Dear Editor,
Although birth rate in Portugal is the fourth lowest in Europe and the number of COVID-19 cases in our country is one of the lowest, we already managed a case of a pregnant woman at term infected with SARS-CoV-2 who went into labor at term [1].
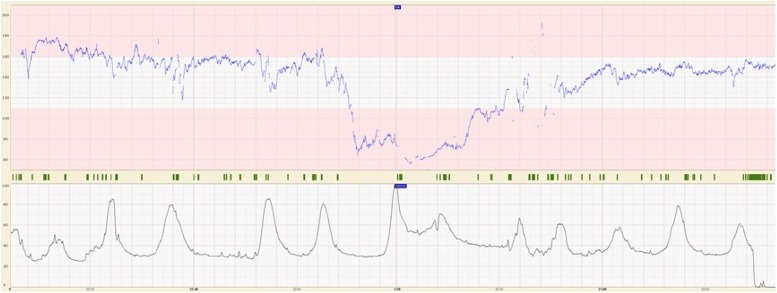
On March 17th 2020, in a level III hospital in Porto, a Caucasian 31-year-old woman with 38 weeks’ gestation was admitted at the obstetrical emergency department. She was a healthy gravida 2 para 1, with no complications during pregnancy. At admission, she was complaining of mild painful uterine contractions for a few hours. She was in home isolation as her husband was diagnosed with COVID-19 and hospitalized on March 12th 2020. At admission, she presented dry cough, with no fever, chills or shortness of breath. Because she was a close contact of a confirmed COVID-19 case, she was attended as a suspected case and settled in an isolation room. SARS-CoV-2 was detected by reverse-transcription polymerase chain reaction (RT-PCR) analysis on nasal and oropharyngeal swabs. After obstetric evaluation, latent phase of labor was diagnosed, the cervix was 3 cm dilated and 30 % effaced. Care in labor continued in the same isolation room. All health care workers in contact with the pregnant woman wore appropriate personal protective equipment for contact and airborne precautions with eye protection. Epidural analgesia was performed as earlier as possible and labor augmentation with oxytocin was started. The fetus was monitored with external continuous cardiotocography and cervical dilation was assessed every two hours. Ten hours after admission, cervix was full dilated and cardiotocography became suspicious (Fig. 1 ) requiring acute tocolysis with salbutamol. Subsequently, cardiotocography exhibited a normal fetal pattern and an operative vaginal delivery was performed with fetal vacuum extraction, in order to shorten the second stage of labor. Umbilical cord was immediately clamped without neonate-maternal contact. The female newborn weighed 3240 g and Apgar score was 9 at 1st and 10 at 5th minutes. The child was separated from the mother immediately after birth and placed in a single-patient negative pressure room. Newborn nasal and oropharyngeal swabs RT-PCR test for SARS-CoV-2 were performed. Two hours after birth newborn tested negative and the repeated test (at 48 h of life) was also negative. Mother was discharged at 3rd day postpartum, symptomless, waiting for recovery criteria at home. The newborn remained at nursery unit until family provide conditions for receiving her at home. The mother wished to breastfeed and started mechanical breast stimulation, in order to breastfeed soon after COVID-19 recovery.
Fig. 1.
Intrapartum cardiotocography in a pregnant woman with mild COVID-19.
COVID-19 is a highly contagious infection, requiring strictly planned intrapartum care for the safety of mother, newborn and healthcare workers. From previous reports, no evidence of intrauterine infection was found. [2] However, there are concerns whether pregnant women with COVID-19 should be allowed to deliver vaginally. There are no studies comparing the risk of neonatal COVID-19 according to the mode of delivery. From the published case series of pregnant women with COVID-19, only two had vaginal deliveries, both were preterm and one of them was a twin’s pregnancy [2,3]. Abnormal intrapartum cardiotocography has been frequently reported in women with COVID-19, probably increasing the rate of cesarean section among them. Since it seems there is an increased risk of intrapartum fetal compromise in women infected with COVID-19, continuous electronic fetal monitoring in labor should be recommended for all women with COVID-19.
This obstetrical case report supports experts’ opinion that women with COVID-19 without severe disease, should be offered vaginal delivery if labor has normal progress, guarantying that continuous electronic fetal monitoring is provided and appropriate infection prevention and control measures are in place.
Disclosure statement
The authors have nothing to disclose. The authors report no conflict of interest.
This study had no financial support for the research.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships
Acknowledgments
We thank all health care professionals across departments for being committed and trained in advance, allowing this case to be managed in our hospital.
References
- 1.Direção Geral de Saúde [Internet] Relatório de situação nº 18 c2020 [cited 2020 Mar 20] Available from: https://covid19.min-saude.pt/wp-content/uploads/2020/03/i026039.pdf.
- 2.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mullins E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–592. doi: 10.1002/uog.22014. [DOI] [PubMed] [Google Scholar]