Abstract
The development of hypertension is associated with mitochondrial redox balance disruptions. NADP+-dependent isocitrate dehydrogenase 2 (IDH2) plays an important role in the maintenance of mitochondrial redox balance by producing mitochondrial NADPH, which is an essential cofactor in the reduction of glutathione (from GSSG to GSH) to reduced form of glutathione (GSH). We investigated the association of IDH2 between the development of prolonged high-fat diet (HFD)-induced hypertension. Idh2 gene-deleted (Idh2−/−) male mice and wild-type (Idh2+/+) littermates were fed either HFD or low-fat diet (LFD). Some mice were administrated with Mito-TEMPO, a mitochondria-specific antioxidant. HFD feeding increased blood pressure (BP) in both Idh2−/− mice and Idh2+/+ mice. HFD-induced BP increase was greater in Idh2−/− than Idh2+/+ mice. HFD intake decreased IDH2 activity, NADPH levels, and the GSH/(GSH + GSSG) ratio in the renal mitochondria. However, HFD intake increased mitochondrial ROS levels, along with the accompanying oxidative stress and damage. HFD intake increased angiotensin II receptor 1 type 1 mRNA levels in the kidneys and plasma renin and angiotensin II concentrations. These HFD-induced changes were more prominent in Idh2−/− mice than Idh2+/+ mice. Mito-TEMPO mitigated the HFD-induced changes in both Idh2−/− and Idh2+/+ mice, with greater effects in Idh2−/− mice than Idh2+/+ mice. These results indicate that prolonged HFD intake disrupts the IDH2-NADPH-GSH-associated antioxidant system and activates the renin-angiotensin system in the kidney, leading to increased BP, suggesting that IDH2 is a critical enzyme in the development of hypertension and that the IDH2-associated antioxidant system could serve as a potential hypertension treatment target.
Keywords: Isocitrate dehydrogenase 2, Hypertension, Mitochondria, Reactive oxygen species, Renin-angiotensin system
Graphical abstract
Highlights
-
•
High-fat diets impair the mitochondrial IDH2-NADPH-GSH antioxidant system.
-
•
IDH2 deletion exacerbates high-fat diet-induced blood pressure increases along with enhanced mitochondrial oxidative stress.
-
•
Mitochondria-targeted antioxidant prevents the effects of IDH2 deficiency.
-
•
IDH2 plays a critical role on the maintenance of mitochondrial redox balance in association with the development of hypertension.
Abbreviations and acronyms
- IDH2
Isocitrate dehydrogenase 2
- HFD
High-fat diet
- LFD
Low-fat diet
- GSH
Glutathione
- GSSG
Reduced glutathione
- GPx
Glutathione peroxidase
- GR
Glutathione reductase
- Trx
Thioredoxin
- Prx
Peroxiredoxin
- TrR
Thioredoxin reductase
- Ang II
Angiotensin II
- AGT
Angiotensinogen
- ACE
Angiotensin-converting enzyme
- AT1R
Angiotensin II type 1 receptor
1. Introduction
Hypertension, a multifactorial disease characterized by increased blood pressure (BP), is a risk factor for cardiovascular diseases [1]. Increased reactive oxygen species (ROS) production and elevated oxidative stress are believed to contribute to the development of hypertension [2]. Recently, many studies have emphasized the importance of mitochondria in the context of oxidative stress-associated hypertension [[2], [3], [4], [5], [6]]. Hence, the regulation of mitochondrial ROS and their scavenging system to reduce oxidative stress has been perceived as a promising approach to controlling hypertension and hypertension-associated diseases [[7], [8], [9]]. However, related mechanisms and effective therapeutic approaches based on ROS and oxidative stress remain to be defined.
Mitochondria are the major producers of ROS; however, they are also vulnerable to the ROS they produce [10]. Therefore, to cope with oxidative stress, mitochondria have their own specific antioxidant system. In normal conditions, the superoxide anion (O2-) generated during the process of mitochondrial energy production is converted to hydrogen peroxide (H2O2) by manganese superoxide dismutase (MnSOD) and then reduced to H2O by glutathione peroxidase (GPx) coupled to glutathione and glutathione reductase (GR), peroxiredoxin (Prx) coupled to thioredoxin (Trx) and thioredoxin reductase (TrR) [11,12]. In pathological conditions, including obesity, the mitochondrial ROS production exceeds ROS scavenging capacity, which can severely damage the ROS scavenging system, exposing the mitochondria to oxidative stress [[12], [13], [14], [15]]. Recent researches have demonstrated that mitochondrial redox imbalances are associated with the development of hypertension and that mitochondrial antioxidant reagents effectively diminish hypertension [3,9,16].
Mitochondrial NADPH is essential for the reduction of glutathione from GSSG to GSH in that it supplies the reducing equivalent [17,18]. GSH is required in the GPx- and thiol-based mitochondrial anti-oxidant system [12]. NADPH does not shuttle between the cytosol and mitochondria. Therefore, mitochondria have their own NADPH producing enzymes such as nicotinamide nucleotide transhydrogenase (NNT) and isocitrate dehydrogenase 2 (IDH2) [19,20]. IDH2, which was the focus of this study, consumes NADP+ during the catalysis of isocitrate to α-ketoglutarate in the tricarboxylic acid cycle and produces NADPH [21]. Three mammalian isocitrate dehydrogenases (IDHs), have been reported: IDH1, IDH2, and IDH3 [21,22]. IDH1 and IDH2 are NADP+-dependent, and they are found in the cytosol and mitochondria, respectively [22]. IDH3 is NAD+-dependent, and it is found in the mitochondria [22]. Therefore, IDH1 and IDH2 have been proposed as important NADPH producers in the cytoplasm and mitochondria, respectively, and also as major antioxidant enzymes. In fact, recently, other investigators and we found that IDH2 defect, exacerbates mitochondrial oxidative stress, whereas increased IDH2 activation provides mitochondrial resistance against oxidative stress [[23], [24], [25], [26], [27], [28]].
Obesity is a well-known risk factor for hypertension and approximately 65–70% of the risk for hypertension is associated with obesity-related diseases [29,30]. Obesity is associated with excessive ROS production during ATP generation in multiple organs, overwhelming their antioxidant capacity [15]. Studies have shown that obesity contributes to the development of hypertension and that increased ROS level and oxidative stress are associated with obesity-induced hypertension [29,31]. Recent studies including ours have shown that IDH2 plays an important role in the development of obesity [32,33]. These data suggest that IDH2 may be involved in the development of hypertension. However, the role of IDH2 in hypertension and its underlying mechanisms are yet to be defined. Therefore, in this present study, we investigated the role of IDH2 in the context of obesity-induced hypertension and found that prolonged high-fat diet (HFD) intake impairs the functioning of IDH2 and its related antioxidant system. We also found that IDH2 gene deletion exacerbates obesity-induced hypertension, whereas mitochondrial antioxidants supplied by HFD feeding attenuated blood pressure increases in mice. These results suggest that IDH2 is associated with obesity-induced hypertension and may be a useful therapeutic target protein for the development of hypertension treatment.
2. Materials and Methods
2.1. Animal preparation
Eight-week-old Idh2 knockout (Idh2−/−) male mice and wild-type (Idh2+/+) littermates weighing 20–25 g were used in these experiments. The Idh2−/− and Idh2+/+ mice were generated and characterized as previously described [34]. This study was conducted in accordance with the guidelines of the Institutional Animal Care and Use Committee of Kyungpook National University, Republic of Korea. Before the starting experiments, the mice were provided free access to water and standard chow. Mice were randomly assigned and fed with either an HFD containing 60% kcal from fat (TD.06414, Harlan Laboratories, Inc., Madison, WI, USA) or a low-fat diet (LFD) containing 10% kcal from fat (TD.94048, Harlan Laboratories). Some mice were injected intraperitoneally with (2-(2,2,6,6-Tetramethylpiperidin-1-oxyl-4-ylamino)-2-oxoethyl) triphenylphosphonium chloride (Mito-TEMPO, 0.7 mg/kg body weight; Sigma, St. Louis, MO, USA), a mitochondrial antioxidant reagent, once daily. Body weight and food intake were measured once a week after HFD or LFD feeding. The kidneys were either snap-frozen in liquid nitrogen or perfusion-fixed in PLP (4% paraformaldehyde, 75 mM l-lysine, and 10 mM sodium periodate; Sigma). More than 10 mice were used for the measurements of blood pressure and more than 6 mice were used for biochemical studies.
2.2. Measurement of blood pressure
Blood pressures (BPs) were measured using a CODA High Throughput Noninvasive BP system (CODA, Kent Scientific, Torrington, CT, USA) according to the manufacturer’s instruction. Briefly, conscious mice were preheated on a hot plate at 35 °C for 10 min and then placed in a restrainer. A cuff with a pneumatic pulse sensor was attached to the tail. BP values were recorded with heating, and the mean of ten consecutive readings was obtained from each mouse.
2.3. Analysis of mouse blood
Blood was withdrawn from the mice using a heparinized syringe. Plasma cholesterol, triglyceride (TG), and high-density lipoprotein (HDL) levels were determined using a VITROS 250 Chemistry Analyzer (Johnson & Johnson, Rochester, NY, USA) according to the manufacturer's instructions.
2.4. Preparation of cytosolic and mitochondrial fractions from tissue
Cytosolic and mitochondrial fractions were prepared as described previously [35]. Briefly, frozen kidney tissue was homogenized in sucrose buffer (0.2 M sucrose, 1 mM EGTA, 10 mM HEPES, pH 7.4; Sigma) on ice, three times using a Teflon Homogenizer (Daihan Scientific, Seoul, Korea) at 1,600 rpm. The homogenate was centrifuged at 600×g for 10 min, and then the supernatant was centrifuged at 7,000×g for 10 min. The supernatant comprised the cytosolic fraction, and it was centrifuged again at 7,000×g for 10 min, to purify the cytosolic fraction. The mitochondrial pellet was washed twice with sucrose buffer and was centrifuged again at 7,000×g for 10 min. The pellet was suspended in phosphate-buffered saline, containing 0.1% Triton X-100, disrupted twice with a sonicator (4710 series; Cole-Palmer, Chicago, IL, USA) at 40% of the maximum setting for 10 s, and centrifuged at 15,000×g for 30 min. The supernatant comprised the mitochondrial fraction, and it was used to measure enzymatic activity. Equal amounts of fractionated proteins were separated by SDS-PAGE and transferred to a PVDF membrane. Effective isolation of those fractions was confirmed by Western blot analysis, using antibodies against IDH2 or COX-IV protein for the mitochondrial fraction.
2.5. Western blot analysis
Protein samples were prepared as described previously [36]. Protein samples were electrophoresed and subjected to immunoblotting with antibodies against IDH2 [37], peroxiredoxin-SO3 (PrxSO3; Abcam, Cambridge, MA, USA), COX-IV (Abcam), and GAPDH (Novus, Littleton, CO, USA), and the blot densities were quantified using Image J software (National Institutes of Health, Bethesda, MD, USA).
2.6. Measurement of IDH2 activity in the renal mitochondrial fraction
IDH2 activity was measured in the kidney tissue mitochondrial fraction, as described previously [24]. Briefly, mitochondrial fraction (50 μg protein) was combined with a reaction mixture containing 40 mM Tris (pH 7.4), 2 mM NADP+, 2 mM MgCl2 and 50 mM threo-DS-isocitrate (Sigma), and NADPH production was measured. IDH2 activity was defined by the changes in absorbance at 340 nm per 1 mg of protein at 37 °C for 1 min. Mitochondrial fractionation was confirmed by Western blot analysis using COX-IV antibody.
2.7. Measurement of NADPH concentration in the renal mitochondrial fraction
NADPH concentration was determined using an EnzyChrom™ NADP/NADPH Assay Kit (BioAssay Systems, Hayward, CA, USA) according to the manufacturer’s instruction. In brief, freshly isolated mitochondrial tissue fractions were suspended in 100 μl NADPH extraction buffer for NADP determination or 100 μl NADPH extraction buffer for NADPH determination. Those mixtures were heated at 60 °C for 5 min and then 20 μl assay buffer and 100 μl of the opposite extraction buffer were added to neutralize the extracts. After centrifugation at 14,000 rpm for 5 min, the supernatant was used for measurement. In a 96-well plate, 40 μl samples were transferred and added 80 μl working reagent (60 μl assay buffer, 1 μl enzyme mix, 10 μl glucose, and 14 μl MTT). The plate was read at 565 nm at time zero and at 30 min. The concentration of NADP(H) was calculated using the change of optical density at 565 nm for 30 min. The sample NADP(H) concentration was determined using the standard curve.
2.8. Measurement of oxidized glutathione (GSSG) and total glutathione levels in the renal mitochondrial fraction
The ratio of oxidized glutathione (GSSG) to total glutathione (GSH + GSSG) was measured using an enzymatic recycling method, as previously described [35]. The amount of total glutathione was determined by analyzing the formation of 5-thio-2-nitrobenzoic acid (TBA) from 5,5-dithiobis (2-nitrobenzoic acid) (DTNB). GSSG was measured by adding 2-vinylpyridine, which inhibits TBA formation when DTNB and glutathione react. Total GSH and GSSG levels were defined by the changes in optical density at 412 nm for 1 min at 37 °C.
2.9. Measurement of H2O2 levels in the renal mitochondrial fraction
H2O2 levels in the mitochondrial fraction the kidney tissue were measured using xylenol orange (Sigma, St. Louis, MO, USA), a dye sensitive to ferric ions, as described previously [35].
2.10. Immunohistochemical staining
Immunohistochemical staining was performed using anti-8-hydroxy-2′-deoxyguanosine (8-OHdG; Abcam, Cambridge, MA, USA) antibody, as previously described [38]. The 8-OHdG-antibody binds to DNA damaged by oxidation in mitochondria and nuclei [39]. Sections were viewed under a Leica microscope (DM2500, Wetzlar, Germany). Photomicrographs were obtained randomly from the cortical region. The intensity of 8-OHdG stains were measured under 400X magnification using an image analysis program (i-solution, IMT, Korea).
2.11. Transmission electron microscopy (TEM)
Kidney TEM samples were prepared as described previously [35]. Briefly, kidneys were perfusion-fixed with 2.5% glutaraldehyde via the abdominal aorta, then stored overnight in the fixative at 4 °C. Samples were cut into 1 mm3 pieces, washed in 0.1 M phosphate buffer, and then post-fixed in aqueous 2% osmium tetroxide for 90 min. After three washes with 0.1 M phosphate buffer, the samples were dehydrated through a graded series of 50% to 100% ethanol, 100% propylene oxide, and then infiltrated in 1:1, 1:2, and 1:3 mixtures of propylene oxide: Epon Resin 828 (Polysciences Inc., Warrington, PA, USA) for 1 h. After the samples had been incubated in 100% Epon Resin 828 over 8 h, they were then embedded in molds and cured at 35 °C and 45 °C for 12 h, followed by additional hardening at 60 °C for 2 days. Ultrathin (60 nm) sections were double-stained with 2% uranyl acetate and 1% lead citrate. Sections were visualized using a transmission electron microscope (H-7000; Hitachi, Yokohama, Japan) at 75 kV. Electron micrographs of the mitochondria were captured from proximal tubule cells in the outer stripe of the outer medulla. The mitochondrial aspect ratio (major axis/minor axis) was computed using 30 mitochondria per cell.
2.12. Measurements of angiotensin II (AngII) and renin in plasma
Plasma was prepared from heparin-treated blood samples. Concentrations of plasma Ang II was measured using an Ang II ELISA kit (Phoenix Pharmaceuticals, INC., Burlingame, CA, USA) and renin was measured using a renin assay kit (BPS Bioscience, San Diego, CA, USA), according to the manufacturers’ instructions.
2.13. Quantitative real-time PCR analysis
RNA was extracted using Tri-RNA reagent (Favorgen, Pingtung, Taiwan) from homogenized kidneys. Next, 1 μg of RNA was used for cDNA synthesis using the DiaStar RT Kit (SolGent, Daejeon, Korea). Quantitative real-time PCR (qRT-PCR) was performed using SYBR Green I Master mix (Enzo Life Science, Farmingdale, NY, USA) and the Agilent Real-time PCR System (Agilent Technology, Santa Clara, CA, USA). Murine qRT–PCR primer sequences were 5′-CTCGAACTCAAAGCAGGAGAG-3′ and 5′-GTAGATGGCGAACAGGAAGG-3′ for angiotensinogen (AGT); 5′-GAACGAATCCCGCTCAAGA A-3′ and 5′-AGGAAGGCCTCTTTGTGAATAC-3′ for renin; 5′-GACAGGTTCGTGGAAGAGTATG-3′ and 5′-TTGCTGCCCTCTATGGTAATG-3′ for angiotensin converting enzyme (ACE); 5′-TGCCCATAACCATCTGCATA G-3′ and 5′-TTCAGGAGCTGGGGAAATAC-3′; for Ang II receptor type 1 (AT1R); and 5′-GTAACCCGTTGAACCCCATT-3′ and 5′-CCATCCAATCGGTAGTAGCG-3′ for 18S rRNA, sense and antisense, respectively.
2.14. Statistical analyses
All data were analyzed using GraphPad Prism 7 software (San Diego, CA, USA). Results are expressed as mean ± standard deviation (SD). Comparisons among groups were performed using ANOVA or unpaired Student's t‐test. Multiple groups at different time points were determined using two-way ANOVA. Blood pressures with Mito-TEMPO treatment were analyzed by three-way ANOVA with times, genotypes, and Mito-TEMPO treatment as factors. Differences were regarded as statistically significant when they had p values < 0.05.
3. Results
3.1. Idh2 gene deletion augments HFD-induced BP increases
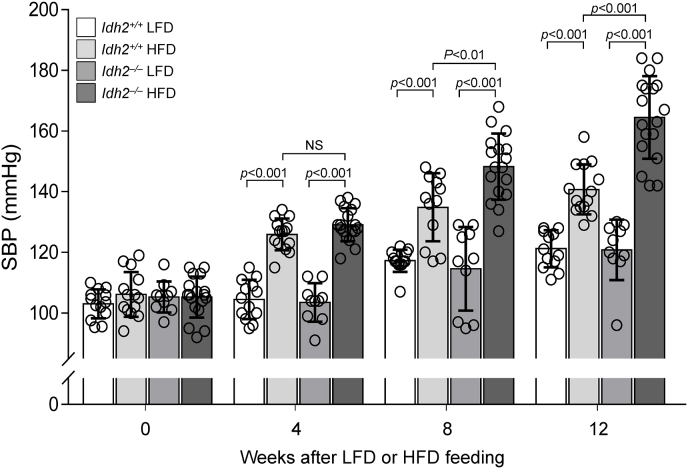
First, we measured blood pressure in normal chow-fed 8-week-old Idh2+/+ and Idh2−/− mice, before controlled diet (HFD or LFD) feedings (Fig. 1 and Supp. Tables 1 and 2). Systolic blood pressures (SBPs) were 105 ± 4.91 mmHg and 103 ± 4.80 mmHg for Idh2−/− mice and Idh2+/+ mice respectively, showing no significant difference between groups (Fig. 1). After HFD feeding, SBPs began increasing 4 weeks later, and they continuously increased at a statistically significant rate for 8 weeks (148.2 ± 10.87 mmHg in Idh2−/−; 135.9 ± 11.41 mmHg in Idh2+/+ mice) and reached means of 164.5 ± 13.66 mmHg and 140.7 ± 8.25 mmHg in Idh2−/− and Idh2+/+ mice 12 weeks, respectively (Fig. 1). This increase was significantly greater in Idh2−/− mice relative to Idh2+/+ mice at 12 weeks (p<0.001) (Fig. 1). After 12 weeks, LFD, SBPs of the LFD-fed both Idh2+/+ and Idh2−/− mice were slightly increased relative to the baseline measurements, but the changes were not statistically significant (Fig. 1). These data indicate that HFD feeding induce BP increases in both Idh2−/− and Idh2+/+ mice and that Idh2 deficiency exacerbates the BP increase.
Fig. 1.
Effect of IDH2 on systolic blood pressure (SBP) after high-fat diet feeding. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed a low-fat diet (LFD) or high-fat diet (HFD) for 12 weeks. SBP was measured using the tail-cuff method at indicated times. SBP values were obtained from ten consecutive readings at each mouse. Results are expressed as the mean ± standard deviation (n = 10–18). Statistical analysis was performed by two-way ANOVA with repeated measures followed by post hoc Bonferroni’s multiple comparisons test. LFD, low-fat diet; HFD, high-fat diet; NS, non-significance.
Before LFD and HFD feeding, body weights (BWs) did not significantly differ between Idh2+/+ and Idh2−/− mice (21.55 ± 0.43 g and 22.35 ± 0.50 g, respectively). BW of the Idh2−/− mice was lower than that of the Idh2+/+ mice, but this difference was not statistically significant (Table 1). Twelve weeks after LFD feeding, there was no significant differences in BW and WAT weight between Idh2+/+ and Idh2−/− mice (Table 1). Twelve weeks after the base line measurements, the plasma concentrations of cholesterol, high-density lipoprotein (HDL), and triglyceride (TG), as well as the visceral fat weights of both Idh2+/+ and Idh2−/− mice were greater in HFD-fed than those in LFD-fed mice (Table 1). These HDL and cholesterol levels were higher in Idh2−/− mice than Idh2+/+ mice (Table 1). However, there were no significant differences in serum HDL, TG, and cholesterol levels between Idh2−/− mice and Idh2+/+ mice 12 weeks of LFD feeding (Table 1).
Table 1.
The effects of high-fat diet feeding on body weight, kidney weight, visceral adipose tissue weight, cholesterol, triglyceride, and high-density lipoprotein levels. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed low-fat diet (LFD) or high-fat diet (HFD) for 12 weeks. Kidney and visceral white adipose tissue weight were measured after harvesting. Results are expressed as the mean ± standard deviation (n = 10–18). LFD, low-fat diet; HFD, high-fat diet. *, p<0.05 vs. respective LFD; †, p<0.05 vs. Idh2+/+ HFD.
| Idh2+/+ LFD | Idh2+/+ HFD | Idh2−/− LFD | Idh2−/− HFD | |
|---|---|---|---|---|
| Body weight (g) | 33.63 ± 1.76 | 47.01 ± 1.20* | 32.53 ± 0.92 | 45.65 ± 1.23* |
| Kidney weight (g) | 0.150 ± 0.007 | 0.169 ± 0.008 | 0.142 ± 0.009 | 0.184 ± 0.011* |
| Visceral WAT (g) | 1.206 ± 0.157 | 1.570 ± 0.168 | 1.162 ± 0.101 | 1.550 ± 0.067* |
| Cholesterol (mg/dl) | 136.75 ± 26.22 | 182.50 ± 20.85* | 155.33 ± 9.88 | 287.25 ± 16.67*† |
| HDL (mg/dl) | 95.00 ± 34.65 | 119.67 ± 13.00 | 107.33 ± 13.61 | 156.33 ± 2.25*† |
| Triglyceride (mf/dl) | 100.25 ± 8.69 | 113.00 ± 14.74 | 77.33 ± 6.33 | 121.50 ± 18.08* |
3.2. HFD-feeding reduces IDH2 activity and NADPH levels in the kidney mitochondria
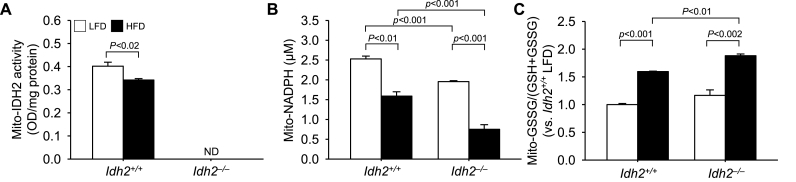
To test whether HFD feeding affects IDH2 function, we determined IDH2 activity in the mitochondrial fraction of Idh2+/+ and Idh2−/− mouse kidneys. IDH2 activity levels in HFD-fed Idh2+/+ mice were significantly lower than those in LFD-fed mice (Fig. 2A). IDH2 activity in Idh2−/− mouse kidney tissue was undetectable (Fig. 2A). IDH2 reduces the NADP+ to NADPH during the decarboxylation of isocitrate to α-ketoglutarate, and given this role, this is recognized as a key generator of NADPH in the mitochondria [22,23]. After 12 weeks of consuming different diets, we examined whether Idh2 gene deletion and HFD-feeding affect the NADPH production in the mitochondrial fraction from kidneys. The level of NADPH was also significantly lower in both HFD-fed Idh2+/+ and HFD-fed Idh2−/− mice than in LFD-fed control mice (Fig. 2B). After 12 weeks of HFD-feeding, NADPH levels of LFD-fed Idh2−/− mice and LFD-fed Idh2+/+ mice were lowered to 61.54% and 37.11% relative to the levels of found in LFD-fed mice, respectively (Fig. 2B). NADPH level in the LFD-fed Idh2−/− mouse kidneys was slightly lower than that in the LFD-fed Idh2+/+ mouse kidneys (Fig. 2B). Since NADPH plays a critical factor in the reduction of glutathione (GSH) from oxidized glutathione (GSSG) [17,18], we determined the ratio of GSSG to total glutathione (tGSH, GSSG + GSH) in the kidney mitochondria. After 12 weeks of HFD-feeding, the ratio of GSSG to tGSH in the mitochondria increased in both Idh2−/− mice and Idh2+/+ mice, but with a greater increase in Idh2−/− mice (Fig. 3A). The ratio of GSSG to tGSH in LFD-fed Idh2−/− mice was higher than that in the LFD-fed Idh2+/+ mice, but this difference was not statistically significant (Fig. 2C). These data indicate that HFD-feeding induces an attenuation of IDH2 activity, leading to decreased NADPH levels and subsequent increases of GSSG/(GSH + GSSG) ratio.
Fig. 2.
IDH2 activity, NADPH level and GSSG/(GSH + GSSG) ratio in the renal mitochondria after high-fat diet feeding. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed a low-fat diet (LFD) or high-fat diet (HFD) for 12 weeks and then the mice kidneys were harvested. The fractionations of mitochondria from kidney tissues were performed as described in the Materials and Methods section. Mitochondrial fractionations were confirmed by Western blot analysis using an anti-COX-IV antibody. (A) IDH2 activities and (B) NADPH concentrations were measured in the mitochondrial fractions of kidneys (C) The ratio of oxidized glutathione (GSSG) to total glutathione (GSH + GSSG) were determined in the mitochondrial fractions. Results are expressed as the mean ± standard deviation (n = 6). LFD, low-fat diet; HFD, high-fat diet; ND, non-detection.
Fig. 3.
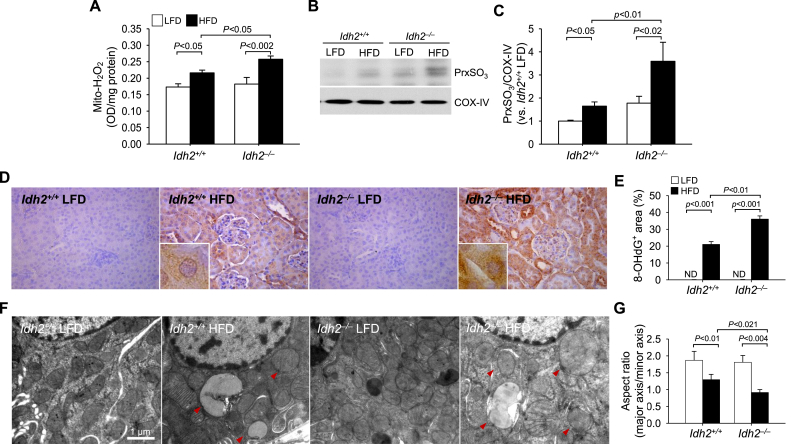
Mitochondrial H2O2and oxidative stress levels, and mitochondrial damage in the kidneys of Idh2+/+and Idh2−/−mice after high-fat diet feeding. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed a low-fat diet (LFD) or high-fat diet (HFD) for 12 weeks. And then the mouse kidneys were frozen in a liquid nitrogen or fixed in PLP solution for biochemical and histological studies, respectively. (A) H2O2 levels were determined in the mitochondrial fractions of kidney tissues. Mitochondrial fractionations were confirmed by Western blot analysis using an anti-COX-IV antibody. (B) PrxSO3 expressions were determined in the kidney mitochondrial fractions by Western blot analysis using an anti-PrxSO3 antibody. COX-IV was used as a loading control for the mitochondrial fraction. (D) Fixed kidney tissues were cut 3 μm thickness using a microtome and then kidney sections were subjected to immunohistochemical staining using an anti-8-OHdG antibody. Images were taken from the cortical lesions. Brown colors are 8-OHdG-positive signals. Inserts are at high magnifications. (E) Intensities of 8-OHdG stains were measured under 400X magnification using an image analysis program (i-solution). (F) Six weeks after the initiation of HFD, mitochondrial structures were evaluated under transmission electron microscopy (TEM). Red arrowheads indicate damaged mitochondrial structures. (G) The aspect ratio (major axis/minor axis) of mitochondria in the TEM pictures was measured. Results are expressed as the mean ± standard deviation (n = 6). LFD, low-fat diet; HFD, high-fat diet.
3.3. HFD-feeding increases H2O2 levels, oxidative stress, and damage in the kidney mitochondria
To investigate whether the reduced IDH2-NADPH-GSH-coupled mitochondrial antioxidant system affects mitochondrial redox balance, we determined the levels of H2O2, and the expression of oxidized Prx (PrxSO3, a form of oxidized Prx) and 8-OHdG, an indicator of DNA oxidation, in the kidneys. HFD feeding for 12 weeks increased H2O2 levels in the mitochondrial fractions of both Idh2−/− and Idh2+/+ mouse kidneys and the increase of H2O2 level was higher in Idh2−/− mice than Idh2+/+ mice (Fig. 3A). PrxSO3 expression also increased in the kidneys of both Idh2+/+ and Idh2−/− mice after 12 weeks of HFD feeding and this increase was greater in Idh2−/− mice than in Idh2+/+ mice (Fig. 3B and C). When DNA oxidation was determined by immunostaining with 8-OHdG antibody, 8-OHdG-positive signals were observed in both the cytosol and nuclei of tubular cells of both Idh2−/− and Idh2+/+ mice 12 weeks after HFD-feeding, indicating that mitochondrial and nuclear DNAs are damaged oxidatively. The positive signal of 8-OHdG antibody was also greater in Idh2−/− mice than Idh2+/+ mice (Fig. 3D and E). After LFD-feeding, the levels of H2O2, DNA oxidation, and PrxSO3 expression were slightly higher in Idh2−/− mice than Idh2+/+ mice (Fig. 3A). These data indicate that HFD intake increases mitochondrial ROS production and oxidative stress and that IDH2 deficiency exacerbates these increases.
To evaluate whether impairment of the mitochondrial IDH2-NADPH-GSH anti-oxidative system is associated with functional and structural damage to mitochondria, we determined the mitochondrial dynamics and morphology and IDH2 activity in kidney proximal tubule cells 6 weeks after the initiation of HFD-feeding, when SBP started to increase. Six weeks after the initiation of HFD feeding, transmission electron microscopy (TEM) data revealed swelling of mitochondria with cristae loss and mitochondrial membrane disruption in both Idh2−/− and Idh2+/+ mouse kidneys (Fig. 3F), representing decreases of the mitochondrial aspect ratio (the ratio between the major and minor axis of the ellipse equivalent to the mitochondrion) (Fig. 3F and G). These mitochondrial structural changes and the decrease in aspect ratio were greater in HFD-fed Idh2−/− mice than Idh2+/+ mice (Fig. 3F). There was no significant difference in mitochondrial aspect ratio between Idh2+/+ and Idh2−/− kidneys 6 weeks after LFD-feeding (Fig. 3G). These results indicate that HFD feeding induces mitochondrial damage, suggesting that HFD-induced mitochondrial damage is a risk factor for HFD-induced hypertension.
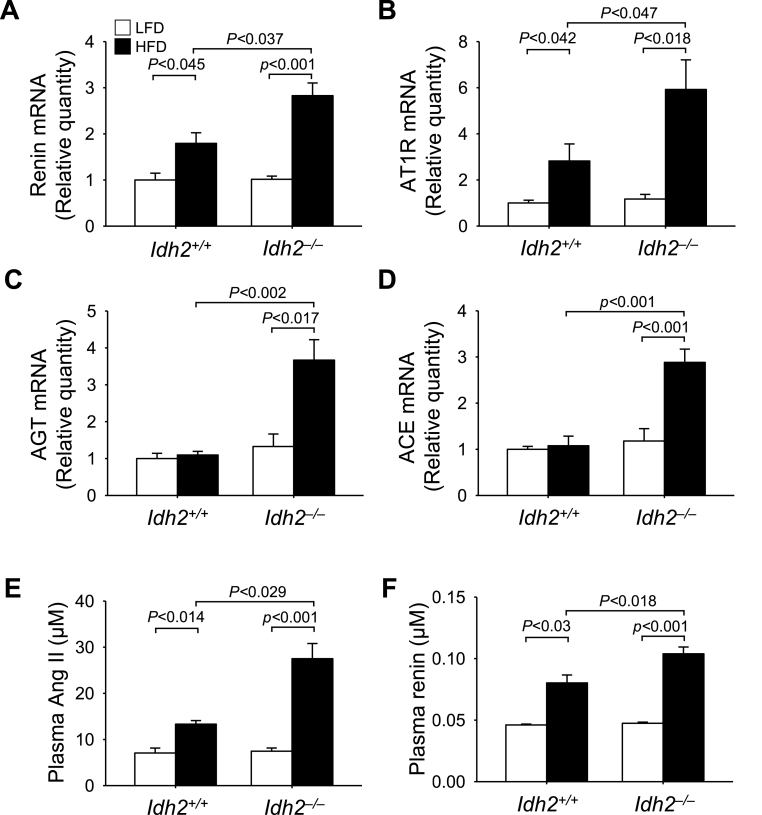
3.4. Idh2 deletion exacerbates HFD-induced renin-angiotensin system (RAS) activation in the kidney
ROS and oxidative stress affect the RAS both locally and systemically, and this strongly influences the development of hypertension [[40], [41], [42], [43]]. Therefore, we determined whether Idh2 gene deletion and HFD-feeding affect kidney RAS components, including angiotensinogen (AGT), renin, angiotensin-converting enzyme (ACE), and angiotensin II type I receptor (AT1R) and discovered the following. After 12 weeks of HFD-feeding renin and AT1R mRNA levels increased in both Idh2−/− and Idh2+/+ mouse kidneys (Fig. 4A and B), with a greater increase in Idh2−/− mice (Fig. 4A and B). AGT and ACE mRNA levels significantly increased in the Idh2−/− mouse kidneys after 12 weeks of HFD-feeding (Fig. 4C and D); however, they were not significantly increased in Idh2+/+ mouse kidneys (Fig. 4C and D). Plasma angiotensin II (Ang II) and renin concentrations increased in both Idh2+/+ and Idh2−/− mice after 12 weeks of HFD-feeding (Fig. 4E and F) and these increases were much greater in the Idh2−/− mice than in the Idh2+/+ mice (Fig. 4E and F). In contrast, there were no significant differences in AGT, AT1R, ACE, and renin mRNA levels and plasma Ang II and renin concentrations in between LFD-fed Idh2−/− and Idh2+/+ mice (Fig. 4E and F). These results indicate that HFD feeding activates the RAS, and Idh2 gene deletion accentuates this activation.
Fig. 4.
Renin-angiotensin system component mRNA expression in the kidney and angiotensin II and renin concentrations in the blood of Idh2+/+and Idh2−/−mice after high-fat diet feeding. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed a low-fat diet (LFD) or high-fat diet (HFD) for 12 weeks and then harvested. mRNAs were extracted from kidney tissues using RNA extraction solution as described in the Materials and Methods. The mRNA levels of renin (A), angiotensin II type 1 receptor (AT1R) (B), angiotensinogen (AGT, C), and angiotensin-converting enzyme (ACE, D) were measured in the kidneys. mRNA levels were normalized by 18S rRNA levels. Plasma concentrations of angiotensin II (Ang II, E) and renin (F) were determined 12 weeks after initiating HFD feeding. Results are expressed as the mean ± standard deviation (n = 6). LFD, low-fat diet; HFD, high-fat diet.
3.5. Mito-TEMPO treatment inhibits HFD-induced increases of BP, H2O2, and RAS components in both Idh2−/− and Idh2+/+ mice, with greater attenuation in Idh2−/− mice
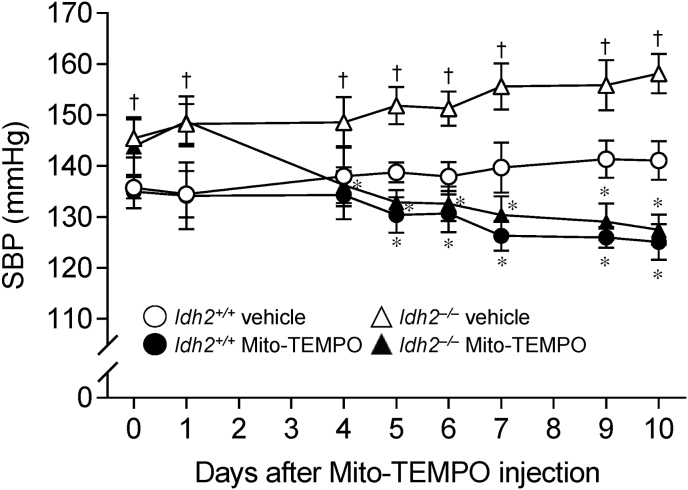
To determine whether the greater BP increases in Idh2−/− mice after HFD feeding were due to greater increases of mitochondrial ROS level and RAS activation, we investigated whether Mito-TEMPO, a mitochondria-specific O2− scavenger, could prevent BP increases after HFD feeding as well as the effects of Idh2 gene deletion. Either Mito-TEMPO (0.7 mg/kg/day) or vehicle (saline) was administered to the mice daily, for 10 days, 8 weeks after the initiation of HFD feeding. First, we determined SBP in those mice. Mito-TEMPO treatment significantly lowered the SBPs in both Idh2+/+ and Idh2−/− mice after HFD-feeding when compared with vehicle treatment, and the reduction in Idh2−/− mice was much greater than that in Idh2+/+ mice (Fig. 5 and Supp. Tables 3 and 4). Ten days after Mito-TEMPO, SBPs in the Idh2−/− mice were similar with those in the Idh2+/+ mice (Fig. 5).
Fig. 5.
Effect of Mito-TEMPO treatment on blood pressure after the onset of hypertension in Idh2+/+and Idh2−/−mice. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed low-fat diet (LFD) or high-fat diet (HFD) for 10 weeks. The mice received either Mito-TEMPO (0.7 mg/kg/day) or vehicle (saline) for 10 days from 8 weeks after the initiation of HFD feeding, daily. Systolic blood pressures were measured as described in the Materials and Methods at the indicated time points. Statistical analysis was performed by three-way ANOVA with repeated measures. Results are expressed as the mean ± standard deviation (n = 10–15). LFD, low-fat diet; HFD, high-fat diet. *, p<0.05 vs. respective HFD vehicle; †, p<0.05 vs. Idh2+/+ HFD vehicle.
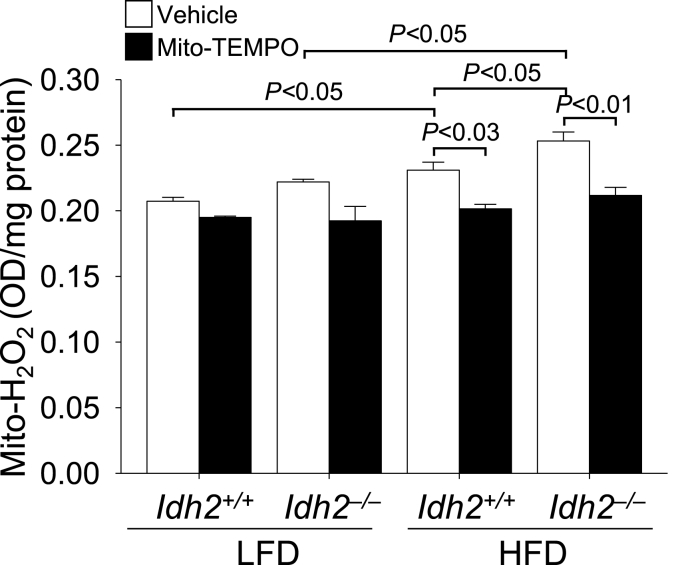
Next, we determined the H2O2 level in the mitochondrial fraction of the Mito-TEMPO-administered mice kidney tissues. After 12 weeks of HFD feeding H2O2 levels increased in the mitochondrial fractions of both Idh2−/− and Idh2+/+ mouse kidneys and the increase of H2O2 level was higher in Idh2−/− mice than Idh2+/+ mice (Fig. 6). Mito-TEMPO treatment completely prevented HFD-induced increases of H2O2 in both Idh2+/+ and Idh2−/− mice, with a greater effect in the Idh2−/− mice (Fig. 6). Mito-TEMPO treatment also reduced the kidney H2O2 levels in both Idh2+/+ and Idh2−/− mice fed with LFD (Fig. 6). These data indicate that the mitochondrial-targeted O2− scavenger Mito-TEMPO attenuates HFD-induced BP increases, also Idh2 gene-deletion induced BP increases, suggesting that the increases of mitochondrial ROS and oxidative stress are mediated the HFD- and Idh2 gene deletion-induced hypertension.
Fig. 6.
Effect of Mito-TEMPO treatment on hydrogen peroxide level in the kidney after high-fat diet feeding. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed low-fat diet (LFD) or high-fat diet (HFD) for 10 weeks. The mice received either Mito-TEMPO (0.7 mg/kg/day) or vehicle (saline) for 10 days from 8 weeks after the initiation of HFD feeding, daily. H2O2 levels were measured in the mitochondrial fractions from kidney tissues of Idh2+/+ and Idh2−/− LFD or HFD-fed mice. Mitochondrial fractionations were confirmed by Western blot analysis using an anti-COX-IV antibody. Results are expressed as the mean ± standard deviation (n = 6). LFD, low-fat diet; HFD, high-fat diet.
Finally, we examined the effect of Mito-TEMPO on HFD-induced RAS activation. HFD-feeding for 12 weeks increased renin and AT1R mRNA levels in both Idh2−/− and Idh2+/+ mouse kidneys (Fig. 7A and B), with a greater increase in Idh2−/− mice (Fig. 7A and B). AGT and ACE mRNA levels significantly increased in the Idh2−/− mouse kidneys after 12 weeks of HFD-feeding (Fig. 7C and D), whereas there were no significant differences between LFD- and HFD-feeding in Idh2+/+ mouse kidneys (Fig. 7C and D). Mito-TEMPO treatment inhibited HFD-induced increases renin and AT1R mRNA levels in the kidneys of both Idh2+/+ and Idh2−/− mice (Fig. 7A to D). These inhibitory effects were greater in Idh2−/− mice than Idh2+/+ mice (Fig. 7A to D). Also, Mito-TEMPO treatment inhibited HFD-induced increases of plasma Ang II and renin concentration in both Idh2+/+ and Idh2−/− mice, with greater inhibition in Idh2−/− mice (Fig. 7E and F). These results indicate that HFD-induced BP increases are associated with mitochondrial oxidative stress and IDH2 may play a preventive role against HFD-induced mitochondrial oxidative stress.
Fig. 7.
Effect of Mito-TEMPO treatment on RAS component mRNA expression after high-fat diet feeding. Eight-week-old Idh2+/+ and Idh2−/− male mice were fed low-fat diet (LFD) or high-fat diet (HFD) for 10 weeks. The mice received either Mito-TEMPO (0.7 mg/kg/day) or vehicle (saline) for 10 days from 8 weeks after the initiation of HFD feeding, daily. mRNAs were extracted from kidney tissues using RNA extraction solution as described in the Materials and Methods. The mRNA levels of renin (A), angiotensin II type 1 receptor (AT1R) (B), angiotensinogen (AGT, C) and angiotensin converting enzyme (ACE, D) were measured in the kidneys. mRNA levels were normalized by 18S rRNA levels. Plasma concentrations of angiotensin II (Ang II, E) and renin (F) were determined. Results are expressed as the mean ± standard deviation (n = 6). LFD, low-fat diet; HFD, high-fat diet.
4. Discussion
We demonstrated, for the first time, that 1) prolonged HFD intake impairs IDH2 function and the IDH2-associated mitochondrial antioxidant system in the kidney, resulting in increases of mitochondrial ROS levels and oxidative stress; 2) Idh2 gene deletion exacerbates HFD-induced BP elevation along with augmented mitochondrial oxidative stress, local kidney RAS production, and plasma Ang II and renin concentrations; and 3) mitochondrial antioxidant treatment mitigates prolonged HFD-induced BP elevation, with a greater mitigation in Idh2 gene-deleted mice relative to wild-type littermates. These findings indicate that IDH2 and its related antioxidant system are involved in the development and progression of hypertension, suggesting that IDH2 could be a useful target for the development of effective preventives and therapeutic agents for hypertension.
Under conditions associated with metabolic imbalances, including obesity, mitochondrial ROS levels greatly increase due to excessive mitochondrial ROS formation [15]. As ROS formation overwhelms the ROS eliminating capacity, mitochondrial components including antioxidant enzymes are impaired, leading to high levels of ROS production and ROS-induced oxidative stress in mitochondrial components. IDH2 is an essential enzyme for the formation of mitochondrial GSH, as it supplies the NADPH necessary to the process of reducing GSSG to GSH [28,44]. GSH is essential for GPx and the non-enzymatic ROS scavenging system in the mitochondria [12]. Furthermore, NADPH produced by IDH2 also plays an important role in the antioxidant function of Trx through the reduction of oxidized thioredoxin [26,28,44,45]. In fact, it has been shown that IDH2 dysfunction and deficiency increase mitochondrial vulnerability to oxidative stress [27,28,32,45]. Several studies have demonstrated that NADPH-linked substrates mitigate oxidative stress in mitochondria [19,46]. In adipose tissue we found that Idh2 gene deletion exacerbates HFD-induced ROS production and oxidative stress along with the decline in NADPH [47]. In the present study, HFD intake led to the diminution of IDH2 function and NADPH levels in the kidney mitochondria of kidney. Although, in the mitochondria, NADPH is produced by other sources, such as NNT [19]. In the present study, HFD intake was associated with a significant decline in NADPH in the kidney mitochondria of both Idh2 gene-deleted mice and wild-type mice, with a greater decline in the Idh2 gene deleted mice. Additionally, Idh2 gene deletion without HFD feeding also diminished NADPH levels in the mitochondria. These results indicate that HFD-induced inhibition of IDH2 function might not be compensated for by other mitochondrial sources, such as NNT and that Idh2 gene deletion-induced diminution of NADPH level also could not be compensated for by the NADPH produced by other enzymes. Furthermore, cytosolic NADPH does not shuttle between the mitochondria and the cytosol [19,20]. Therefore, the HFD-induced decline in mitochondrial NADPH may be directly associated with IDH2 function, suggesting that IDH2 is a critical enzyme for the maintenance of mitochondrial NADPH levels and redox balance during periods of prolonged HFD consumption. Supporting this, Ogura et al. recently reported that high glucose levels in cultured proximal tubular cells inhibit IDH2 activity, leading to decreased NADPH levels and increased GSSG to GSH ratios in mitochondria [48]. In contrast, Someya et al. reported that, in ear cells, caloric restriction lessens oxidative stress through increases of IDH2 activity, leading to increased NADPH levels and an increased ratio of GSH to GSSG [49]. Recently, Wang et al. reported that the renal mitochondria of rats with diabetes mellitus, contained high levels of acetylated IDH2 relative to the mitochondria of rat without diabetes mellitus, and this increase in acetylated IDH2 decreased IDH2 function in the kidney mitochondria [50]. Additionally, the normalization of acetylated IDH2 ameliorated oxidative stress on the kidneys and obesity-induced kidney damage [50]. In the brown adipose tissue, we also found that Idh2 gene deletion exacerbates HFD-induced lysine acetylation, and that this acetylation is inhibited by antioxidant treatment [47]. In the present study, although we do not exactly elucidate how prolonged consumption of an HFD impairs IDH2 function, our data clearly indicate that high-fat intake induces an IDH2 functional defect. Additionally, IDH2 is required to cope with ROS overproduction. These results suggest that prolonged high-fat intake disrupts mitochondrial IDH2 function, and this diminished IDH2 function is implicated in the development of hypertension via the increase of mitochondrial oxidative stress.
HFD-induced BP elevations are associated with the disruption of redox balance [6]. There is evidence that antioxidant supplements, such as Cu/Zn-SOD protein, or inhibitors of ROS-producing enzymes, such as NADPH oxidase and xanthine oxidase, lower BP, whereas pro-oxidant supplements raise BP [7,[51], [52], [53]]. In the present study, we observed that HFD feeding impaired IDH2 function and increased mitochondrial ROS levels and oxidative stress, resulting in disrupted mitochondrial dynamics and mitochondrial damage in kidney proximal tubule cells. Moreover, Idh2 gene deletion exacerbated this HFD-induced mitochondrial damage. These results indicate that IDH2 is a critical enzyme for the maintenance of mitochondrial homeostasis via redox balance regulation and that HFD feeding induced BP elevation is, at least partly, mediated by diminished IDH2 function and the subsequent loss of mitochondrial homeostasis. Supporting this, supplementation with the mitochondrial antioxidant, Mito-TEMPO, significantly inhibited HFD-induced BP elevations and mitochondrial oxidative stress in both Idh2−/− and Idh2+/+ mice, with greater inhibition in the Idh2−/− mice. Studies have demonstrated that HFD consumption induces mitochondrial fission [54]. Conversely, nutrient depletion activates mitochondria fusion [55]. In the present study, HFD feeding increased mitochondrial fission, and this fission was greater in Idh2−/− mice than Idh2+/+ mice, suggesting that IDH2 protects mitochondria against HFD-induced mitochondrial fission.
The local and circulating RAS components have been well recognized as the most important vasoactive hormonal factors for BP regulation and hypertension onset. Additionally, RAS activation has been widely accepted as an important contributor to mitochondrial ROS formation and oxidative stress [[56], [57], [58]]. Recent studies have demonstrated that increased ROS production and mitochondrial oxidative stress caused by excessive weight gain activate the RAS [57,58]. Hsieh et al. reported that H2O2 stimulates AGT mRNA expression in kidney proximal tubule cells, whereas treatment with MnSOD mimetic inhibits AGT mRNA expression [40]. Abdo et al. reported that catalase overexpression reduces AGT expression in kidney tubule cells [59]. In line with those findings, in the present study, we found that HFD-feeding increased renin and Ang II concentrations in the blood and renin and AT1R mRNA levels in the kidneys, and that these increases were larger in Idh2−/− mice than in Idh2+/+ mice. These results show that Idh2 deficiency enhances systemic and renal RAS system activation after HFD. We also found that mitochondrial antioxidant treatment inhibited the HFD-induced changes in both Idh2−/− and Idh2+/+ mice, with a greater inhibitory effect in the Idh2−/− mice. These data indicate that mitochondria-generated ROS and oxidative stress activates the renal RAS and that this activation may elevate BP.
Recently we observed that IDH2 deficiency decreased nitric oxide concentration in endothelial cells and impaired endothelium-dependent vaso-relaxation through increased mitochondrial oxidative stress; we also observed that changes were prevented by Mito-TEMPO [25]. Additionally, we found that IDH2 deficiency in mice caused cardiac hypertrophy through increased mitochondrial oxidative stress [27]. These results suggest that HFD feeding-induced hypertension could be associated with vascular dysfunction and cardiac hypertrophy. Taken together, our data clearly show that IDH2 is a critical enzyme for the maintenance of mitochondrial redox balance in obesity, and that prolonged high-fat intake impairs the IDH2-NADPH-GSH antioxidant system, resulting in mitochondrial oxidative damage, while the prevention of mitochondrial oxidative damage attenuated obesity-induced BP elevation. These data indicate that IDH2 may be a useful target protein for the development of effective therapeutics for hypertension. However, further studies are required to determine how prolonged high-fat intake impairs the IDH2-NADPH-GSH antioxidant system. To our knowledge, this is the first report demonstrating how prolonged high-fat intake impairs IDH2 function and subsequently leads to mitochondrial dysfunction.
Source of funding
This research was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare (grant number: HI15C0001), and National Research Foundation of Korea (NRF) Grant (NRF-2017R1A2A2A05069707) funded by the Korean government (MIST).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.redox.2020.101548.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Petrie J.R., Guzik T.J., Touyz R.M. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can. J. Cardiol. 2018;34(5):575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baradaran A., Nasri H., Rafieian-Kopaei M. Oxidative stress and hypertension: possibility of hypertension therapy with antioxidants. J. Res. Med. Sci. 2014;19(4):358–367. [PMC free article] [PubMed] [Google Scholar]
- 3.Dikalov S.I., Ungvari Z. Role of mitochondrial oxidative stress in hypertension. Am. J. Physiol. Heart Circ. Physiol. 2013;305(10):H1417–H1427. doi: 10.1152/ajpheart.00089.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Touyz R.M. Reactive oxygen species, vascular oxidative stress, and redox signaling in hypertension: what is the clinical significance? Hypertension. 2004;44(3):248–252. doi: 10.1161/01.HYP.0000138070.47616.9d. [DOI] [PubMed] [Google Scholar]
- 5.Rodrigo R., Gonzalez J., Paoletto F. The role of oxidative stress in the pathophysiology of hypertension. Hypertens. Res. 2011;34(4):431–440. doi: 10.1038/hr.2010.264. [DOI] [PubMed] [Google Scholar]
- 6.Lahera V., de Las Heras N., Lopez-Farre A., Manucha W., Ferder L. Role of mitochondrial dysfunction in hypertension and obesity. Curr. Hypertens. Rep. 2017;19(2):11. doi: 10.1007/s11906-017-0710-9. [DOI] [PubMed] [Google Scholar]
- 7.Dikalova A.E., Bikineyeva A.T., Budzyn K., Nazarewicz R.R., McCann L., Lewis W., Harrison D.G., Dikalov S.I. Therapeutic targeting of mitochondrial superoxide in hypertension. Circ. Res. 2010;107(1):106–116. doi: 10.1161/CIRCRESAHA.109.214601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montezano A.C., Touyz R.M. Reactive oxygen species, vascular Noxs, and hypertension: focus on translational and clinical research. Antioxidants Redox Signal. 2014;20(1):164–182. doi: 10.1089/ars.2013.5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dikalov S.I., Dikalova A.E. Contribution of mitochondrial oxidative stress to hypertension. Curr. Opin. Nephrol. Hypertens. 2016;25(2):73–80. doi: 10.1097/MNH.0000000000000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stallons L.J., Funk J.A., Schnellmann R.G. Mitochondrial homeostasis in acute organ failure. Curr Pathobiol Rep. 2013;1(3) doi: 10.1007/s40139-013-0023-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birben E., Sahiner U.M., Sackesen C., Erzurum S., Kalayci O. Oxidative stress and antioxidant defense. World Allergy Organ J. 2012;5(1):9–19. doi: 10.1097/WOX.0b013e3182439613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mari M., Morales A., Colell A., Garcia-Ruiz C., Fernandez-Checa J.C. Mitochondrial glutathione, a key survival antioxidant. Antioxidants Redox Signal. 2009;11(11):2685–2700. doi: 10.1089/ars.2009.2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tabara L.C., Poveda J., Martin-Cleary C., Selgas R., Ortiz A., Sanchez-Nino M.D. Mitochondria-targeted therapies for acute kidney injury. Expet Rev. Mol. Med. 2014;16:e13. doi: 10.1017/erm.2014.14. [DOI] [PubMed] [Google Scholar]
- 14.Yang Y., Liu H., Liu F., Dong Z. Mitochondrial dysregulation and protection in cisplatin nephrotoxicity. Arch. Toxicol. 2014;88(6):1249–1256. doi: 10.1007/s00204-014-1239-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Furukawa S., Fujita T., Shimabukuro M., Iwaki M., Yamada Y., Nakajima Y., Nakayama O., Makishima M., Matsuda M., Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Invest. 2004;114(12):1752–1761. doi: 10.1172/JCI21625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leskov I., Neville A., Shen X., Pardue S., Kevil C.G., Granger D.N., Krzywanski D.M. Nicotinamide nucleotide transhydrogenase activity impacts mitochondrial redox balance and the development of hypertension in mice. J Am Soc Hypertens. 2017;11(2):110–121. doi: 10.1016/j.jash.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Leonardi R., Subramanian C., Jackowski S., Rock C.O. Cancer-associated isocitrate dehydrogenase mutations inactivate NADPH-dependent reductive carboxylation. J. Biol. Chem. 2012;287(18):14615–14620. doi: 10.1074/jbc.C112.353946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park S.Y., Lee S.M., Shin S.W., Park J.W. Inactivation of mitochondrial NADP+-dependent isocitrate dehydrogenase by hypochlorous acid. Free Radic. Res. 2008;42(5):467–473. doi: 10.1080/10715760802098834. [DOI] [PubMed] [Google Scholar]
- 19.Rydstrom J. Mitochondrial NADPH, transhydrogenase and disease. Biochim. Biophys. Acta. 2006;1757(5–6):721–726. doi: 10.1016/j.bbabio.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Korge P., Calmettes G., Weiss J.N. Increased reactive oxygen species production during reductive stress: the roles of mitochondrial glutathione and thioredoxin reductases. Biochim. Biophys. Acta. 2015;1847(6–7):514–525. doi: 10.1016/j.bbabio.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smolkova K., Jezek P. The role of mitochondrial NADPH-dependent isocitrate dehydrogenase in cancer cells. Int J Cell Biol. 2012;2012:273947. doi: 10.1155/2012/273947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reitman Z.J., Yan H. Isocitrate dehydrogenase 1 and 2 mutations in cancer: alterations at a crossroads of cellular metabolism. J. Natl. Cancer Inst. 2010;102(13):932–941. doi: 10.1093/jnci/djq187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jo S.H., Son M.K., Koh H.J., Lee S.M., Song I.H., Kim Y.O., Lee Y.S., Jeong K.S., Kim W.B., Park J.W., Song B.J., Huh T.L. Control of mitochondrial redox balance and cellular defense against oxidative damage by mitochondrial NADP+-dependent isocitrate dehydrogenase. J. Biol. Chem. 2001;276(19):16168–16176. doi: 10.1074/jbc.M010120200. [DOI] [PubMed] [Google Scholar]
- 24.Kim J., Kim J.I., Jang H.S., Park J.W., Park K.M. Protective role of cytosolic NADP(+)-dependent isocitrate dehydrogenase, IDH1, in ischemic pre-conditioned kidney in mice. Free Radic. Res. 2011;45(7):759–766. doi: 10.3109/10715762.2011.577426. [DOI] [PubMed] [Google Scholar]
- 25.Park J.B., Nagar H., Choi S., Jung S.B., Kim H.W., Kang S.K., Lee J.W., Lee J.H., Park J.W., Irani K., Jeon B.H., Song H.J., Kim C.S. IDH2 deficiency impairs mitochondrial function in endothelial cells and endothelium-dependent vasomotor function. Free Radic. Biol. Med. 2016;94:36–46. doi: 10.1016/j.freeradbiomed.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 26.Park J.H., Ku H.J., Lee J.H., Park J.W. Idh2 deficiency exacerbates acrolein-induced lung injury through mitochondrial redox environment deterioration. Oxid Med Cell Longev. 2017;2017:1595103. doi: 10.1155/2017/1595103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ku H.J., Ahn Y., Lee J.H., Park K.M., Park J.W. IDH2 deficiency promotes mitochondrial dysfunction and cardiac hypertrophy in mice. Free Radic. Biol. Med. 2015;80:84–92. doi: 10.1016/j.freeradbiomed.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 28.Han S.J., Jang H.S., Noh M.R., Kim J., Kong M.J., Kim J.I., Park J.W., Park K.M. Mitochondrial NADP(+)-Dependent isocitrate dehydrogenase deficiency exacerbates mitochondrial and cell damage after kidney ischemia-reperfusion injury. J. Am. Soc. Nephrol. 2017;28(4):1200–1215. doi: 10.1681/ASN.2016030349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kotchen T.A. Obesity-related hypertension: epidemiology, pathophysiology, and clinical management. Am. J. Hypertens. 2010;23(11):1170–1178. doi: 10.1038/ajh.2010.172. [DOI] [PubMed] [Google Scholar]
- 30.Hall J.E., Crook E.D., Jones D.W., Wofford M.R., Dubbert P.M. Mechanisms of obesity-associated cardiovascular and renal disease. Am. J. Med. Sci. 2002;324(3):127–137. doi: 10.1097/00000441-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Dobrian A.D., Davies M.J., Schriver S.D., Lauterio T.J., Prewitt R.L. Oxidative stress in a rat model of obesity-induced hypertension. Hypertension. 2001;37(2 Pt 2):554–560. doi: 10.1161/01.hyp.37.2.554. [DOI] [PubMed] [Google Scholar]
- 32.Lee S.J., Kim S.H., Park K.M., Lee J.H., Park J.W. Increased obesity resistance and insulin sensitivity in mice lacking the isocitrate dehydrogenase 2 gene. Free Radic. Biol. Med. 2016;99:179–188. doi: 10.1016/j.freeradbiomed.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 33.Nam W.S., Park K.M., Park J.W. RNA interference targeting cytosolic NADP(+)-dependent isocitrate dehydrogenase exerts anti-obesity effect in vitro and in vivo. Biochim. Biophys. Acta. 2012;1822(8):1181–1188. doi: 10.1016/j.bbadis.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 34.Kim S., Kim S.Y., Ku H.J., Jeon Y.H., Lee H.W., Lee J., Kwon T.K., Park K.M., Park J.W. Suppression of tumorigenesis in mitochondrial NADP(+)-dependent isocitrate dehydrogenase knock-out mice. Biochim. Biophys. Acta. 2014;1842(2):135–143. doi: 10.1016/j.bbadis.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Noh M.R., Kim K.Y., Han S.J., Kim J.I., Kim H.Y., Park K.M. Methionine sulfoxide reductase A deficiency exacerbates cisplatin-induced nephrotoxicity via increased mitochondrial damage and renal cell death. Antioxidants Redox Signal. 2017;27(11):727–741. doi: 10.1089/ars.2016.6874. [DOI] [PubMed] [Google Scholar]
- 36.Noh M.R., Kim J.I., Han S.J., Lee T.J., Park K.M. C/EBP homologous protein (CHOP) gene deficiency attenuates renal ischemia/reperfusion injury in mice. Biochim. Biophys. Acta. 2015;1852(9):1895–1901. doi: 10.1016/j.bbadis.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Lee S.M., Koh H.J., Park D.C., Song B.J., Huh T.L., Park J.W. Cytosolic NADP(+)-dependent isocitrate dehydrogenase status modulates oxidative damage to cells. Free Radic. Biol. Med. 2002;32(11):1185–1196. doi: 10.1016/s0891-5849(02)00815-8. [DOI] [PubMed] [Google Scholar]
- 38.Kim J., Seok Y.M., Jung K.J., Park K.M. Reactive oxygen species/oxidative stress contributes to progression of kidney fibrosis following transient ischemic injury in mice. Am. J. Physiol. Ren. Physiol. 2009;297(2):F461–F470. doi: 10.1152/ajprenal.90735.2008. [DOI] [PubMed] [Google Scholar]
- 39.Cheng K.C., Cahill D.S., Kasai H., Nishimura S., Loeb L.A. 8-Hydroxyguanine, an abundant form of oxidative DNA damage, causes G----T and A----C substitutions. J. Biol. Chem. 1992;267(1):166–172. [PubMed] [Google Scholar]
- 40.Hsieh T.J., Zhang S.L., Filep J.G., Tang S.S., Ingelfinger J.R., Chan J.S. High glucose stimulates angiotensinogen gene expression via reactive oxygen species generation in rat kidney proximal tubular cells. Endocrinology. 2002;143(8):2975–2985. doi: 10.1210/endo.143.8.8931. [DOI] [PubMed] [Google Scholar]
- 41.Giani J.F., Bernstein K.E., Janjulia T., Han J., Toblli J.E., Shen X.Z., Rodriguez-Iturbe B., McDonough A.A., Gonzalez-Villalobos R.A. Salt sensitivity in response to renal injury requires renal angiotensin-converting enzyme. Hypertension. 2015;66(3):534–542. doi: 10.1161/HYPERTENSIONAHA.115.05320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kobori H., Harrison-Bernard L.M., Navar L.G. Urinary excretion of angiotensinogen reflects intrarenal angiotensinogen production. Kidney Int. 2002;61(2):579–585. doi: 10.1046/j.1523-1755.2002.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alhenc-Gelas F., Baussant T., Hubert C., Soubrier F., Corvol P. The angiotensin converting enzyme in the kidney. J. Hypertens. Suppl. 1989;7(7) doi: 10.1097/00004872-198909007-00003. S9-13;discussion S4. [DOI] [PubMed] [Google Scholar]
- 44.Nakamura T., Nakamura H., Hoshino T., Ueda S., Wada H., Yodoi J. Redox regulation of lung inflammation by thioredoxin. Antioxidants Redox Signal. 2005;7(1–2):60–71. doi: 10.1089/ars.2005.7.60. [DOI] [PubMed] [Google Scholar]
- 45.Kim H., Lee J.H., Park J.W. IDH2 deficiency exacerbates acetaminophen hepatotoxicity in mice via mitochondrial dysfunction-induced apoptosis. Biochim. Biophys. Acta (BBA) - Mol. Basis Dis. 2019;1865(9):2333–2341. doi: 10.1016/j.bbadis.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 46.Bellomo G., Martino A., Richelmi P., Moore G.A., Jewell S.A., Orrenius S. Pyridine-nucleotide oxidation, Ca2+ cycling and membrane damage during tert-butyl hydroperoxide metabolism by rat-liver mitochondria. Eur. J. Biochem. 1984;140(1):1–6. doi: 10.1111/j.1432-1033.1984.tb08058.x. [DOI] [PubMed] [Google Scholar]
- 47.Lee J.H., Go Y., Kim D.Y., Lee S.H., Kim O.H., Jeon Y.H., Kwon T.K., Bae J.H., Song D.K., Rhyu I.J., Lee I.K., Shong M., Oh B.C., Petucci C., Park J.W., Osborne T.F., Im S.S. Isocitrate dehydrogenase 2 protects mice from high-fat diet-induced metabolic stress by limiting oxidative damage to the mitochondria from brown adipose tissue. Exp. Mol. Med. 2020;52:238–252. doi: 10.1038/s12276-020-0379-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ogura Y., Kitada M., Monno I., Kanasaki K., Watanabe A., Koya D. Renal mitochondrial oxidative stress is enhanced by the reduction of Sirt3 activity, in Zucker diabetic fatty rats. Redox Rep. 2018;23(1):153–159. doi: 10.1080/13510002.2018.1487174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Someya S., Yu W., Hallows W.C., Xu J., Vann J.M., Leeuwenburgh C., Tanokura M., Denu J.M., Prolla T.A. Sirt3 mediates reduction of oxidative damage and prevention of age-related hearing loss under caloric restriction. Cell. 2010;143(5):802–812. doi: 10.1016/j.cell.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang X.X., Edelstein M.H., Gafter U., Qiu L., Luo Y., Dobrinskikh E., Lucia S., Adorini L., D'Agati V.D., Levi J., Rosenberg A., Kopp J.B., Gius D.R., Saleem M.A., Levi M., G Protein-coupled bile acid receptor TGR5 activation inhibits kidney disease in obesity and diabetes. J. Am. Soc. Nephrol. 2016;27(5):1362–1378. doi: 10.1681/ASN.2014121271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dikalov S.I., Nazarewicz R.R., Bikineyeva A., Hilenski L., Lassegue B., Griendling K.K., Harrison D.G., Dikalova A.E. Nox2-induced production of mitochondrial superoxide in angiotensin II-mediated endothelial oxidative stress and hypertension. Antioxidants Redox Signal. 2014;20(2):281–294. doi: 10.1089/ars.2012.4918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rodriguez-Iturbe B., Sepassi L., Quiroz Y., Ni Z., Wallace D.C., Vaziri N.D. Association of mitochondrial SOD deficiency with salt-sensitive hypertension and accelerated renal senescence. J. Appl. Physiol. 2007;102(1):255–260. doi: 10.1152/japplphysiol.00513.2006. [DOI] [PubMed] [Google Scholar]
- 53.Dai D.F., Johnson S.C., Villarin J.J., Chin M.T., Nieves-Cintron M., Chen T., Marcinek D.J., Dorn G.W., 2nd, Kang Y.J., Prolla T.A., Santana L.F., Rabinovitch P.S. Mitochondrial oxidative stress mediates angiotensin II-induced cardiac hypertrophy and Galphaq overexpression-induced heart failure. Circ. Res. 2011;108(7):837–846. doi: 10.1161/CIRCRESAHA.110.232306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang X.X., Wang D., Luo Y., Myakala K., Dobrinskikh E., Rosenberg A.Z., Levi J., Kopp J.B., Field A., Hill A., Lucia S., Qiu L., Jiang T., Peng Y., Orlicky D., Garcia G., Herman-Edelstein M., D'Agati V., Henriksen K., Adorini L., Pruzanski M., Xie C., Krausz K.W., Gonzalez F.J., Ranjit S., Dvornikov A., Gratton E., Levi M. FXR/TGR5 dual agonist prevents progression of nephropathy in diabetes and obesity. J. Am. Soc. Nephrol. 2018;29(1):118–137. doi: 10.1681/ASN.2017020222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liesa M., Shirihai O.S. Mitochondrial dynamics in the regulation of nutrient utilization and energy expenditure. Cell Metabol. 2013;17(4):491–506. doi: 10.1016/j.cmet.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dikalov S.I., Nazarewicz R.R. Angiotensin II-induced production of mitochondrial reactive oxygen species: potential mechanisms and relevance for cardiovascular disease. Antioxidants Redox Signal. 2013;19(10):1085–1094. doi: 10.1089/ars.2012.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Araujo M., Wilcox C.S. Oxidative stress in hypertension: role of the kidney. Antioxidants Redox Signal. 2014;20(1):74–101. doi: 10.1089/ars.2013.5259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kobori H., Nishiyama A. Effects of tempol on renal angiotensinogen production in Dahl salt-sensitive rats. Biochem. Biophys. Res. Commun. 2004;315(3):746–750. doi: 10.1016/j.bbrc.2004.01.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abdo S., Shi Y., Otoukesh A., Ghosh A., Lo C.S., Chenier I., Filep J.G., Ingelfinger J.R., Zhang S.L., Chan J.S. Catalase overexpression prevents nuclear factor erythroid 2-related factor 2 stimulation of renal angiotensinogen gene expression, hypertension, and kidney injury in diabetic mice. Diabetes. 2014;63(10):3483–3496. doi: 10.2337/db13-1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.