Since the first identification in December 2019 in Wuhan, China, a number of cases of novel coronavirus (2019-nCoV)-infected patients is increasing around the world. It has been reported that there are high-risk populations with high mortality, such as elderly people and those with comorbidities [1]. However, no specific treatment has been developed yet. Historically, humans have overcome the pandemics of viral infection by preventing secondary infection. Several studies have simulated the spread of 2019-nCoV, and the basic reproduction number (R0) ranges from 2.2 to 3.6 [2, 3]. On the other hand, patients treated with disease-modifying antirheumatic drugs may have insufficient antibody response, implying the possibility of reinfection [4].
Here, to simulate the efficacy of preventing secondary infection in population with consideration of reinfection, I simulated a scenario of one person with 2019-CoV infection entering into a population of 1000 people with the hypothesis that a part of them lose immunity. I used the SIRS model which is composed of different categories within a population; the susceptible (S), infected (I), recovered (R), and returned-susceptible (S) compartments, respectively. The model can be written as the following ordinary differential equation:
where S, I, and R are proportions of susceptible, infected, and recovered individuals, respectively, β is the transmission rate of infection, γ is recovery rate (inverse of the infectious period), and ξ is returning rate of recovered individuals to the susceptible statue due to loss of immunity. N (= S + I + R) is the total population. The simulation was started with S = 999, I = 1, and R = 0 for the following 100 days after the entry of one person with 2019-nCoV. Considering the uncertainty of parameters in the real-world outside China, I combined parameters based on considerable circumstances. Analyses were performed by R software.
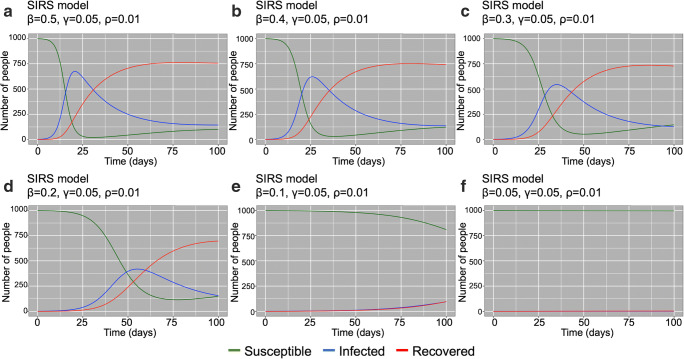
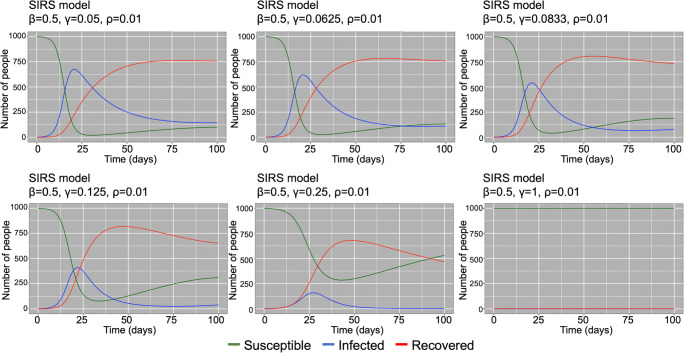
First, parameters were set as (β, γ, ξ) = (0.5, 1/20, 0.01) based on assumption that infectious duration is 20 days [5] and 1% of recovered individuals return to the susceptible statue due to loss of immunity. As β decreased 0.5, 0.4, 0.3, 0.1, and 0.05 (Fig. 1 a, b, c, d, e, and f, respectively), the maximum number of infected people decreased and the peak delayed, suggesting the effectivity of decreasing transmission rate by standard precautions. When β was 0.05, the secondary infection did not occur. R0 in each situation was 10, 8, 6, 4, 2, and 1, respectively. Next, to evaluate the efficacy of prompt isolation of infected patients, γ was stratified with 1/20, 1/16, 1/12, 1/8, 1/4, and 1/1 with keeping βN and ξ the same. As a result, the maximum number of infected people decreased as γ increased (Fig. 2 a, b, c, d, e, and f, respectively). The secondary infection did not occur in the case of γ = 1/1. R0 in each situation was 10, 8, 6, 4, 2, and 1, respectively. These trends were the same as the case ξ = 0 (Supplementary Figs. 1 and 2; when 2019-nCoV infection would lead to long-lasting immunity).
Figure 1.
SIRS model for assessing impact of transmission rate (β). Transmission rate were stratified with 0.5 (a), 0.4 (b), 0.3 (c), 0.2 (d), 0.1 (e), and 0.05 (f) with keeping recovery rate (γ) and returning rate (ξ) as 1/20 and 0.01, respectively
Fig. 2.
SIRS model for assessing impact of recovery rate (γ). Recovery rates were stratified with 1/20 (a), 1/16 (b), 1/12 (c), 1/8 (d), 1/4 (e), and 1/1 (f) with keeping transmission rate (β) and returning rate (ξ) as 0.5 and 0.01, respectively
This study suffers from several limitations. First, since the clinical characteristics of 2019-nCoV are largely unknown, the value of parameters used in this simulation may not be proper. Second, the SIRS model is a simple model based on some assumptions; the population is closed (no vital dynamics such as birth and death) and the course of the infection is short (emergent outbreak). Also, the possibility that asymptomatic patients could be infectious to others is not considered in this model [6]. Third, because the SIR model assumes a homogeneous infection network between individuals, the heterogeneity of individuals such as disease status was not considered. Forth, other than standard precautions, β is also affected by virologic characteristics and factors of hosts. Therefore, the result of this study cannot apply to data in the real-world directly. However, this study demonstrated that outbreaks can be prevented by performing appropriate precautionary measures even in populations with consideration of the possibility of reinfection.
Electronic supplementary material
SIR model for assessing impact of transmission rate (β). Transmission rate were 0.5 (A), 0.4 (B), 0.3 (C), 0.2 (D), 0.1 (E) and 0.05 (F). Recovery rate (γ) and returning rate (ξ) were set as 1/20 and 0, respectively. (PNG 7014 kb)
SIR model for assessing impact of recovery rate (γ). Recovery rate were 1/20 (A), 1/16 (B), 1/12 (C), 1/8 (D), 1/4 (E) and 1/1 (F). Transmission rate (β) and returning rate (ξ) were set as 0.5 and 0, respectively. (PNG 2062 kb)
Author’s contributions
Conceptualization, formal analysis, and writing were conducted by the author.
Data availability
All custom computer codes in the generation or processing of the described data are available in the supplementary file.
Compliance with ethical standards
Ethics approval and consent to participate
Ethical approval or individual consent was not applicable.
Consent for publication
Not applicable.
Disclosures
None.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W, Lou Y, Gao D, Yang L, He D, Wang MH. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214–217. doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hesselstrand R, Nagel J, Saxne T, Geborek P, Skattum L, Kapetanovic MC. Immunogenicity and safety of pneumococcal vaccination in patients with systemic sclerosis. Rheumatology (Oxford) 2018;57:625–630. doi: 10.1093/rheumatology/kex471. [DOI] [PubMed] [Google Scholar]
- 5.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, Yu J, Kang M, Song Y, Xia J, Guo Q, Song T, He J, Yen HL, Peiris M, Wu J. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W, Seilmaier M, Drosten C, Vollmar P, Zwirglmaier K, Zange S, Wölfel R, Hoelscher M. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SIR model for assessing impact of transmission rate (β). Transmission rate were 0.5 (A), 0.4 (B), 0.3 (C), 0.2 (D), 0.1 (E) and 0.05 (F). Recovery rate (γ) and returning rate (ξ) were set as 1/20 and 0, respectively. (PNG 7014 kb)
SIR model for assessing impact of recovery rate (γ). Recovery rate were 1/20 (A), 1/16 (B), 1/12 (C), 1/8 (D), 1/4 (E) and 1/1 (F). Transmission rate (β) and returning rate (ξ) were set as 0.5 and 0, respectively. (PNG 2062 kb)
Data Availability Statement
All custom computer codes in the generation or processing of the described data are available in the supplementary file.