Sir,
Coronavirus disease 2019 (COVID-19) due to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has infected >3.3 million people and caused 238,628 deaths [1]. With reference to our experience of the SARS-CoV outbreak [2], pandemic influenza A virus H1N1 [3] and sporadic cases of avian influenza A virus H7N9 [4] in Hong Kong, we implemented proactive infection control measures including active surveillance, isolation of suspected and confirmed cases in airborne infection isolation rooms (AIIRs), provision of rapid molecular diagnostic testing, and notification to the Hospital Authority and Department of Health, Hong Kong Special Administrative Region, China [5,6]. However, the AIIRs in the hospitals in Hong Kong were fully occupied due to an increasing number of symptomatic people returning from countries with local transmission, as well as an increasing number of COVID-19 patients in Hong Kong, and it was thought that suspected cases of COVID-19 might need to be hospitalized in non-AIIRs, which would pose a potential risk to healthcare workers (HCWs).
The innovative idea to set up a temporary test centre (TTC) at AsiaWord-Expo (AWE) (https://www.asiaworld-expo.com/), within the Hong Kong International Airport complex, was put into practice, with an interval of 48 h between visiting the site (21:00 h on 18th March 2020) and commencement of service (08:00 h on 20th March 2020) [7]. The project was initiated and supported by the Quality and Safety Division, Hospital Authority and Hong Kong Government, respectively. A medical director and a chief nursing officer were seconded to AWE for administration, logistic and manpower allocation. An infection control officer and a senior infection control nurse from a university-affiliated hospital were invited to participate in the project to coordinate and implement appropriate infection control measures to prevent cross-infection among patients (clinically stable symptomatic returning travellers aged 12–60 years) and HCWs.
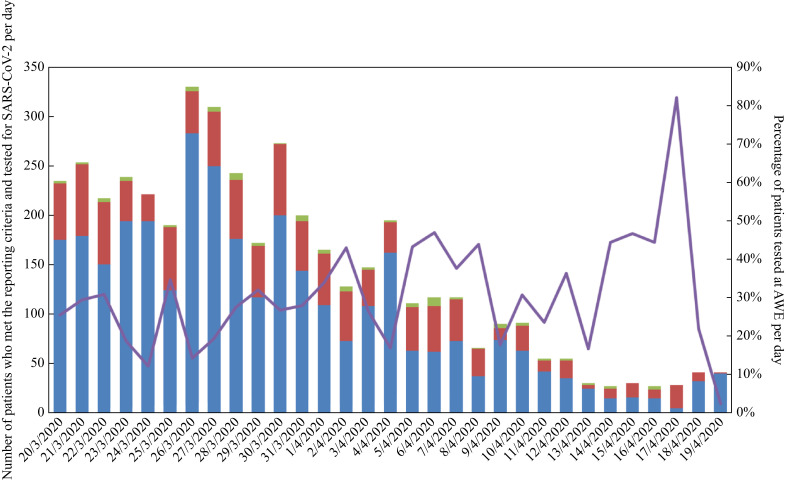
The implementation of infection control measures in a non-hospital setting was challenging. It was important to design a unidirectional workflow for both patients and HCWs in the large hall (∼60,000 square feet) at AWE. The hall was divided into two zones – a clean zone (∼30% of area) and a patient zone (∼70% of area) – with clear demarcation by double-fencing. The clean zone included a staff area for rest, dining and uniform changes; a gowning area; and a central command centre. The patient zone included areas for patient registration, assessment, collection of clinical specimens, and waiting for diagnostic test results. If the patients tested positive for SARS-CoV-2, they were transferred to a designated waiting area in the patient zone to await hospital admission. The degowning area was located at the exit of the patient zone. Infection control refresher training was provided to 80 HCW volunteers who were working in seven healthcare networks in Hong Kong. It was critically important to prevent transmission of SARS-CoV-2 in the TTC, especially for HCWs working in an unfamiliar setting. An audit of gowning and degowning of personal protective equipment (PPE), including gloves, gown, N95 respirator and faceshield, was performed for nine doctors, 41 nurses, 12 clerical staff, four supporting staff and 14 cleaning staff. A buddy system was introduced for directly-observed degowning of PPE to prevent the risk of self-contamination during degowning. HCWs were reminded to report respiratory symptoms and were tested for SARS-CoV-2 if indicated. The clean zone was disinfected once every two hours, and the patient zone was disinfected hourly and immediately after patient discharge using sodium hypochlorite (1000 ppm). As the indoor air of the hall underwent six air changes per hour without AIIRs at AWE, partitions were built to collect nasopharyngeal swabs (NPSs) in the outdoor covered area, which was adjacent to the hall. Two 88-cm-diameter fans were set to enhance air changes around the specimen collection area, in addition to natural ventilation. The NPSs were sent to the microbiology laboratory every 2 h for rapid molecular diagnostic testing, as described previously [6]. From 20th March 2020 to 19th April 2020, 1210 symptomatic (27.2%) cases out of 4445 patients who met the reporting criteria were tested at TTC. Eighty-eight (7.3%) of these 1210 patients tested positive for SARS-CoV-2 (Figure 1 ). Another 1122 (92.7%) patients who tested negative for SARS-CoV-2 were discharged for 14 days of home quarantine by order of the Department of Health. Therefore, the TTC reduced the number of hospital admissions by 36 patients per day during its 31 days of operation.
Figure 1.
Number of patients who met the reporting criteria and tested for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) in public hospitals and the temporary test centre at AsiaWorld-Expo (AWE) in Hong Kong. Green bars, patients who met the reporting criteria and tested positive for SARS-CoV-2 at AWE per day; red bars, patients who met the reporting criteria and tested negative for SARS-CoV-2 at AWE per day; blue bars, patients who met the reporting criteria and tested for SARS-CoV-2 in public hospitals (excluding AWE) per day; purple line, percentage of patients who met the criteria and tested at AWE per day.
During public health emergencies, innovative ideas and rapid responses are required to cope with the challenges. Fangcang shelter hospitals were built in China to cope with the overwhelming number of patients needing hospitalization [8]. In Hong Kong, a TTC was set up within 48 h to test almost one-third of clinically stable patients who were originally required to undergo tests in hospitals. On 19th April 2020, the TTC was closed when the service demand was no longer required, and the hall was disinfected by sodium hypochlorite (1000 ppm) and ultraviolet irradiation. Following 14 days of medical surveillance, no cases of infection were identified among the HCWs who worked in the TTC. This concept provides a model to test travellers at national borders to minimize the risk of importation of SARS-CoV-2.
Acknowledgements
We wish to thank our healthcare workers for combating COVID-19, especially those who were working at the TTC at AWE, Hong Kong. We also wish to thank administrative and frontline staff at AWE for supporting this project.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.World Health Organization . WHO; Geneva: 2020. Coronavirus disease 2019 (COVID-19). Situation Report – 104.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200503-covid-19-sitrep-104.pdf?sfvrsn=53328f46_2 Available at: [Google Scholar]
- 2.Cheng V.C., Lau S.K., Woo P.C., Yuen K.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 2007;20:660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng V.C., To K.K., Tse H., Hung I.F., Yuen K.Y. Two years after pandemic influenza A/2009/H1N1: what have we learned? Clin Microbiol Rev. 2012;25:223–263. doi: 10.1128/CMR.05012-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng V.C., Tai J.W., Lee W.M., Chan W.M., Wong S.C., Chen J.H. Infection control preparedness for human infection with influenza A H7N9 in Hong Kong. Infect Control Hosp Epidemiol. 2015;36:87–92. doi: 10.1017/ice.2014.2. [DOI] [PubMed] [Google Scholar]
- 5.Cheng V.C.C., Wong S.C., To K.K.W., Ho P.L., Yuen K.Y. Preparedness and proactive infection control measures against the emerging novel coronavirus in China. J Hosp Infect. 2020;104:254–255. doi: 10.1016/j.jhin.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Government of the Hong Kong Special Administrative Region . Government of the Hong Kong Special Administrative Region; Beijing: 2020. Temporary test centres speed up tests for people upon arrival.https://www.info.gov.hk/gia/general/202003/19/P2020031900664.htm Press release. Available at: [Google Scholar]
- 8.Chen S., Zhang Z., Yang J., Wang J., Zhai X., Bärnighausen T. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395:1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]