The present emergency caused by the spread of the Covid-19 infection is putting enormous pressure on the healthcare systems worldwide and especially on intensive care units (ICUs).
One of the main fears in this regard is that we may run out of ventilators, a possibility which is getting more and more likely as the pandemic spreads throughout the world and the ICUs are overloaded with ventilated patients.
Many authors have already investigated the possibility of manipulating a ventilator circuit in order to ventilate up to four patients with a single machine. Neyman and Ervin first performed a bench study demonstrating the technical feasibility of ventilating four patients with one ventilator and one modified circuit.1 The same circuit configuration was used in 2008 by Paladino et al in an animal model, resulting in substantial differences in oxygenation and decarboxylation between subjects during the ventilation period.2 In 2012 Branson et al tested in vitro the Neyman and Ervin system simulating different conditions of compliance and resistance between the simultaneously ventilated test lungs. They observed wide variability in measured tidal volume (Vt) and end-expiratory lung volume, so they concluded that the technique should be avoided because of potential danger.3 Accordingly, the authors argued that the stockpiling of ventilators should be the first-line solution when massive emergencies are forecast; only after their depletion, strategies such as the ‘double circuit’ should be implemented for the shortest possible duration.4 5
On 20 February 2020, the first case of Covid-19 emerged in the Lombardy region, northern Italy. As of 17 March, a total of 1069 patients had been admitted to ICUs in Lombardy, with a total of 1202 ICU beds available (after a significant expansion from the 720 beds available pre-crisis).6 By this time, a potential problem of ventilator shortages began to emerge because of the further spread of the virus in other regions of Italy. Great efforts have been put into place by institutions and industries to provide more ventilators for hospitals, but there is still a high potential for a supply–demand mismatch.
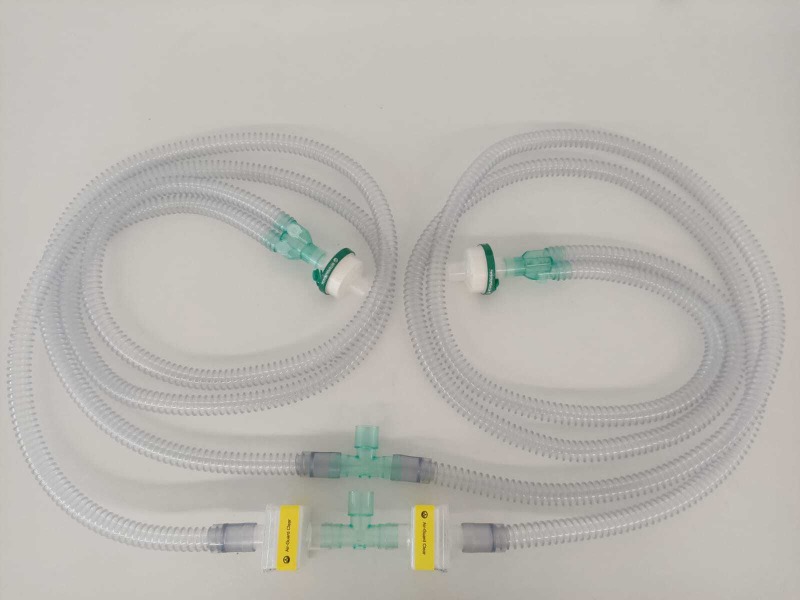
Therefore, we assembled, tested and proposed for production a simple circuit comprising tubing and accessories that are easily available in any intensive care/operating room setting. Indeed, one just needs two regular ‘wye’ breathing circuits, two ‘T’ connectors, and four heat and moisture exchanger (HME) filters to build this system (see figure 1 online supplementary file 1, online supplementary file 2).
thoraxjnl-2020-214895supp001.pdf (134.4KB, pdf)
thoraxjnl-2020-214895supp002.mp4 (55.2MB, mp4)
Figure 1.
Assembled circuit.
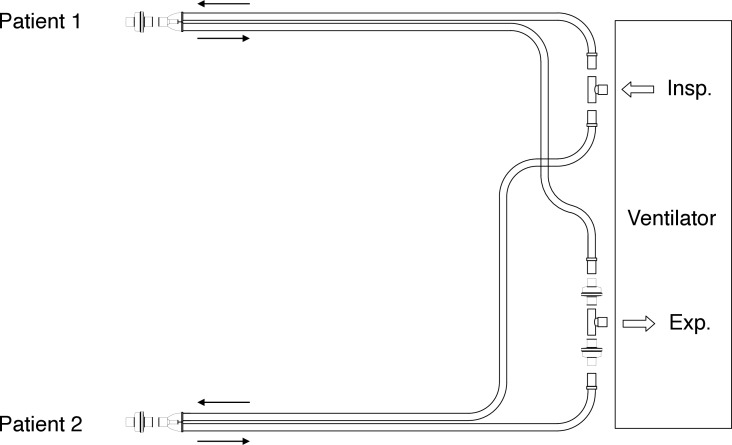
The two T pieces are connected to the inspiratory and expiratory ports of the ventilator (figure 2). We preferred to interpose one HME filter in each expiratory limb (and not one for the entire expiratory circuit) in order to reduce total circuit resistance. At the end of each wye a patient is connected by interposing one HME filter. Total length of the tubing is 9.6 m, and each patient can be located at ~2 m from the ventilator.
Figure 2.
Circuit set-up. Arrows pointing left indicate inspiratory airflow, arrows pointing right indicate expiratory airflow. Insp., inspiratory port; Exp., expiratory port.
We tested the circuit on a turbine ventilator (SIARETRON 4000 T, Siare Engineering International Group, Crespellano-Valsamoggia, Italy) connected by a two-patient circuit (Intersurgical SpA, Mirandola, Italy) to two test lungs (Model 5601 - Michigan Instruments Inc, Grand Rapids, MI, USA). We set ventilation for two patients of 80 kg of predicted body weight (PBW) targeting 6 mL/kg Vt at a respiratory rate (RR) of 20/min with an inspiratory: expiratory (I:E) ratio of 1:1 and a fraction of inspired oxygen (FiO2) of 100%. Positive end-expiratory pressure (PEEP) was set at 15 cmH2O and initial inspiratory pressure (Pinsp) at 10 cmH2O. We performed an initial 15 hour test with similar conditions between the two simulated patients (static compliance of the respiratory system (Cstat) 50 mL/cmH2O and airway resistance (Raw) 5 cmH2O/L/sec); in pressure control mode (Pinsp 11 cmH2O, PEEP 14 cmH2O, RR 20 beats/min), measured delivered Vt was 953 mL, while the patients received 470 mL each.
We then performed two more tests:
Different Cstat (40 mL/cmH2O vs 60 mL/cmH2O) and equal Raw (5 cmH2O/L/sec): as expected, Vt distribution was proportional to Cstat—540 mL for the simulated patient with Cstat 60 mL/cmH2O and 340 mL for the one with Cstat 40 mL/cmH2O
Different Raw (5 cmH2O/L/sec vs 20 cmH2O/L/sec) and equal Cstat (50 mL/cmH2O): as expected, Vt distribution correlated with Raw—480 mL for Raw 5 cmH2O/L/sec and 400 mL for Raw 20 cmH2O/L/sec.
Our tests confirm the in vitro technical feasibility of ventilating two patients with a single ventilator, but the difficulties and potential harm due to this configuration remain. Considering present knowledge on this issue and our data, we suggest a flow chart (table 1) to initiate this type of ventilation only in cases of extreme emergency due to machinery shortages. A critical point is to match patients by compliance and, possibly, by airways resistance. Clinical personnel must remain vigilant, in order to recognise any possible sign of hypo- or overventilation, and must be ready at any time to start manual bag ventilation if any issue would occur.
Table 1.
Connecting two patients to one ventilator.
| Prerequisites: |
|
| Settings: |
|
| Starting procedures: |
|
| Monitoring and alarms: |
|
| Provide another ventilator as soon as possible | |
ABG, arterial blood gas test; ET, endotracheal tube; EtCO2, end-tidal carbon dioxide; FiO2, fraction of inspired oxygen ; PBW, predicted body weight; PCV, pressure-controlled ventilation; PEEP, positive end-expiratory pressure; SpO2, peripheral capillary oxygen saturation; Vt, tidal volume.
Compared with manual bag ventilation, our technique allows delivery of ventilation, PEEP and FiO2 with reasonable accuracy, is safer for operators and avoids the need for additional human resources (no ‘human ventilator’ is constantly needed at the patient’s head). Using one ventilator for two patients instead of four (as proposed by some authors) reduces possible logistical issues (bed and ventilator positioning) and problems related to inadequate patient size matching.
We can conclude that this simple and easily built circuit can theoretically allow the emergency ventilation of two patients with a single ventilator. However, for a clinical application of this ‘extreme’ technique, several other factors must be taken into account. Indeed, anthropometric features (body weight and body mass index), respiratory mechanics (lung and chestwall compliances, airway resistances, possible auto-PEEP), physiological variables (complete paralysis, oxygen consumption and carbon dioxide production) and the clinical course of the two connected patients play a major role in determining the quality and quantity of ventilation delivered to each patient. Moreover, monitoring respiratory mechanics in each patient would be impossible or very difficult; however, we cannot neglect the possibility that, besides technical and physiological factors, ethical dilemmas may also arise.7 Indeed, the most difficult choice during such an emergency would be to either accept a grim triage reality (in which not all patients receive a ventilator) or accept the fact that trying to save two patients with one ventilator could mean harming at least one of them.
To the best of our knowledge, no significant evidence is available to date on this topic, but very recently New York-Presbyterian Hospital in the USA published a clinical guideline on this topic.8 To add to the controversy, however, a very recent consensus statement by several North American scientific societies discourages clinicians from connecting more than one patient to a single ventilator.7
Footnotes
TT, AZ and GP contributed equally.
Contributors: All authors contributed in designing and writing the paper and in testing the equipment. All authors read and approved the final version of this manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Neyman G, Irvin CB. A single ventilator for multiple simulated patients to meet disaster surge. Acad Emerg Med 2006;13:1246–9. 10.1197/j.aem.2006.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Paladino L, Silverberg M, Charchaflieh JG, et al. Increasing ventilator surge capacity in disasters: ventilation of four adult-human-sized sheep on a single ventilator with a modified circuit. Resuscitation 2008;77:121–6. 10.1016/j.resuscitation.2007.10.016 [DOI] [PubMed] [Google Scholar]
- 3. Branson RD, Blakeman TC, Robinson BR, et al. Use of a single ventilator to support 4 patients: laboratory evaluation of a limited concept. Respir Care 2012;57:399–403. 10.4187/respcare.01236 [DOI] [PubMed] [Google Scholar]
- 4. Branson RD, Rubinson L. A single ventilator for multiple simulated patients to meet disaster surge. Acad Emerg Med 2006;13:1352–3. 10.1197/j.aem.2006.10.002 [DOI] [PubMed] [Google Scholar]
- 5. Branson RD, Rubinson L. One ventilator multiple patients--what the data really supports. Resuscitation 2008;79:171–2. 10.1016/j.resuscitation.2008.04.033 [DOI] [PubMed] [Google Scholar]
- 6. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020. doi: 10.1001/jama.2020.4031. [Epub ahead of print: 13 Mar 2020]. [DOI] [PubMed] [Google Scholar]
- 7. Consensus Statement on Multiple Patients Per Ventilator [Internet] Available: https://www.sccm.org/Disaster/Joint-Statement-on-Multiple-Patients-Per-Ventilato [Accessed 7 Mar 2020].
- 8. Beitler JR, Kallet R, Kacmarek R, et al. Columbia University Vagelos College of Physicians & Surgeons – New York-Presbiterian Hospital - ventilator sharing protocol: dual-patient ventilation with a single mechanical ventilator for use during critical ventilator shortages – version 4, March 27 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2020-214895supp001.pdf (134.4KB, pdf)
thoraxjnl-2020-214895supp002.mp4 (55.2MB, mp4)