Abstract
Introduction
The SARS-CoV-2 pandemic has hit the European region disproportionately. Many HIV clinics share staff and logistics with infectious disease facilities, which are now on the frontline in tackling COVID-19. Therefore, this study investigated the impact of the current pandemic situation on HIV care and continuity of antiretroviral treatment (ART) supplies in CEE countries.
Methods
The Euroguidelines in Central and Eastern Europe (ECEE) Network Group was established in February 2016 to review standards of care for HIV in the region. The group consists of professionals actively involved in HIV care. On March 19, 2020 we decided to review the status of HIV care sustainability in the face of the emerging SARS-CoV-2 pandemic in Europe. For this purpose, we constructed an online survey consisting of 23 questions. Respondents were recruited from ECEE members in 22 countries, based on their involvement in HIV care, and contacted via email.
Results
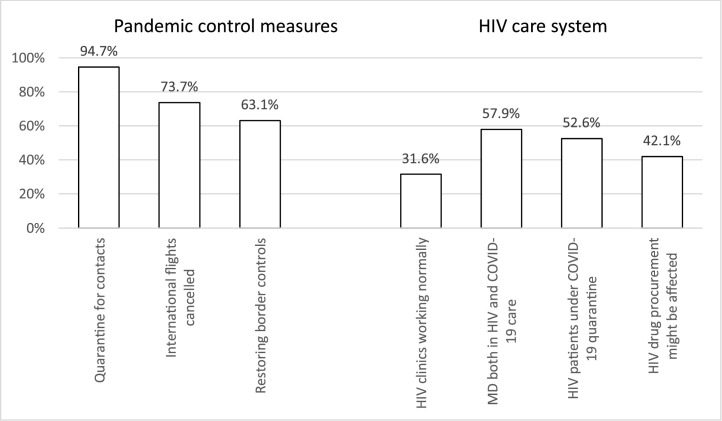
In total, 19 countries responded: Albania, Armenia, Belarus, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Estonia, Georgia, Greece, Hungary, Lithuania, Macedonia, Poland, Republic of Moldova, Russia, Serbia, Turkey, and Ukraine. Most of the respondents were infectious disease physicians directly involved in HIV care (17/19). No country reported HIV clinic closures. HIV clinics were operating normally in only six countries (31.6%). In 11 countries (57.9%) physicians were sharing HIV and COVID-19 care duties. None of the countries expected shortage of ART in the following 2 weeks; however, five physicians expressed uncertainty about the following 2 months. At the time of providing responses, ten countries (52.6%) had HIV-positive persons under quarantine.
Conclusions
A shortage of resources is evident, with an impact on HIV care inevitable. We need to prepare to operate with minimal medical resources, with the aim of securing constant supplies of ART. Non-governmental organizations should re-evaluate their earlier objectives and support efforts to ensure continuity of ART delivery.
Keywords: HIV, SARS-CoV-2, COVID-19, ARV
Introduction
The SARS-CoV-2 pandemic has hit the European region disproportionately, with over half a million people being infected with the virus within 4 weeks, of whom more than 40 000 died (European Centre for Disease Prevention and Control, 2020). At the time of writing this represented half of all confirmed cases worldwide and two thirds of deaths. There is increasing concern that low- and middle-income countries are not testing for SARS-CoV-2; therefore, the number of cases remains strongly under-reported for some Central and Eastern European (CEE) countries. It is in these areas where the uncontrolled coronavirus pandemic meets fragile or basic healthcare systems.
Many HIV clinics share staff and logistics with infectious disease facilities, which are now on the frontline in tackling COVID-19. Therefore, this study investigated the impact of the current SARS-CoV-2 pandemic situation on HIV care and continuity of antiretroviral treatment (ART) supplies in CEE countries.
Methods
The Euroguidelines in Central and Eastern Europe (ECEE) Network Group was established in February 2016 to review standards of care for HIV in the region. The group consists of experts in the HIV field as well as professionals actively involved in HIV patient care. In addition to yearly meetings held in Warsaw, the group acts through online surveys, applying the same method each time (Kowalska et al., 2017). On March 19 we decided to review the status of HIV care sustainability in the face of the emerging COVID-19 pandemic in Europe. For this purpose, we constructed an online survey consisting of 23 questions. Most included predefined multiple-choice answers plus an additional 'other' answer allowing for a free text input. Respondents were recruited from the ECEE members in 22 countries (one per country), based on their involvement in HIV care, and contacted via email.
Results
In total, 19 countries responded: Albania, Armenia, Belarus, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Estonia, Georgia, Greece, Hungary, Lithuania, Macedonia, Poland, Republic of Moldova, Russia, Serbia, Turkey, and Ukraine. Most of the respondents were infectious disease physicians directly involved in HIV care (17/19).
Substantial pandemic control measures were being used in the majority of the countries. These included: restoration of trans-border traffic controls (12/19); cancellation of international flights (with planned citizen evacuations in 14/19 and no planned citizen evacuations in 4/19); no entry for non-citizens (13/19); quarantines (for people from suspected contacts in 18/19, for all returning from abroad in 16/19, and for those returning from selected countries in 3/19); home-based work preference (17/19); or temporary suspension from work duties (9/19).
No country reported the closure of HIV clinics. HIV clinics were operating normally in six countries (31.6%). In three countries there were either shorter hours or reduced staff, while in ten (52.6%) normal activity (regular visits and blood tests) was suspended, and only ART distribution was continued. In 11 countries (57.9%) physicians were sharing HIV care and COVID-19 care duties (Figure 1 ).
Figure 1.
Main findings on measures to control the SARS-CoV-2 pandemic and HIV care services in 19 countries.
In most countries ART was dispensed for 2–3 months (13/19), in five for 4–6 months, and in one for a month. None of the countries expected shortages of ART over the following 2 weeks; however, five physicians expressed uncertainty about the following 2 months. In eight countries respondents were of the opinion that procurement might be endangered. One person expressed concern relating to possible lopinavir/ritonavir stock-outs, related to its wider use for COVID-19 patients. Three respondents expressed uncertainty relating to the economic situation after the pandemic, which could affect governments’ ability to continue ART procurement.
In eight countries respondents indicated that HIV clinics were contacted by HIV-positive person(s) who were not under their care, but unable to return to their place of residence due to SARS-CoV-2 pandemic-related restrictions. In all cases HIV-positive persons were provided with ART free of charge.
At the time of providing responses, ten countries (52.6%) had HIV-positive persons under SARS-CoV-2-related quarantine.
Discussion
In our survey almost 60% of responding countries reported that HIV physicians were at the same time directly involved in work related to COVID-19 patients. Infectious disease physicians, who take care of HIV-positive patients, are likely to be fully occupied with the current SARS-CoV-2 situation. This area of medical specialty has, for many years, been underfinanced and underpowered in CEE countries and is not easily replaced. In addition, medical staff will most likely face exhaustion, trauma, and other negative psychological effects (Kang et al., 2020).
In our study only around 30% of the countries continued to have HIV clinics working normally. Healthcare systems in Europe have been hit hard by the high number of COVID-19 cases and the severity of the disease (Saglietto et al., 2020). As a result, both acute and chronic medical conditions unrelated to COVID-19 have been down prioritized, which is especially difficult when patients are dependent on their clinics in terms of continuity of drug supply. The COVID-19 pandemic poses a threat to the continuum of HIV care at any given stage (Jiang et al., 2020). Half of the countries in the CEE reported SARS-CoV-2 quarantines applying also to HIV-positive persons, and in eight countries ART was provided for people whose travel back to their place of residency had been restricted. A survey performed in February 2020, during the SARS-CoV-2 outbreak in China, showed that one in three HIV-positive persons was not carrying enough ART to cover them for special travelling restrictions, and two out of three in Hubei province reported difficulty in obtaining ART (Guo et al., 2020).
In addition, remaining in isolation and social distancing measures may fuel negative psychological effects. In the CEE region many HIV-positive people come from vulnerable populations and already experience stigmatization and loneliness (Balayan et al., 2019). Taking lessons from previous epidemics, we should acknowledge that in people exposed to a stressful event during a pandemic, depression is highly likely to occur (Liu et al., 2012). All these factors may affect adherence to, and retention in, care. At the same time, patients with advanced or uncontrollable HIV infection may be more vulnerable to COVID-19 disease, with half of them having comorbidities that increase COVID-19 severity (Anon, 2020a).
In most CEE countries HIV care is organized in such a way that ART is bought centrally and distributed through designated clinics (Gokengin et al., 2018). Moreover, ART procurement varies by country and relies on complicated administrative procedures, because many ART components are not produced locally. According to our data most countries dispensed ART for 2–3 months, with some respondents expressing uncertainty about the sustainability of supplies. Almost half of our respondents indicated that procurement processes might be further impacted due to the current pandemic. It seems inevitable that international organizations need to collaborate with governments in CEE countries in order to provide additional financial and logistic support in this area (Anon, 2020b).
There are some important limitations in relation to this work that need to be mentioned. As this was a survey study, with each country represented by a single person, the answers could be subjective and express the opinion of the respondent. However, each country was represented by a nationally recognized expert in the field, who was also actively involved in HIV patient care (Kowalska et al., 2017). Therefore, we believe that the responses accurately reflect the situation in a given country, and thus provide a reliable sample. The group has reviewed many aspects of standards of HIV care in the past using the same method (Kowalska et al., 2018). Finally, survey studies are conducted in order to gather large amounts of information in a short period of time; however, they carry certain bias and should be interpreted with caution. As the SARS-CoV-2 pandemic continues we need to prepare for operating with minimal medical resources in order to secure retention of ART. Non-governmental organizations (NGOs) should re-evaluate their earlier objectives and support medical efforts to retain continuity of ART deliverance. For example, where personal ART pick-up is not possible it could be organized by home delivery or distributed through existing peer-to-peer contacts. For that reason, those funding NGOs need to show flexibility in restructuring already sponsored programs. The shortage of resources is evident and the impact on HIV care inevitable.
Conflicts of interest
The authors declare no conflicts of interest and this project did not receive any funding. According to local law, there was no requirement to obtain bioethical committee approval for this study.
Acknowledgments
ECEE Network Group: Afonina L (Russia), Alexiev I (Bulgaria), Antonyak S (Ukraine), Antonyak S (Ukraine), Balayan T (Armenia), Bednarska A (Poland), Begovac J (Croatia), Bolokhadze N (Georgia), Bukovinowa P (Slovakia), Burkacka E (Poland), Bursa D (Poland), Caplinskas S (Lithuania), Chkhartishvili N (Georgia), Dragovic G (Serbia), Goekengin D (Turkey), Harxhi A (Albania), Higersberger J (Poland), Holban T (Moldova), Horban A (Poland), Jevtovic D (Serbia), Jilich D (Czech Republic), Karpov I (Belarus), Kase K (Estonia), Kowalska JD (Poland), Krasniqi V (Kosovo), Ladnaya N (Russia), Lakatos B (Hungary), Marczyńska M (Poland), Mardarescu M (Romania), Matłosz B (Poland), Matulyte E (Lithuania), Matulionyte R (Lithuania), Mulabdic V (Bosnia-Herzegovina), Oprea C (Romania), Otelea D (Romania), Paciorek M (Poland), Panteleyev A (Russia), Papadopoulos A (Greece), Podlasin B (Poland), Podlekareva D (Denmark), Rukhadze (Georgia), Ruutel K (Estonia), Sedlacek D (Czech Republic), Simonovic Babic J (Serbia), Skrzat-Klapaczynska A (Poland), Sluzhynska M (Ukraine), Stańczak J (Poland), Stevanovic M (Macedonia), Strashimirov D (Bulgaria), Streinu-Cercel A (Romania), Tetradov S (Romania),Tomazic J (Slovenia), Turcanu O (Rep. of Moldova), Vassilenko A (Belarusia), Vasylyev M (Ukraine), Verhaz A (Bosnia-Herzegovina), Yurin O (Russia), Yancheva N (Bulgaria), Zabłocka H (Poland),
References
- Anon . 2020. EACS and BHIVA Statement on risk of COVID-19 for people living with HIV (PLWH)https://eacsociety.org/home/covid-19-and-hiv.html 1 April 2020. [Google Scholar]
- Anon . 2020. UNAIDS and China working together during the COVID-19 outbreak to ensure that people living with HIV continue to get treatment.https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2020/february/20200218_china_covid19 . Date: February 19, 2020 Date Accessed: April 1, 2020. [Google Scholar]
- Balayan T., Oprea C., Yurin O., Jevtovic D., Begovac J., Lakatos B. People who inject drugs remain hard-to-reach population across all HIV continuum stages in Central, Eastern and South Eastern Europe - data from Euro-guidelines in Central and Eastern Europe Network. Infect Dis (Lond) 2019;51:277–286. doi: 10.1080/23744235.2019.1565415. [DOI] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control . 2020. COVID-19 situation update worldwide, as of 21 May 2020. Available at: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases. [Accessed on 22 May 2020] [Google Scholar]
- Gokengin D., Oprea C., Begovac J., Horban A., Zeka A.N., Sedlacek D. HIV care in Central and Eastern Europe: How close are we to the target? Int J Infect Dis. 2018;70:121–130. doi: 10.1016/j.ijid.2018.03.007. [DOI] [PubMed] [Google Scholar]
- Guo W., Weng H.L., Bai H., Liu J., Wei X.N., Zhou K. [Quick community survey on the impact of COVID-19 outbreak for the healthcare of people living with HIV] Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:663–667. doi: 10.3760/cma.j.cn112338-20200314-00345. [DOI] [PubMed] [Google Scholar]
- Jiang H., Zhou Y., Tang W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV. 2020;7(5):e308–e309. doi: 10.1016/S2352-3018(20)30105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalska J.D., Oprea C., de Witt S., Pozniak A., Gokengin D., Youle M. Euroguidelines in Central and Eastern Europe (ECEE) conference and the Warsaw Declaration - a comprehensive meeting report. HIV Med. 2017;18:370–375. doi: 10.1111/hiv.12436. [DOI] [PubMed] [Google Scholar]
- Kowalska J.D., Bursa D., Gokengin D., Jilich D., Tomazic J., Vasylyev M. HIV health care providers are ready to introduce pre-exposure prophylaxis in Central and Eastern Europe and neighbouring countries: data from the Euroguidelines in Central and Eastern Europe (ECEE) Network Group. HIV Med. 2018;19:629–633. doi: 10.1111/hiv.12641. [DOI] [PubMed] [Google Scholar]
- Liu X., Kakade M., Fuller C.J., Fan B., Fang Y., Kong J. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012;53:15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saglietto A., D’Ascenzo F., Zoccai G.B., De Ferrari G.M. COVID-19 in Europe: the Italian lesson. Lancet. 2020 doi: 10.1016/S0140-6736(20)30690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]