Abstract
Social determinants of health (SDoH) are the conditions in which people live and work that shape access to essential social and economic resources. Calls for healthcare systems to intervene on unmet social needs have stimulated several large-scale initiatives across the country. Yet, such activities are underway in the absence of a unifying conceptual framework outlining the potential mechanisms by which healthcare-based unmet social need interventions can improve health outcomes. Drawing on theoretical foundations and empirical evidence about the relationship between unmet social needs and health, the authors developed the OASIS (Outcomes from Addressing SDoH in Systems) conceptual framework to map the known and hypothesized pathways by which unmet social need screening and referral interventions may impact outcomes. The OASIS framework may help guide policy makers, healthcare system leaders, clinicians, and researchers to utilize a more unified approach in their efforts to implement and evaluate unmet social need interventions and thus foster the development of an evidence base to inform healthcare systems to more effectively mitigate the consequences of unmet social needs. Adopting an overarching conceptual framework for addressing unmet social needs by healthcare systems holds promise for better achieving health equity and promoting health at the individual and population levels.
KEY WORDS: social determinants of health, health equity, conceptual framework, healthcare delivery
SOCIAL DETERMINANTS EXERT SUBSTANTIAL EFFECTS ON ADULT HEALTH
Reflecting the Society of General Medicine’s (SGIM) vision to foster a “just system of care …where all people can achieve optimal health” and its value of “attending to population health outcomes and their social determinants,” social determinants of health (SDoH) was a prominent topic at the 2019 SGIM annual meeting. SDoH are the conditions in which people are born, live, and work,1 and exert sizable effects on the onset and progression of disease.2, 3 Unmet social needs (e.g., food insecurity) resulting from adverse social conditions are associated with decrements in health.3–5 This, combined with the rise of value-based purchasing and accountable care organizations (ACOs), which require healthcare providers to improve patient outcomes at lower costs (holding providers accountable for health outcomes affected by unmet social needs), has motivated healthcare delivery systems to move beyond the traditional biomedical model of illness to one that additionally identifies and addresses patients’ unmet social needs. Numerous professional organizations including the National Academy of Medicine, the American College of Physicians, and the American Heart Association now emphasize and support the need for healthcare systems to screen for unmet social needs at healthcare visits.5–7 While healthcare systems cannot address the broader social conditions in which their patients live (e.g., low wages), identifying and addressing patients’ immediate unmet social needs as part of the clinical encounter may improve individual and population health and reduce healthcare costs.8
A CONCEPTUAL FRAMEWORK IS NEEDED TO EVALUATE AND ASSESS THE IMPACT OF SDoH INTERVENTIONS IN HEALTHCARE SYSTEMS
Recent large-scale initiatives have begun to intervene on unmet social needs. These include the Centers for Medicare and Medicaid’s Accountable Health Communities demonstration to test whether identifying and addressing unmet social needs impacts healthcare costs among community-dwelling Medicare/Medicaid beneficiaries, and the National Association of Community Health Centers’ implementation of the Protocol for Responding to and Assessing Patient Asset, Risks and Experiences (PRAPARE), a social needs screening tool for health center patients. Medicaid managed care organizations and most state Medicaid ACOs are also encouraging or requiring screening and referral (“S&R”) for unmet social needs. Yet these and other smaller-scale initiatives that address unmet social needs are underway in the absence of a unifying conceptual framework outlining the potential mechanisms by which healthcare-based interventions to address unmet social needs can improve health outcomes. For example, recent findings demonstrated that unmet social need S&R was associated with reduced blood pressure and lipids, but the mechanisms by which the intervention led to such effects were not elucidated.9 Similar studies reporting positive health effects from interventions addressing housing and income needs also failed to describe the pathways by which these interventions led to positive outcomes.10, 11 Thus, it is unclear what elements of an SDoH intervention led to the effect and why; in turn, it is not known what needs to change or be replicated. To that end, a framework would help inform and guide future efforts to implement and evaluate interventions to identify and address unmet social needs, and to evaluate the outcomes of such efforts.12
EXISTING FRAMEWORKS DO NOT ADEQUATELY DETAIL THE PATHWAYS BY WHICH HEALTHCARE-BASED SDoH INTERVENTIONS MAY IMPROVE HEALTH
Existing conceptual models about SDoH are not sufficiently granular about the pathway by which healthcare-based interventions that address unmet social needs can improve health outcomes. For example, WHO’s SDoH conceptual framework includes “Health System” as a mediating force between unmet social needs and health but does not detail the underlying mechanisms.1 DeVoe’s (2016) framework proposes the collection of community “vital signs” and patient-reported SDoH, making such data available at the point of care for panel management and referrals to needed social services, with the end goal of improving health outcomes.13 Yet, there is no clear hypothesized pathway depicting how collecting and using such data in these ways might improve health outcomes. Steiner et al.’s (2019) care continuum framework adds some important detail, suggesting that connecting patients to community resources to address unmet social needs is the intermediate step to improved health outcomes, but the “black box” between addressing these unmet needs and the effect on outcomes needs further elucidation.14 We suggest that a framework that simply and clearly explicates these pathways can help to guide intervention efforts and measurement, improve understanding about how outcomes are or are not affected, and isolate which levers drive outcomes.
FILLING THE GAP: THE OASIS FRAMEWORK
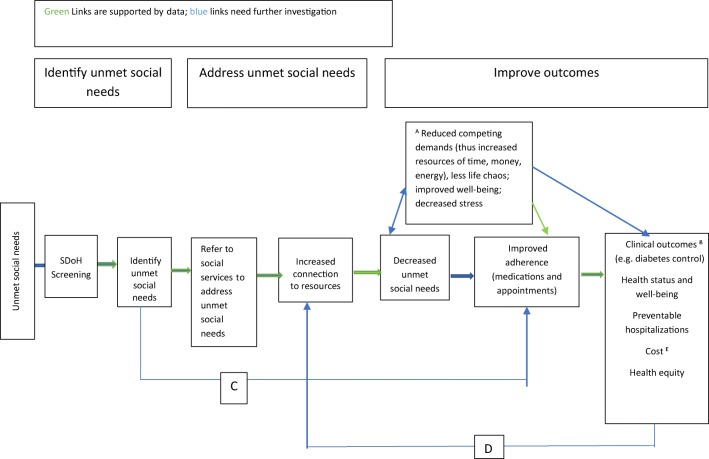
We developed the OASIS (Outcomes from Addressing SDoH in Systems) framework to map the known and hypothesized pathways by which S&R interventions in healthcare settings may impact outcomes (Fig. 1). This framework is based on Maslow’s Hierarchy of Needs model15 which specifies that one’s basic physiological needs (e.g., shelter, food) must be met before one can address higher order needs. For example, someone who is food insecure will likely be more focused on the immediate need to obtain food than on adhering to medications or attending medical appointments.
Figure 1.
OASIS framework: Outcomes from Addressing SDoH in Systems. Green links are supported by data; blue links need further investigation. Letter “A” indicates that for patients with multiple unmet social needs, resolution of one need may enable them to address another. Reduced competing demands includes freeing up various resources (money, time, energy) to address other needs, which in turn can affect health outcomes. Letter “B” indicates clinical outcomes which may include but are not limited to conditions where adherence to therapy directly impacts outcomes, such as hypertension, diabetes, and asthma. Letter “C” indicates that identification of unmet social needs may be beneficial, even without referring to resources. For patients with transportation problems, for example, delivering prescriptions through mail order can bypass the barrier posed by the unmet transportation need without directly addressing it. Letter “D” indicates that improved outcomes, such as improved well-being, may help patients connect to resources. Letter “E” indicates costs may be reduced through improved control of chronic conditions, such as hypertension, which could avert costly future admissions for stroke or target organ damage. But increased costs to address unmet social needs may affect the equation for other conditions.
The first three components in our model rest on prior research supporting the notion that screening for unmet social needs in clinical settings is feasible, leads to identification of unmet social needs and, when coupled with subsequent referrals to services, fosters connections to services to address such needs.16–20 Studies in primary care have found that implementing unmet social need screening using existing electronic health record work flows is feasible and successful in identifying such needs.21 Studies also demonstrate that healthcare-based S&R interventions identify a range of unmet social needs including difficulty affording healthcare, food, and utilities19 and lead to receipt of more community services.16, 18
Our model’s fourth component–that connection to social services and community resources will result in unmet social needs reduction–is supported by a recent systematic review of interventions on patients’ social and economic needs which concluded that programs that connect program participants to resources to address unmet social needs generally have positive impacts on those needs.22 For example, such interventions reduced the risk of homelessness,23 increased safety-promoting behaviors among women experiencing intimate partner violence,24 and increased employment.16, 25
Next, we posit that reductions in unmet social needs will lead to greater adherence to medications or medical appointments, based on research indicating that competing demands, life chaos, and well-being affect adherence to recommended care.26 In turn, adherence leads to improved clinical outcomes such as reduced blood pressure and blood sugar and improved asthma control,27 which we posit will reduce urgent care usage and preventable hospitalizations. Additionally, the cumulative pathways model postulates that chronic stress, defined as prolonged exposure to adversity such as unmet social needs, can result in undue wear and tear on the body’s physiological stress-response systems (i.e., allostatic load), leading to worse health outcomes. Animal and human studies have demonstrated the impact this stress can have on hypothalamic-pituitary-adrenal hyperactivity.28–33 Thus, by reducing stress, physiological and epigenetic beneficial changes may accrue and reduce allostatic load and promote the upregulation of health-promoting and disease prevention genes. Finally, the OASIS model posits that improved patient-level health outcomes will be associated with decreased costs (due to decreased acute care and avoidable utilization) and increased health equity (as many unmet social needs underlie other bases of disparities such as race and ethnicity34).
Importantly, the OASIS model also captures some of the complexity of the relationship between unmet social needs and outcomes, including the bi-directionality of unmet social needs and health outcomes. For example, unmet social needs may exacerbate a patient’s depression or anxiety, which may not only affect adherence and health outcomes but can impede the patient from connecting with resources to address their unmet social needs. As well, identifying patients’ unmet social needs can affect health outcomes even if the needs are not addressed. For instance, if a provider knows a patient has limited transportation resources, s/he can convert prescriptions to mail order vs. pharmacy pick-up. This tailoring of care plans, also known as “social risk-informed care” may help reduce barriers to adherence35, 36 and, in turn, improve clinical outcomes. Finally, addressing one unmet social need may free-up resources to address other needs. For instance, recent research showed a spillover “income effect” as receipt of SNAP benefits allowed beneficiaries to buy medications, conceivably by reducing out-of-pocket food expenditures.37
APPLYING THE OASIS FRAMEWORK
We envision several uses for the OASIS framework; initially, it can be used to determine the relevance of and need for a given research study related to S&R. In this capacity, the framework can be used to map and organize the existing evidence base and in so doing identify areas where knowledge gaps exist. Related and importantly, use of the OASIS framework to amass and organize the evidence base can also help to build (and refine) understanding of the pathways by which clinical settings can effectively intervene on unmet social needs.
In addition, for researchers and healthcare leaders considering implementation and evaluation of S&R interventions, the framework can be used to anchor the proposed S&R intervention along the pathway and set realistic goals for defining program success. The nature and duration of the intervention will likely be key factors. For instance, a 1-year S&R intervention may not exert meaningful impact on clinical health outcomes but might lead to increased connection to resources that address participants’ unmet social needs and improve well-being. Situating an intervention within the framework provides guidance on the process outcomes that could be measured and tracked to help explain why the intervention did or did not achieve the expected outcomes. Tracking and documenting intermediate process outcomes is critical for healthcare and operational leaders wanting to build the case for their programs and for researchers wanting to establish causal linkages between observed outcomes and the intervention under study.
The OASIS framework also helps to organize data sources for measurement of the outcomes it describes; for example, the process measures suggested by the framework may be derived from existing data. For instance, electronic health record (EHR) platforms including EPIC are increasingly incorporating unmet social need screening domains, data from which can identify who gets screened and document the unmet social needs that are identified.38 Indicators of utilization (preventable hospitalizations, urgent care use) and adherence (prescription refills, appointment keeping) can be derived from administrative claims data. However, in two instances—patient connection to resources and unmet social need reduction—EHR and/or administrative data will be insufficient. For example, healthcare interventions that address patients’ unmet social needs often involve referrals to community-based programs (e.g., housing programs, food pantries) that operate outside the healthcare system itself, which can inhibit tracking whether a patient followed through with a referral and connected to a service. In these instances, information would need to be collected through either direct follow-up with patients or the organizations to which they are referred, as would assessments of whether unmet social needs are reduced through these service connections. There are numerous examples from the literature of programs successfully gathering this information.22
CONCLUSION
As healthcare systems take on the charge of identifying and addressing patients’ unmet social needs, there is an opportunity to make inroads on population health and health equity. Given the nascence of this research field and the need for further understanding about the pathways by which unmet social need interventions will affect health outcomes, some healthcare systems are reluctant to proceed without additional evidence-based guidance on the outcomes of such efforts. We developed OASIS to help those engaged in social needs interventional work to think more systematically about how to design these interventions and assess their effects, while acknowledging that it does not fully detail the immensely complex relationship between diverse unmet social needs and outcomes; others have done this extensively.5 Our hope is that the relative simplicity of the OASIS framework will encourage its use by policy makers, healthcare leaders, clinicians, and researchers and foster a unified approach in efforts to implement and evaluate healthcare-based unmet social needs interventions. In this way, the framework can advance the development of an evidence base that will inform healthcare systems to more effectively mitigate the consequences of unmet social needs.
Funding Information
Dr. Kressin was financially supported in part by a Senior VA HSR&D Research Career Scientist award (RCS 02-066.1).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. What are social determinants of health?. 2019 [cited 2019 March 12]; Available from: http://who.int/social_determinants/sdh_definition/en/.
- 2.Marmot M. Social justice, epidemiology and health inequalities. Eur J Epidemiol. 2017;32(7):537–546. doi: 10.1007/s10654-017-0286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilensky G. Addressing Social Issues Affecting Health to Improve US Health Outcomes. Jama. 2016;315(15):1552–3. doi: 10.1001/jama.2016.3863. [DOI] [PubMed] [Google Scholar]
- 4.Knighton AJ, Stephenson B, Savitz LA. Measuring the Effect of Social Determinants on Patient Outcomes: A Systematic Literature Review. J Health Care Poor Underserved. 2018;29(1):81–106. doi: 10.1353/hpu.2018.0009. [DOI] [PubMed] [Google Scholar]
- 5.Havranek EP, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873–98. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 6.Daniel H, Bornstein SS, Kane GC. Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. Ann Intern Med. 2018;168(8):577–578. doi: 10.7326/M17-2441. [DOI] [PubMed] [Google Scholar]
- 7.Dzau VJ, et al. Vital Directions for Health and Health Care: Priorities From a National Academy of Medicine InitiativeNAM’s Vital Directions for Health and Health Care InitiativeNAM’s Vital Directions for Health and Health Care Initiative. JAMA. 2017;317(14):1461–1470. doi: 10.1001/jama.2017.1964. [DOI] [PubMed] [Google Scholar]
- 8.“Meeting Individual Social Needs Falls Short Of Addressing Social Determinats Of Health”, in Health Affairs Blog. 2019.
- 9.Berkowitz SA, et al. Addressing Unmet Basic Resource Needs as Part of Chronic Cardiometabolic Disease Management. JAMA Intern Med. 2017;177(2):244–252. doi: 10.1001/jamainternmed.2016.7691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herd P, Schoeni RF, House JS. Upstream solutions: does the supplemental security income program reduce disability in the elderly? Milbank Q. 2008;86(1):5–45. doi: 10.1111/j.1468-0009.2007.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ludwig J, et al. Neighborhoods, obesity, and diabetes--a randomized social experiment. N Engl J Med. 2011;365(16):1509–19. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ravitch S, Riggan M. Reason & Rigor How Conceptual Frameworks Guide Research. 2. Thousand Oaks, CA: SAGE Publications, Inc; 2016. [Google Scholar]
- 13.DeVoe JE, et al. Perspectives in Primary Care: A Conceptual Framework and Path for Integrating Social Determinants of Health Into Primary Care Practice. Ann Fam Med. 2016;14(2):104–8. doi: 10.1370/afm.1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steiner J, et al. Interventions to address basic resource needs in Kaiser Permanente: A care continuum and an outcomes wheel. Perm J. 2018;22:18–130. [Google Scholar]
- 15.Maslow AH. A theory of human motivation. Psychol Rev. 1943;50(4):370–96. doi: 10.1037/h0054346. [DOI] [Google Scholar]
- 16.Garg A, et al. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–304. doi: 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gordon JA, Emond JA, Camargo CA., Jr The State Children’s Health Insurance Program: a multicenter trial of outreach through the emergency department. Am J Public Health. 2005;95(2):250–3. doi: 10.2105/AJPH.2003.037242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen AL, et al. A clinic-based pilot intervention to enhance diabetes management for elderly Hispanic patients. J Health Environ Educ. 2016;8:1–6. doi: 10.18455/08001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkowitz SA, et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf. 2016;25(3):164–72. doi: 10.1136/bmjqs-2015-004521. [DOI] [PubMed] [Google Scholar]
- 20.Andermann A. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev. 2018;39:19. doi: 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buitron de la Vega P, et al. Implementing an EHR-based Screening and Referral System to Address Social Determinants of Health in Primary Care. Med Care. 2019;57(Suppl 6 Suppl 2):S133–s139. doi: 10.1097/MLR.0000000000001029. [DOI] [PubMed] [Google Scholar]
- 22.Gottlieb LM, Wing H, Adler NE. A Systematic Review of Interventions on Patients’ Social and Economic Needs. Am J Prev Med. 2017;53(5):719–729. doi: 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Herman DB, et al. Randomized trial of critical time intervention to prevent homelessness after hospital discharge. Psychiatr Serv. 2011;62(7):713–9. doi: 10.1176/ps.62.7.pss6207_0713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillum TL, Sun CJ, Woods AB. Can a health clinic-based intervention increase safety in abused women? Results from a pilot study. J Women's Health (Larchmt) 2009;18(8):1259–64. doi: 10.1089/jwh.2008.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamilton AB, et al. Implementation of Evidence-Based Employment Services in Specialty Mental Health. Health Serv Res. 2013;48(6pt2):2224–2244. doi: 10.1111/1475-6773.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zullig LL, et al. Association between perceived life chaos and medication adherence in a postmyocardial infarction population. Circ Cardiovasc Qual Outcomes. 2013;6(6):619–25. doi: 10.1161/CIRCOUTCOMES.113.000435. [DOI] [PubMed] [Google Scholar]
- 27.Rose AJ, et al. Effects of daily adherence to antihypertensive medication on blood pressure control. J Clin Hypertens (Greenwich) 2011;13(6):416–21. doi: 10.1111/j.1751-7176.2011.00427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci. 2007;18(11):953–7. doi: 10.1111/j.1467-9280.2007.02008.x. [DOI] [PubMed] [Google Scholar]
- 29.Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q. 2002;80(3):433–79. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McEwen BS. Protective and damaging effects of stress mediators: central role of the brain. Dialogues Clin Neurosci. 2006;8(4):367–81. doi: 10.31887/DCNS.2006.8.4/bmcewen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sapolsky RM. Social subordinance as a marker of hypercortisolism. Some unexpected subtleties. Ann N Y Acad Sci. 1995;771:626–39. doi: 10.1111/j.1749-6632.1995.tb44715.x. [DOI] [PubMed] [Google Scholar]
- 32.Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 33.Tsigos C, Chrousos GP. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J Psychosom Res. 2002;53(4):865–71. doi: 10.1016/S0022-3999(02)00429-4. [DOI] [PubMed] [Google Scholar]
- 34.Adler N, et al. Addressing Social Determinats of Health and Health Disparities: A Vital Direction for Health and Health Care, N.A.o.M. NAM Perspectives. Discussion Paper, Washinton, DC, Editor. 2016.
- 35.Gottlieb L, et al. Social Determinants of Health: What’s a Healthcare System to Do? J Healthc Manag. 2019;64(4):243–257. doi: 10.1097/JHM-D-18-00160. [DOI] [PubMed] [Google Scholar]
- 36.Kressin NR, Chapman SE, Magnani JW. A Tale of Two Patients: Patient-Centered Approaches to Adherence as a Gateway to Reducing Disparities. Circulation. 2016;133(24):2583–92. doi: 10.1161/CIRCULATIONAHA.116.015361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Srinivasan M, Pooler JA. Cost-Related Medication Nonadherence for Older Adults Participating in SNAP, 2013–2015. Am J Public Health. 2018;108(2):224–230. doi: 10.2105/AJPH.2017.304176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freij M, et al. Incorporating Social Determinants of Health in Electronic Health Records: Qualitative Study of Current Practices Among Top Vendors. JMIR Med Inform. 2019;7(2):e13849. doi: 10.2196/13849. [DOI] [PMC free article] [PubMed] [Google Scholar]