Abstract
A lady who underwent lensectomy for microspherophakia and pars plana vitrectomy for retinal detachment in her left eye developed recurrent filtering blebs at the site of sclerotomies. Filtering blebs were managed by suturing the sclerotomies. Targeted gene sequencing identified a variant of ASPH gene (p.Arg688Gln) which is not known to be associated with Traboulsi syndrome. But considering the paucity of cases with genetic analysis, it would be possible that p.Arg688Gln is a pathogenic variant. This is the first case report of Traboulsi syndrome due to an ASPH variant not reported earlier that can lead to recurrent filtering blebs.
Keywords: Microspherophakia, pars plana vitrectomy, Traboulsi syndrome, unintentional filtering blebs
Spontaneous filtering bleb and unintentional filtering blebs are rare clinical entities. Unintentional filtering blebs are reported to develop after cataract surgery.[1] Spontaneous filtering blebs are reported in Werner syndrome,[2,3] scleritis,[4] and Terrien's marginal degeneration.[5] It is also known to develop as a part of Traboulsi syndrome which includes ectopia lentis, spontaneous filtering blebs, and craniofacial dysmorphism.[6] In this article, we report a case of unilateral recurrent filtering bleb due to gaping of sclerotomies several years later in a lady operated for microspherophakia and retinal detachment (RD).
Case Report
A 33-year-old lady presented to us with complaints of small palpebral aperture in the left eye. Review of her past history revealed that she underwent lensectomy for microspherophakia 15 years ago. She underwent scleral buckling for RD in right eye 5 years ago. She underwent vitrectomy with circumferential explant 8 years ago (the details of surgery are not available) and epimacular membrane removal with sutureless 23G vitrectomy, 4 years ago in the left eye. Best corrected visual acuity (BCVA) was 20/20 (with spectacle correction of +12D) in the right eye and 20/60 (with spectacle correction of +14D) in the left eye. Intraocular pressure (IOP) was 18 mm of Hg in right eye and 2 mm of Hg in left eye. On examination, subconjunctival cysts were noted in the inferotemporal quadrant in the left eye. Seidel test was positive. It was adjacent to limbus extending from 4 to 6 o' clock [Fig. 1a]. There was no evidence of communication with the anterior chamber on anterior segment optical coherence tomography (ASOCT) [Fig. 1b and c]. There were choroidal folds with optic nerve head edema in the left eye due to hypotony. A diagnosis of unintentional filtering bleb was made. Surgical exploration of the bleb revealed a linear wound parallel to limbus at 5 o' clock position 3.5 mm from the limbus [Fig. 2a]. This would correspond to the site of inferotemporal sclerotomy. The wound was closed by a horizontal mattress suture (nylon). On first postoperative day, IOP was 32 mm of Hg. At 1 month, IOP was 14 mm of Hg. BCVA was 20/60. There was no evidence of bleb [Fig. 2b]. 6 months later, IOP was 2 mm of Hg. A filtering bleb was seen in the superotemporal quadrant adjacent to limbus from 1 to 3 o' clock [Fig. 3a]. The Seidel test was negative. ASOCT through the bleb did not identify any breech in sclera [Fig. 3b and c]. Brilliant blue G dye was injected into the vitreous cavity and the superotemporal bleb was explored. A linear area of staining was noted at 3 o' clock [Fig. 4a]. There was no definite gape, but on pressure minimal ooze of fluid could be detected. The linear thinning was closed by mattress suture and autologous partial thickness scleral patch graft. Areas of thinning was noted in superonasal quadrant, but there was no evidence of leak [Fig. 4b]. Eight months later, a filtering bleb was seen in the superonasal quadrant from 10 to 12 o' clock. But IOP was 12 mm of Hg. Considering the occurrence of unintentional recurrent filtering blebs, microspherophakia, and flat cheek [Fig. 4c], targeted gene sequencing was performed to identify ASPH gene mutation which is implicated in Traboulsi syndrome. Analysis of pedigree chart showed that her parents were second cousins [Fig. 4d]. A homozygous missense variation in exon 24 of the ASPH gene that results in the amino acid substitution of glutamine for arginine at codon 688 was detected (p. Arg688Gln). Though an ASPH gene mutation was found, this variant is not reported to be responsible for Traboulsi syndrome in the literature so far. Validation of the variant by sequencing the variant in the parents and other family members was planned. But the patient denied further investigations, as other family members were not affected by the disorder.
Figure 1.
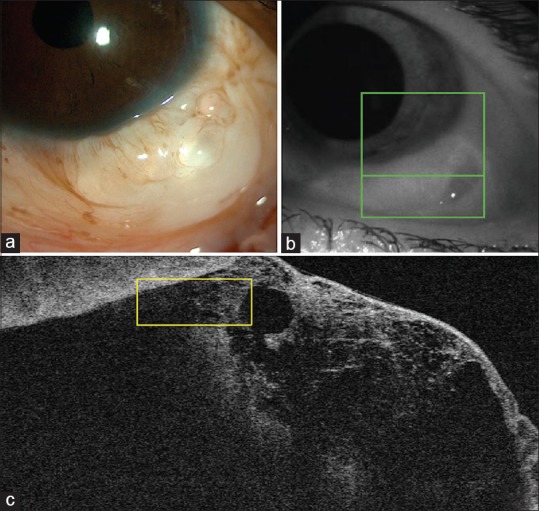
(a): Slit-lamp photograph of the left eye showing cystic bleb in the inferotemporal quadrant. (b): Demonstration of the level of cross-section of optical coherence tomography. (c): Anterior segment optical coherence tomography through the bleb showing subconjunctival cystic areas
Figure 2.
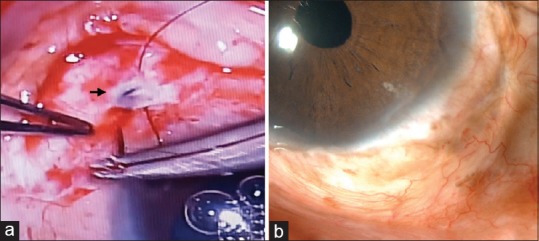
(a): Linear gape in the sclera (arrow) in the inferotemporal quadrant parallel to the limbus corresponding to sclerotomy. (b): Postoperative slit-lamp photograph showing conjunctival scarring
Figure 3.
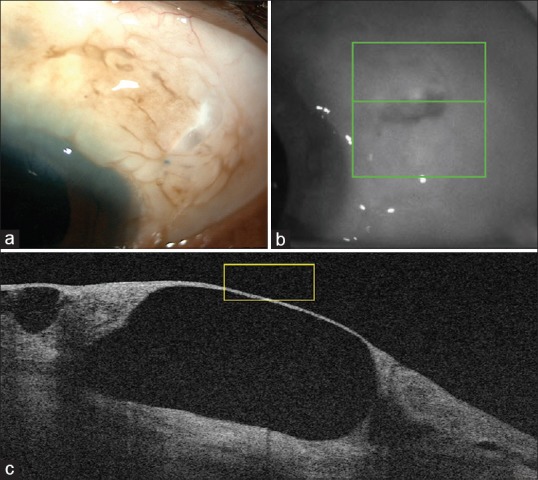
(a): Slit-lamp photograph of the left eye showing cystic bleb in the superotemporal quadrant. (b): Demonstration of the level of cross-section of optical coherence tomography. (c): Anterior segment optical coherence tomography through the bleb showing thin walled cyst
Figure 4.
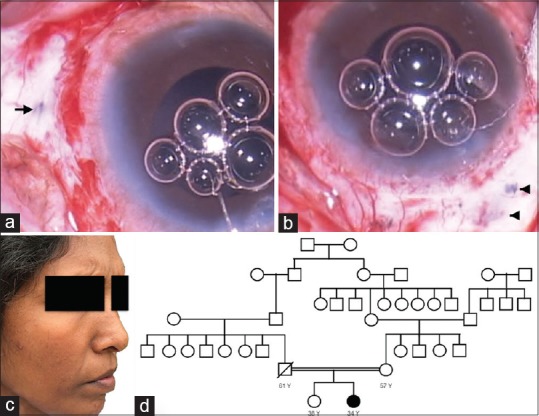
(a): Linear area of thinning in the sclera (arrow) at 3 o' clock parallel to the limbus corresponding to sclerotomy. (b): Area of scleral thinning in the superonasal quadrant (arrow head). (c): Face photograph showing flat cheek. (d): Analysis of pedigree chart shows common ancestral origin of subject's parents. Pedigree chart is incomplete as she could not recollect beyond her grandparents
Discussion
Spontaneous filtering blebs are reported as a part of Traboulsi syndrome. The syndrome is characterized by the presence of dislocated crystalline lens and distinctive facial features involving beaked nose and flat cheeks. Spontaneous conjunctival filtering blebs with hypotony is seen in a few affected individuals probably due to scleral thinning.[7,8] The syndrome is caused by homozygous or compound heterozygous mutation in the ASPH gene on chromosome 8q12.[9] ASPH encodes an enzyme which hydroxylate asparagine and aspartic acid on epidermal growth factor domain containing proteins.[8]
Our patient underwent lensectomy for microspherophakia. Unintentional filtering blebs are not reported after vitrectomy. The filtering bleb developed due to leak of fluid from vitreous through a linear well-constructed wound in inferotemporal quadrant corresponding to sclerotomy site. After successful closure of the inferotemporal fistulous tract, the bleb developed in superotemporal quadrant and then in the superonasal quadrant. The area of leak in the superotemporal quadrant was also similar to a sclerotomy wound. It is unlikely that a sclerotomy would gape after 4 years of surgery. But it would be possible that a condition which would predispose to spontaneous filtering bleb would co-exist in our case. The co-existent condition could have led to gaping of sclerotomy which is a compromised site in the sclera. Our patient had flat cheeks which is described in cases with Traboulsi syndrome. But there was no evidence of beaked nose. Targeted gene sequencing identified a variant of ASPH gene (p. Arg688Gln) which is not known to be associated with Traboulsi syndrome. p. Arg735Trp is described as a pathogenic variant in literature.[8] But considering the paucity of cases with genetic analysis, it would be possible that p. Arg688Gln is a pathogenic variant. The right eye did not develop filtering blebs. Scleral buckling was done in the right eye in contrast to pars plana vitrectomy in the left eye. Though spontaneous blebs are known to develop in Traboulsi syndrome without any insults, avoiding sclerotomies would prevent development of filtering blebs to some extent. Scleral thickness was not measured in our case, but definite scleral thinning was not noted in other areas. So partial thickness scleral autograft was used. But it would have been avoided considering that the eye is predisposed to recurrent blebs.
Recurrent unintentional filtering blebs following vitrectomy is not reported in the literature so far. This is the first case report of Traboulsi syndrome due to an ASPH variant not reported earlier that can lead to filtering blebs due to gaping of sclerotomies several years after vitrectomy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Swan KC, Campbell WL. Unintentional filtration following cataract surgery. Arch Ophthalmol. 1964;71:43–9. doi: 10.1001/archopht.1964.00970010059007. [DOI] [PubMed] [Google Scholar]
- 2.Moghimi S, Soleimani M, Soltani R. UBM study in spontaneous bleb formation and blebitis after cataract surgery in Werner syndrome. Eye (Lond) 2009;23:1481–3. doi: 10.1038/eye.2009.61. [DOI] [PubMed] [Google Scholar]
- 3.Jonas JB, Ruprecht KW, Schmitz-Valckenberg P, Brambring D, Platt D, Gebhart E, et al. Ophthalmic surgical complications in Werner's syndrome: Report on 18 eyes of nine patients. Ophthalmic Surg. 1987;18:760–4. [PubMed] [Google Scholar]
- 4.Mantravadi AV, Stock EL. Spontaneous filtration bleb as a consequence of scleritis. Arch Ophthalmol. 2007;125:1578–9. doi: 10.1001/archopht.125.11.1578. [DOI] [PubMed] [Google Scholar]
- 5.Munro M, McWhae J, Romanchuk K, Crichton A, Carter G, Ball A, et al. Two cases of spontaneous filtering blebs, one idiopathic and one associated with Terrien marginal degeneration. Cornea. 2014;33:752–4. doi: 10.1097/ICO.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 6.Mansour AM, Younis MH, Dakroub RH. Anterior segment imaging and treatment of a case with syndrome of ectopia lentis, spontaneous filtering blebs, and craniofacial dysmorphism. Case Rep Ophthalmol. 2013;4:84–90. doi: 10.1159/000350951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shawaf S, Noureddin B, Khouri A, Traboulsi EI. A family with a syndrome of ectopia lentis, spontaneous filtering blebs, and craniofacial dysmorphism. Ophthal Genet. 1995;16:163–9. doi: 10.3109/13816819509057858. [DOI] [PubMed] [Google Scholar]
- 8.Patel N, Khan AO, Mansour A, Mohamed JY, Al-Assiri A, Haddad R, et al. Mutations in ASPH cause facial dysmorphism, lens dislocation, anterior-segment abnormalities, and spontaneous filtering blebs, or Traboulsi syndrome. Am J Hum Genet. 2014;94:755–9. doi: 10.1016/j.ajhg.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haddad R, Uwaydat S, Dakroub R, Traboulsi EI. Confirmation of the autosomal recessive syndrome of ectopia lentis and distinctive craniofacial appearance. Am J Med Genet. 2001;99:185–9. doi: 10.1002/1096-8628(2001)9999:9999<::aid-ajmg1156>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]


