’s fate, and policies of the center at which treatment is delivered, depends on the continuum of care (from pre-hospital to rehabilitation). Second, the centers differed in their ICU characteristics, which might potentially contribute to between-center differences in ICU stay, treatment and outcome. In addition, we might have missed some important case-mix variables in the models that might have contributed to differences between centers (instead of true differences in policies). Third, the low number and non-consecutive enrolment in some centers could result in non-representative recruitment with reference to local ICU admission policy and introduce selection bias. Finally, all centers participating in CENTER TBI are characterized by their commitment to TBI research. They might represent a selected sample of the neuro-trauma centers in Europe limiting generalizability.
Future directions
The observed between-center differences in ICU policies require further research on whether these differences impact patient outcome. Comparative effectiveness research (CER) can be used for this purpose [27], requiring adequate covariate adjustment to account for confounders, and adjustment for other treatment policies that might differ between the centers. Variation in ICU performance also provides opportunities for future benchmarking and quality initiatives.
Conclusions
Our results confirm that the current ICU patient population admitted with Traumatic Brain Injury across Europe has changed, compared to previous data, and now includes older patients and a substantial proportion of mild and moderate cases. Sub-populations of patients (which we defined as short-stay, long-stay, and early mortality groups), are clearly different in injury severities, indications for ICU admission, care pathways, ICU resource utilization, and outcome. Our per-center analysis identified differences in the proportion of short-stay patients and interventions, for instance in the use of ICP monitoring and aggressive therapy, while there were only small differences in outcome.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (JPEG 21 kb) Figure S1: Length of ICU stay. A Length of Stay at the ICU for all patients (n = 2138). B Length of Stay at the ICU for the first 7 days, stratified by ICU mortality (data available for 1130 patients)
Supplementary material 3 (JPEG 51 kb) Figure S2: Cause of Mortality in Early Death Group. This figure shows the cause of mortality in the early death patients (N = 96) Only one reason per patient could be entered by clinicians
Supplementary material 4 (JPEG 27 kb) Figure S3: Reason for ICU admission for short-stay patients. This figure shows the reasons for ICU admission for the short-stay patients (N = 631). Only one reason per patients could be entered by clinicians
Acknowledgements
The authors would like to thank all patients for their participation in the CENTER-TBI study. The authors would like to thank all principal investigators and researchers for ICU data collection and for sharing their valuable expertise (collaboration group, supplementary material 11). We would like to thank the InTBIR funders and investigators for the collaboration and support. We would like to thank Daan Nieboer (Erasmus MC, Rotterdam) for his statistical support and Dr. Francesca Graziano for her assistance with Fig. 2. CENTER-TBI investigators and participants: Cecilia Åkerlund, Krisztina Amrein, Nada Andelic, Lasse Andreassen, Gérard Audibert, Philippe Azouvi, Maria Luisa Azzolini, Ronald Bartels, Ronny Beer, Bo-Michael Bellander, Habib Benali, Maurizio Berardino, Luigi Beretta, Erta Beqiri, Morten Blaabjerg, Stine Borgen Lund, Camilla Brorsson, Andras Buki, Manuel Cabeleira, Alessio Caccioppola, Emiliana Calappi, Maria Rosa Calvi, Peter Cameron, Guillermo Carbayo Lozano, Ana M. Castaño-León, Simona Cavallo, Giorgio Chevallard, Arturo Chieregato, Mark Coburn, Jonathan Coles, Jamie D. Cooper, Marta Correia, Endre Czeiter, Marek Czosnyka, Claire Dahyot-Fizelier, Paul Dark, Véronique DeKeyser, Vincent Degos, Francesco Della Corte, Hugo den Boogert, Bart Depreitere, Dula Dilvesi, Abhishek Dixit, Jens Dreier, Guy-Loup Dulière, Erzsébet Ezer, Martin Fabricius, Kelly Foks, Shirin Frisvold, Alex Furmanov, Damien Galanaud, Dashiell Gantner, Alexandre Ghuysen, Lelde Giga, Jagos Golubovic, Pedro A. Gomez, Francesca Grossi, Deepak Gupta, Iain Haitsma, Eirik Helseth, Peter J. Hutchinson, Stefan Jankowski, Faye Johnson, Mladen Karan, AngelosG. Kolias, Daniel Kondziella, Evgenios Koraropoulos, Lars-Owe Koskinen, Noémi Kovács, Ana Kowark, Alfonso Lagares, Steven Laureys, Didier Ledoux, Aurelie Lejeune, Roger Lightfoot, Alex Manara, Costanza Martino, Hugues Maréchal, Julia Mattern, Catherine McMahon, Tomas Menovsky, Benoit Misset, Visakh Muraleedharan, Lynnette Murray, Ancuta Negru, Virginia Newcombe, József Nyirádi, Fabrizio Ortolano, Jean-François Payen, Vincent Perlbarg, Paolo Persona, Anna Piippo-Karjalainen, Horia Ples, Inigo Pomposo, Jussi P. Posti, Louis Puybasset, Andreea Radoi, Arminas Ragauskas, Rahul Raj, Jonathan Rhodes, Sophie Richter, Saulius Rocka, Cecilie Roe, Olav Roise, Jeffrey V. Rosenfeld, Christina Rosenlund, Guy Rosenthal, Rolf Rossaint, Sandra Rossi, Juan Sahuquillo, Oddrun Sandrød, Oliver Sakowitz, Renan Sanchez-Porras, Kari Schirmer-Mikalsen, Rico Frederik Schou, Peter Smielewski, Abayomi Sorinola, Emmanuel Stamatakis, Nina Sundström, Riikka Takala, Viktória Tamás, Tomas Tamosuitis, Olli Tenovuo, Matt Thomas, Dick Tibboel, Christos Tolias, Tony Trapani, CristinaMaria Tudora, Peter Vajkoczy, Shirley Vallance, Egils Valeinis , Zoltán Vámos, Gregory Van der Steen Roel P. J. van Wijk, Alessia Vargiolu, Emmanuel Vega, Anne Vik, Rimantas Vilcinis, Victor Volovici, Petar Vulekovic, Guy Williams, Stefan Winzeck, Stefan Wolf, Alexander Younsi, Frederick A. Zeiler, Agate Ziverte Hans Clusmann, Daphne Voormolen, Jeroen T. J. M. van Dijck, Thomas A. van Essen.
Abbreviations
- AIS
Abbreviated injury scale
- CENTER-TBI
Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury
- CPP
Cerebral perfusion pressure
- CT
Computer tomography
- EDH
Epidural hematoma
- GCS
Glasgow Coma Scale
- GOSE
Glasgow Outcome Scale Extended
- ICP
Intracranial pressure
- ICU
Intensive care unit
- IMPACT
International Mission for Prognosis and Analysis of Clinical Trials
- MOR
Median odds ratio
- tSAH
Traumatic subarachnoid hemorrhage
- TBI
Traumatic brain injury
- US
United States
Author contributions
JAH and EJAW analyzed the data and drafted the tables and figures. JAH, EJAW, and NS interpreted the data and drafted the manuscript. NS designed the study protocol and supervised the study. HFL, GC, AIRM, and DKM were involved in regular meetings on the manuscript and reviewed the manuscript multiple times. All authors were involved in the design of the CENTER-TBI study, and reviewed and approved the final version of the manuscript.
Funding
This research is funded by the European Commission 7th Framework program (602150). Additional funding was obtained from the Hannelore Kohl Stiftung (Germany), from OneMind (USA), from Integra LifeSciences Corporation (USA) and from Neurotrauma Sciences (USA). The funders had no role in the design of the study and collection, analysis, interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available via https://www.center-tbi.eu/data on reasonable request.
Compliance with ethical standards
Conflicts of interest
AIRM declares consulting fees from PresSura Neuro, Integra Life Sciences, and NeuroTrauma Sciences. DKM reports grants from the UK National Institute for Health Research, during the conduct of the study; grants, personal fees, and non-financial support from GlaxoSmithKline; personal fees from Neurotrauma Sciences, Lantmaanen AB, Pressura, and Pfizer, outside of the submitted work. WP reports grants from the Netherlands Brain Foundation. ES reports personal fees from Springer, during the conduct of the study. All other authors declare no competing interests.
Ethics approval and consent to participate
In each recruiting site, ethical approval was given; an overview is available online [28].
Footnotes
The CENTER-TBI investigators are listed in the acknowledgements section.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jilske A. Huijben and Eveline J. A. Wiegers contributed equally.
Contributor Information
Jilske A. Huijben, Email: j.a.huijben@erasmusmc.nl
CENTER-TBI investigators and participants:
Cecilia Åkerlund, Krisztina Amrein, Nada Andelic, Lasse Andreassen, Gérard Audibert, Philippe Azouvi, Maria Luisa Azzolini, Ronald Bartels, Ronny Beer, Bo-Michael Bellander, Habib Benali, Maurizio Berardino, Luigi Beretta, Erta Beqiri, Morten Blaabjerg, Stine Borgen Lund, Camilla Brorsson, Andras Buki, Manuel Cabeleira, Alessio Caccioppola, Emiliana Calappi, Maria Rosa Calvi, Peter Cameron, Guillermo Carbayo Lozano, Ana M. Castaño-León, Simona Cavallo, Giorgio Chevallard, Arturo Chieregato, Mark Coburn, Jonathan Coles, Jamie D. Cooper, Marta Correia, Endre Czeiter, Marek Czosnyka, Claire Dahyot-Fizelier, Paul Dark, Véronique DeKeyser, Vincent Degos, Francesco Della Corte, Hugo den Boogert, Bart Depreitere, Dula Dilvesi, Abhishek Dixit, Jens Dreier, Guy-Loup Dulière, Erzsébet Ezer, Martin Fabricius, Kelly Foks, Shirin Frisvold, Alex Furmanov, Damien Galanaud, Dashiell Gantner, Alexandre Ghuysen, Lelde Giga, Jagos Golubovic, Pedro A. Gomez, Francesca Grossi, Deepak Gupta, Iain Haitsma, Eirik Helseth, Peter J. Hutchinson, Stefan Jankowski, Faye Johnson, Mladen Karan, AngelosG. Kolias, Daniel Kondziella, Evgenios Koraropoulos, Lars-Owe Koskinen, Noémi Kovács, Ana Kowark, Alfonso Lagares, Steven Laureys, Didier Ledoux, Aurelie Lejeune, Roger Lightfoot, Alex Manara, Costanza Martino, Hugues Maréchal, Julia Mattern, Catherine McMahon, Tomas Menovsky, Benoit Misset, Visakh Muraleedharan, Lynnette Murray, Ancuta Negru, Virginia Newcombe, József Nyirádi, Fabrizio Ortolano, Jean-François Payen, Vincent Perlbarg, Paolo Persona, Anna Piippo-Karjalainen, Horia Ples, Inigo Pomposo, Jussi P. Posti, Louis Puybasset, Andreea Radoi, Arminas Ragauskas, Rahul Raj, Jonathan Rhodes, Sophie Richter, Saulius Rocka, Cecilie Roe, Olav Roise, Jeffrey V. Rosenfeld, Christina Rosenlund, Guy Rosenthal, Rolf Rossaint, Sandra Rossi, Juan Sahuquillo, Oddrun Sandrød, Oliver Sakowitz, Renan Sanchez-Porras, Kari Schirmer-Mikalsen, Rico Frederik Schou, Peter Smielewski, Abayomi Sorinola, Emmanuel Stamatakis, Nina Sundström, Riikka Takala, Viktória Tamás, Tomas Tamosuitis, Olli Tenovuo, Matt Thomas, Dick Tibboel, Christos Tolias, Tony Trapani, CristinaMaria Tudora, Peter Vajkoczy, Shirley Vallance, Egils Valeinis, Zoltán Vámos, Gregory Van der Steen, Roel P. J. van Wijk, Alessia Vargiolu, Emmanuel Vega, Anne Vik, Rimantas Vilcinis, Victor Volovici, Petar Vulekovic, Guy Williams, Stefan Winzeck, Stefan Wolf, Alexander Younsi, Frederick A. Zeiler, Agate Ziverte Hans Clusmann, Daphne Voormolen, Jeroen T. J. M. van Dijck, and Thomas A. van Essen
References
- 1.Majdan M, Plancikova D, Brazinova A, Rusnak M, Nieboer D, Feigin V, Maas A. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health. 2016;1:e76–e83. doi: 10.1016/S2468-2667(16)30017-2. [DOI] [PubMed] [Google Scholar]
- 2.Stocchetti N, Carbonara M, Citerio G, Ercole A, Skrifvars MB, Smielewski P, Zoerle T, Menon DK. Severe traumatic brain injury: targeted management in the intensive care unit. Lancet Neurol. 2017;16:452–464. doi: 10.1016/S1474-4422(17)30118-7. [DOI] [PubMed] [Google Scholar]
- 3.Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, Napolitano LM, O’Grady NP, Bartlett JG, Carratala J, El Solh AA, Ewig S, Fey PD, File TM, Jr, Restrepo MI, Roberts JA, Waterer GW, Cruse P, Knight SL, Brozek JL. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63:e61–e111. doi: 10.1093/cid/ciw353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steyerberg EW, Wiegers E, Sewalt C, Buki A, Citerio G, De Keyser V, Ercole A, Kunzmann K, Lanyon L, Lecky F, Lingsma H, Manley G, Nelson D, Peul W, Stocchetti N, von Steinbuchel N, Vande Vyvere T, Verheyden J, Wilson L, Maas AIR, Menon DK, Participants C-T, Investigators Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: a European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 2019;18:923–934. doi: 10.1016/S1474-4422(19)30232-7. [DOI] [PubMed] [Google Scholar]
- 5.Volovici V, Ercole A, Citerio G, Stocchetti N, Haitsma IK, Huijben JA, Dirven CMF, van der Jagt M, Steyerberg EW, Nelson D, Cnossen MC, Maas AIR, Polinder S, Menon DK, Lingsma HF. Intensive care admission criteria for traumatic brain injury patients across Europe. J Crit Care. 2019;49:158–161. doi: 10.1016/j.jcrc.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Maas AI, Menon DK, Steyerberg EW, Citerio G, Lecky F, Manley GT, Hill S, Legrand V, Sorgner A, Participants C-T, Investigators Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI): a prospective longitudinal observational study. Neurosurgery. 2015;76:67–80. doi: 10.1227/NEU.0000000000000575. [DOI] [PubMed] [Google Scholar]
- 7.Zuercher P, Groen JL, Aries MJ, Steyerberg EW, Maas AI, Ercole A, Menon DK. Reliability and validity of the therapy intensity level scale: analysis of clinimetric properties of a novel approach to assess management of intracranial pressure in traumatic brain injury. J Neurotrauma. 2016;33:1768–1774. doi: 10.1089/neu.2015.4266. [DOI] [PubMed] [Google Scholar]
- 8.Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, Rastam L, Larsen K. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60:290–297. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS, Murray GD, Marmarou A, Roberts I, Habbema JD, Maas AI. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5:e165. doi: 10.1371/journal.pmed.0050165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Stram DO, Lee JW. Variance components testing in the longitudinal mixed effects model. Biometrics. 1994;50:1171–1177. doi: 10.2307/2533455. [DOI] [PubMed] [Google Scholar]
- 12.Schrijvers LH, Beijlevelt-van der Zande M, Peters M, Lock J, Cnossen MH, Schuurmans MJ, Fischer K. Adherence to prophylaxis and bleeding outcome in haemophilia: a multicentre study. Br J Haematol. 2016;174:454–460. doi: 10.1111/bjh.14072. [DOI] [PubMed] [Google Scholar]
- 13.Van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–68. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- 14.Marshall LF, Becker DP, Bowers SA, Cayard C, Eisenberg H, Gross CR, Grossman RG, Jane JA, Kunitz SC, Rimel R, Tabaddor K, Warren J. The National Traumatic Coma Data Bank. Part 1: design, purpose, goals, and results. J Neurosurg. 1983;59:276–284. doi: 10.3171/jns.1983.59.2.0276. [DOI] [PubMed] [Google Scholar]
- 15.Maas AIR, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, Bragge P, Brazinova A, Buki A, Chesnut RM, Citerio G, Coburn M, Cooper DJ, Crowder AT, Czeiter E, Czosnyka M, Diaz-Arrastia R, Dreier JP, Duhaime AC, Ercole A, van Essen TA, Feigin VL, Gao G, Giacino J, Gonzalez-Lara LE, Gruen RL, Gupta D, Hartings JA, Hill S, Jiang JY, Ketharanathan N, Kompanje EJO, Lanyon L, Laureys S, Lecky F, Levin H, Lingsma HF, Maegele M, Majdan M, Manley G, Marsteller J, Mascia L, McFadyen C, Mondello S, Newcombe V, Palotie A, Parizel PM, Peul W, Piercy J, Polinder S, Puybasset L, Rasmussen TE, Rossaint R, Smielewski P, Soderberg J, Stanworth SJ, Stein MB, von Steinbuchel N, Stewart W, Steyerberg EW, Stocchetti N, Synnot A, Te Ao B, Tenovuo O, Theadom A, Tibboel D, Videtta W, Wang KKW, Williams WH, Wilson L, Yaffe K, In TP, Investigators Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16:987–1048. doi: 10.1016/S1474-4422(17)30371-X. [DOI] [PubMed] [Google Scholar]
- 16.Nelson LD, Temkin NR, Dikmen S, Barber J, Giacino JT, Yuh E, Levin HS, McCrea MA, Stein MB, Mukherjee P, Okonkwo DO, Diaz-Arrastia R, Manley GT, TRACK-TBI Investigators. Adeoye O, Badjatia N, Boase K, Bodien Y, Bullock MR, Chesnut R, Corrigan JD, Crawford K, Mis Duhaime AC, Ellenbogen R, Feeser VR, Ferguson A, Foreman B, Gardner R, Gaudette E, Gonzalez L, Gopinath S, Gullapalli R, Hemphill JC, Hotz G, Jain S, Korley F, Kramer J, Kreitzer N, Lindsell C, Machamer J, Madden C, Martin A, McAllister T, Merchant R, Noel F, Palacios E, Perl D, Puccio A, Rabinowitz M, Robertson CS, Rosand J, Sander A, Satris G, Schnyer D, Seabury S, Sherer M, Taylor S, Toga A, Valadka A, Vassar MJ, Vespa P, Wang K, Yue JK, Zafonte R. Recovery after mild traumatic brain injury in patients presenting to us level i trauma centers: a transforming research and clinical knowledge in traumatic brain injury (TRACK-TBI) study. JAMA Neurol. 2019 doi: 10.1001/jamaneurol.2019.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marincowitz C, Lecky FE, Townend W, Borakati A, Fabbri A, Sheldon TA. The risk of deterioration in GCS13-15 patients with traumatic brain injury identified by computed tomography imaging: a systematic review and meta-analysis. J Neurotrauma. 2018;35:703–718. doi: 10.1089/neu.2017.5259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bonow RH, Quistberg A, Rivara FP, Vavilala MS. Intensive care unit admission patterns for mild traumatic brain injury in the USA. Neurocrit Care. 2019;30:157–170. doi: 10.1007/s12028-018-0590-0. [DOI] [PubMed] [Google Scholar]
- 19.Cnossen MC, Polinder S, Andriessen TM, van der Naalt J, Haitsma I, Horn J, Franschman G, Vos PE, Steyerberg EW, Lingsma H. Causes and consequences of treatment variation in moderate and severe traumatic brain injury: a multicenter study. Crit Care Med. 2017;45:660–669. doi: 10.1097/CCM.0000000000002263. [DOI] [PubMed] [Google Scholar]
- 20.Bulger EM, Nathens AB, Rivara FP, Moore M, MacKenzie EJ, Jurkovich GJ, Brain Trauma F. Management of severe head injury: institutional variations in care and effect on outcome. Crit Care Med. 2002;30:1870–1876. doi: 10.1097/00003246-200208000-00033. [DOI] [PubMed] [Google Scholar]
- 21.Alali AS, Fowler RA, Mainprize TG, Scales DC, Kiss A, de Mestral C, Ray JG, Nathens AB. Intracranial pressure monitoring in severe traumatic brain injury: results from the American College of Surgeons Trauma Quality Improvement Program. J Neurotrauma. 2013;30:1737–1746. doi: 10.1089/neu.2012.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stocchetti N, Penny KI, Dearden M, Braakman R, Cohadon F, Iannotti F, Lapierre F, Karimi A, Maas A, Jr, Murray GD, Ohman J, Persson L, Servadei F, Teasdale GM, Trojanowski T, Unterberg A, European Brain Injury C Intensive care management of head-injured patients in Europe: a survey from the European brain injury consortium. Intensive Care Med. 2001;27:400–406. doi: 10.1007/s001340000825. [DOI] [PubMed] [Google Scholar]
- 23.Cnossen MC, Huijben JA, van der Jagt M, Volovici V, van Essen T, Polinder S, Nelson D, Ercole A, Stocchetti N, Citerio G, Peul WC, Maas AIR, Menon D, Steyerberg EW, Lingsma HF, Investigators C-T Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: a survey in 66 neurotrauma centers participating in the CENTER-TBI study. Crit Care. 2017;21:233. doi: 10.1186/s13054-017-1816-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huijben JA, van der Jagt M, Cnossen MC, Kruip M, Haitsma IK, Stocchetti N, Maas AIR, Menon DK, Ercole A, Maegele M, Stanworth SJ, Citerio G, Polinder S, Steyerberg EW, Lingsma HF. Variation in blood transfusion and coagulation management in traumatic brain injury at the intensive care unit: a survey in 66 neurotrauma centers participating in the collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury Study. J Neurotrauma. 2017 doi: 10.1089/neu.2017.5194. [DOI] [PubMed] [Google Scholar]
- 25.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Variation in adult traumatic brain injury outcomes in the United States. J Head Trauma Rehabil. 2018;33:E1–E8. doi: 10.1097/HTR.0000000000000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lingsma HF, Roozenbeek B, Li B, Lu J, Weir J, Butcher I, Marmarou A, Murray GD, Maas AI, Steyerberg EW. Large between-center differences in outcome after moderate and severe traumatic brain injury in the international mission on prognosis and clinical trial design in traumatic brain injury (IMPACT) study. Neurosurgery. 2011;68:601–607. doi: 10.1227/NEU.0b013e318209333b. [DOI] [PubMed] [Google Scholar]
- 27.Maas AI, Menon DK, Lingsma HF, Pineda JA, Sandel ME, Manley GT. Re-orientation of clinical research in traumatic brain injury: report of an international workshop on comparative effectiveness research. J Neurotrauma. 2012;29:32–46. doi: 10.1089/neu.2010.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kelly D, Mc Erlean S, Byrne D, Mahon PM, Mc Caffrey J. A case of thoracic giant cell tumor of bone and discussion of radiological features and current management practices. Radiol Case Rep. 2016;11:222–226. doi: 10.1016/j.radcr.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1 (JPEG 21 kb) Figure S1: Length of ICU stay. A Length of Stay at the ICU for all patients (n = 2138). B Length of Stay at the ICU for the first 7 days, stratified by ICU mortality (data available for 1130 patients)
Supplementary material 3 (JPEG 51 kb) Figure S2: Cause of Mortality in Early Death Group. This figure shows the cause of mortality in the early death patients (N = 96) Only one reason per patient could be entered by clinicians
Supplementary material 4 (JPEG 27 kb) Figure S3: Reason for ICU admission for short-stay patients. This figure shows the reasons for ICU admission for the short-stay patients (N = 631). Only one reason per patients could be entered by clinicians
Data Availability Statement
The datasets used and/or analyzed during the current study are available via https://www.center-tbi.eu/data on reasonable request.