Abstract
This population epidemiology study characterizes trends in polymerase chain reaction (PCR) test positivity for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in Washington State and the Seattle area between March 1 and April 16, 2020, before and after statewide physical distancing guidelines and stay-at-home orders.
The first reported case of coronavirus disease 2019 (COVID-19) in the US occurred on January 20, 2020, in Snohomish County, Washington.1 The University of Washington (UW) Virology Division was among the first US laboratories to test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and since March 1, 2020, has tested samples from more than 73 000 patients. More than 90% of the samples are from the UW health system and outpatient clinics in Washington State.
The positivity rates for SARS-CoV-2 in outpatient settings in Washington State and in emergency departments (EDs) in Seattle were analyzed to identify temporal trends that may reflect the local dynamics of the pandemic and the effect of mitigation strategies such as physical distancing.
Methods
Samples were collected from 17 232 patients at 127 outpatient clinics across 10 counties and from 1932 patients at 3 Seattle EDs. Specimens (>95% were nasopharyngeal swabs) were analyzed by a laboratory-developed reverse transcriptase–polymerase chain reaction test using the E/RdRp primer set from the World Health Organization,2 N1/N2 primer sets from the US Centers for Disease Control and Prevention,3 or tests from Hologic (Panther Fusion), DiaSorin (Simplexa), and Roche (cobas).
The SARS-CoV-2 positivity rate was analyzed by fitting penalized cubic regression splines to binomial testing data, and accounting for variation in the daily testing totals.4 The results were aligned to the sample collection date for the study period (March 1–April 16, 2020). When a patient had multiple results, only the first positive test was included. Limited demographic data were available from the referring facilities. The 95% CIs for the estimated SARS-CoV-2 positivity rates in the demographic subgroups were calculated by the Wilson score method.5
Comparisons between groups were made using a 2-sided χ2 test with a significance level of .05. The statistical analyses were performed using R version 3.6.1 (R Foundation for Statistical Computing), with smoothed models fit using the mgcv package. This study was approved and granted a waiver of consent by the institutional review boards at UW and the Fred Hutchinson Cancer Research Center.
Results
The positivity rates for SARS-CoV-2 were 8.2% in Washington State outpatient clinics, 8.4% in Seattle-area outpatient clinics, and 14.4% in Seattle EDs. The SARS-CoV-2 positivity rates were higher in males than in females (P < .001 for Washington State and Seattle-area outpatients; P = .13 for Seattle ED patients), and higher in Seattle EDs than in Seattle-area outpatient clinics (P < .001) (Table and Figure).
Table. Patient Demographics by Type of Facility.
| SARS-CoV-2 | SARS-CoV-2 positivity rate, % (95% CI) | ||
|---|---|---|---|
| Not detected | No. of positive cases | ||
| Outpatient clinics in Washington Statea | |||
| Total patients | 15 825 | 1407 | 8.2 (7.8-8.6) |
| Sex | |||
| Female | 9896 | 778 | 7.3 (6.8-7.8) |
| Male | 5910 | 627 | 9.6 (8.9-10.3) |
| Unknown | 19 | 2 | 9.5 (2.7-28.9) |
| Age group, y | |||
| 0-19 | 820 | 46 | 5.3 (4.0-7.0) |
| 0-12 | 449 | 15 | 3.2 (2.0-5.3) |
| 13-19 | 371 | 31 | 7.7 (5.5-10.7) |
| 20-39 | 5793 | 456 | 7.3 (6.7-8.0) |
| 40-59 | 5700 | 544 | 8.7 (8.0-9.4) |
| 60-79 | 3170 | 319 | 9.1 (8.2-10.1) |
| 80-115 | 342 | 42 | 10.9 (8.2-14.5) |
| Outpatient clinics in Seattle areab | |||
| Total patients | 9820 | 905 | 8.4 (7.9-9.0) |
| Sex | |||
| Female | 6251 | 513 | 7.6 (7.0-8.2) |
| Male | 3565 | 391 | 9.9 (9.0-10.9) |
| Unknown | 4 | 1 | 20.0 (1.0-62.4) |
| Age group, y | |||
| 0-19 | 414 | 21 | 4.8 (3.2-7.3) |
| 0-12 | 220 | 6 | 2.7 (1.2-5.7) |
| 13-19 | 194 | 15 | 7.2 (4.4-11.5) |
| 20-39 | 3691 | 305 | 7.6 (6.8-8.5) |
| 40-59 | 3466 | 326 | 8.6 (7.7-9.5) |
| 60-79 | 2012 | 223 | 10.0 (8.8-11.3) |
| 80-115 | 237 | 30 | 11.2 (8.0-15.6) |
| Emergency departments in Seattlec | |||
| Total patients | 1653 | 279 | 14.4 (12.9-16.1) |
| Sex | |||
| Female | 717 | 107 | 13.0 (10.9-15.5) |
| Male | 936 | 172 | 15.5 (13.5-17.8) |
| Age group, y | |||
| 0-19 | 37 | 6 | 14.0 (6.6-27.3) |
| 0-12 | 9 | 0 | 0 (0-29.9) |
| 13-19 | 28 | 6 | 17.6 (8.3-33.5) |
| 20-39 | 517 | 57 | 9.9 (7.7-12.6) |
| 40-59 | 581 | 88 | 13.2 (19.8-15.9) |
| 60-79 | 405 | 94 | 18.8 (15.6-22.5) |
| 80-115 | 112 | 34 | 23.3 (17.2-30.8) |
| Unknown | 1 | 0 | 0 (0-94.9) |
Abbreviation: SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Samples were collected from 17 232 patients.
Samples were collected from 10 725 patients.
Samples were collected from 1932 patients.
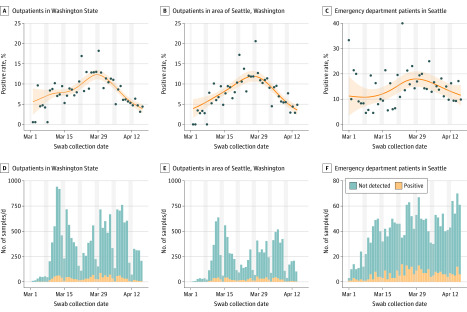
Figure. SARS-CoV-2 Positivity Rates and Amount of Samples Tested at Outpatient and Emergency Department Settings in Washington State.
The vertical gray shading indicates testing that occurred during the weekends (from 12 am on Saturday to 11:59 pm on Sunday). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) positivity (gray dots; determined using reverse transcriptase–polymerase chain reaction tests), estimated smooth trends (orange lines), and 95% CIs (light orange shading) appear in A-C. The number of samples tested appear in D-F.
Nonlinear trends were observed in the estimated smooth curves for outpatients in Washington State (part A of the Figure) and outpatients in the Seattle area (part B of the Figure), with SARS-CoV-2 positivity rates peaking around March 28-29, 2020, and then declining for both populations. The trajectory in Seattle ED patients showed a similar time to peak, followed by a more gradual decline (part C of the Figure). The SARS-CoV-2 positivity rate was 17.6% in the outpatient clinics and 14.3% in EDs at the peak period and 3.8% and 9.8%, respectively, at the end of the analysis period. Testing volumes steadily increased for the first half of March and, for outpatients, peaked around March 12-13, 2020 (parts D-E of the Figure), with fewer samples collected on the weekends.
Discussion
SARS-CoV-2 infections in patients seen in Washington outpatient clinics and Seattle ED settings peaked in late March and have been declining. This trajectory is aligned with local physical distancing guidelines (statewide shutdown of bars and restaurants; expanded social gathering limits enacted on March 16, 2020) and the “Stay Home, Stay Healthy” order announced by Governor Inslee on March 23, 2020.6
Testing criteria in Washington have not changed significantly during the study period, and testing remains largely limited to symptomatic persons. Testing volume in the study populations did not increase, likely due to shortages of sample collection materials, and the UW Virology Division has not reached maximum testing capacity since mid-March, so declining SARS-CoV-2 positivity is not attributed to expanded testing. This is not a population-based sample, and the mix of cases seen over time is not constant. The Seattle-area outpatient population analyzed is a subset of the Washington State outpatient population, and most of the samples were collected in the Northwest and South Puget Sound regions of Washington and therefore are not representative of the entire state.
These results suggest that the early and aggressive physical distancing measures enacted in Washington State have influenced the course of the COVID-19 pandemic. Whether adherence to physical distancing will continue and how that affects acquisition trends remain to be determined.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Holshue ML, DeBolt C, Lindquist S, et al. ; Washington State 2019-nCoV Case Investigation Team . First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929-936. doi: 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corman VM, Landt O, Kaiser M, et al. . Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3):1-8. doi: 10.2807/1560-7917.ES.2020.25.3.2000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): information for laboratories. Accessed March 1, 2020. https://www.cdc.gov/coronavirus/2019-ncov/lab/index.html
- 4.Wood SN. Generalized Additive Models: An Introduction With R. 2nd ed Chapman and Hall/CRC; 2017. doi: 10.1201/9781315370279 [DOI] [Google Scholar]
- 5.Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat. 1998;52:119-126. [Google Scholar]
- 6.Governor of Washington Proclamation by the Governor amending proclamation 20-05. Accessed March 25, 2020. https://www.governor.wa.gov/sites/default/files/proclamations/20-25%20Coronovirus%20Stay%20Safe-Stay%20Healthy%20%28tmp%29%20%28002%29.pdf