Abstract
Introduction
Involving laypersons in response to out-of-hospital cardiac arrest through mobile-phone technology is becoming widespread in numerous countries, and different solutions were developed. We performed a systematic review on the impact of alerting citizens as first responders and to provide an overview of different strategies and technologies used.
Methods
We searched electronic databases up to October 2019. Eligible studies described systems to alert citizens first responders to out-of-hospital cardiac arrest through text messages or apps. We analyzed the implementation and performance of these systems and their impact on patients’ outcomes.
Results
We included 28 manuscripts describing 12 different systems. The first text message system was implemented in 2006 and the first app in 2010. First responders accepted to intervene in median (interquartile) 28.7% (27–29%) of alerts and reached the scene after 4.6 (4.4–5.5) minutes for performing CPR. First responders arrived before ambulance, started CPR and attached a defibrillator in 47% (34–58%), 24% (23–27%) and 9% (6–14%) of cases, respectively. Pooled analysis showed that first responders activation increased layperson-CPR rates (1463/2292 [63.8%] in the intervention group vs. 1094/1989 [55.0%] in the control group; OR = 1.70; 95% CI, 1.11–2.60; p = 0.01) and survival to hospital discharge or at 30 days (327/2273 [14.4%] vs. 184/1955 [9.4%]; OR = 1.51; 95% CI, 1.24–1.84; p < 0.001).
Conclusions
Alerting citizens as first responders in case of out-of-hospital cardiac arrest may reduce the intervention-free time and improve patients’ outcomes.
Keywords: Out-of-hospital cardiac arrest, First responders, Cardiopulmonary resuscitation, Mobile-phone technology
Introduction
Out-of-hospital cardiac arrest (OHCA) is a leading cause of mortality in the world. Due to low survival rates and to the high risk for irreversible neurological damage and disability in survivors, it is a significant public health issue. Survival rates following OHCA vary significantly across geographic regions ranging between 0.6% and 25%.1 Every year in Europe, 275,000 people have OHCA, with only 10% surviving to hospital discharge.2 Emergency medical services (EMS) treat 34 per 100,000 person-years suffering from OHCA in Europe, 53 in North America, 50 in Australia, and 59 in Asia. Rates of survival to hospital discharge are poor with only 7.6% surviving in Europe, 6.8% in North America, 9.7% in Australia, and 3.0% in Asia.1
Multiple factors influence survival after OHCA including patient characteristics, location, presenting rhythm, bystander-initiated cardiopulmonary resuscitation (CPR), ambulance response times and emergency system characteristics. Advanced medical interventions including vasopressors,12 antiarrhythmics,13 mechanical chest compression devices14 and tracheal intubation,15, 16, 17 have failed to show convincing effects on survival with good neurological outcome.
Furthermore, the most important modifiable factor affecting survival is bystander-CPR3 and when it is immediately performed before the arrival of EMS, the chances of survival are three times higher.4 Conventional public health approaches to increase rates of lay bystander care in the community include the development of public access defibrillation programmes and the education of citizens to provide effective care in case of OHCA. However, these strategies are not cost-effective and, despite outstanding efforts in training, rates of bystander-CPR and defibrillation remains low.6, 7
The potential role of mobile technology in out-of-hospital emergencies was first described in the literature in 2007,5 and it is now becoming widespread in numerous countries. Where adopted, the use of mobile-phone technology activated by EMS dispatch centres allows citizens to provide CPR and defibrillation to victims of sudden cardiac arrest. Citizens willing to provide assistance in case of OHCA can voluntarily register in a first responder network. When an OHCA occurs, the nearest citizens are alerted simultaneously to the dispatch of professional responders, hopefully increasing the proportion of cases in which CPR is performed before ambulance arrival.22
Different solutions were developed to locate and alert citizens as first responders but an overview of the characteristics of available technologies and their impact on patients’ outcomes has never been previously performed. We hypothesized that a comprehensive overview would inform clinicians, researchers and software developers for future research and development of these systems. Moreover, policymakers could take inspiration from these results. Accordingly, we decided to conduct a systematic review to identify the existing systems and technologies to locate and alert citizens acting as first responders to nearby OHCAs, determine their technical characteristics and analyze their impact in terms of rates of bystander-CPR, ROSC and survival.
Methods
This systematic review was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines8, 9 and the protocol was registered in PROSPERO (CDR 42020146905).
Search strategy and study selection
We systematically searched PubMed, Embase, BioMedCentral, Cochrane Central Register of Controlled Trials databases for pertinent studies from the earliest publication date available through October 31st, 2019. Backward snowballing was applied to retrieve additional manuscripts. We also retrieved the references of articles identified by this search strategy and selected those we considered relevant. In addition, websites of identified systems and conference proceedings were searched for additional studies and information.
We considered eligible randomized controlled trials (RCTs), observational trials, and case series published in peer-reviewed journals and conference proceedings fulfilling all the following criteria: (a) the article described a system able to locate and alert citizens first responders to nearby OHCA and (b) the system was either based on text messages or mobile application. We excluded systematic reviews, editorials, literature reviews, and articles describing systems to dispatch professional first responders (e.g. firefighters, police). After removal of duplicates, eligibility assessment was performed independently by two investigators (TS, OP) at title/abstract level. The final selection of included articles was based on complete manuscripts with disagreements solved by consensus under the supervision of one investigator (GL).
Data extraction
Data were independently extracted by two authors (TS, OP) using a standardized form with disagreements resolved by discussion and involving a third reviewer when required. Extracted data included first author, publication year, country, characteristics and technical aspects of the system (e.g. technology and platform adopted, activation radius, destination of first responders, active time, activation criteria, training needed, and recruitment of first responders), alerting process variables (e.g. acceptance rates, number of activations, response times, and arrival prior EMS), relevant outcomes (e.g. rates of bystander-CPR, ROSC, survival to hospital discharge or 30 days, and survival with good neurological outcomes), and risk of bias. We did not apply any imputation for missing data.
Statistical analysis
We planned to perform a meta-analysis of RCTs to compare the effect on the outcome of alerting first responders through mobile phone systems versus conventional EMS response. Since our systematic literature search identified only one RCT corresponding to the inclusion criteria, we decided to include in our meta-analysis also non-RCTs comparing mobile phone systems with conventional EMS response. The primary outcome for the meta-analysis was rate of bystander CPR. Secondary outcomes included rate of ROSC, overall survival to hospital discharge or 30-days, and survival with good neurological outcome. We calculated individual and pooled odds ratio (OR) for dichotomous outcomes with corresponding 95% confidence intervals (CI). Data were analyzed using the Mantel–Haenszel method. Heterogeneity analysis was performed with Cochran Q statistic and quantified with I 2. Heterogeneity with an I 2 > 25% was considered significant: fixed effect and random-effects models were used in case of low and high statistical heterogeneity, respectively. For pooled outcome analyses, a p-value <0.05 was considered significant. For studies included in the pooled analysis, risk of bias of RCTs was assessed following the recommended tool of Cochrane Collaboration (randomized sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective reporting, other bias).10 In contrast, for non-RCTs, the tool Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I) was used.11 Each item was evaluated by two trained investigators and an overall judgement of low, high, or unclear risk of bias provided. Studies were classified as “high risk of bias” if they had at least one item reported as high risk of bias, at “unclear risk of bias” if they had at least one item judged to carry an unclear risk of bias, and at low risk of bias if all of the items were at low risk of bias. Data were analyzed using RevMan 5.3. software (Review Manager, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Results
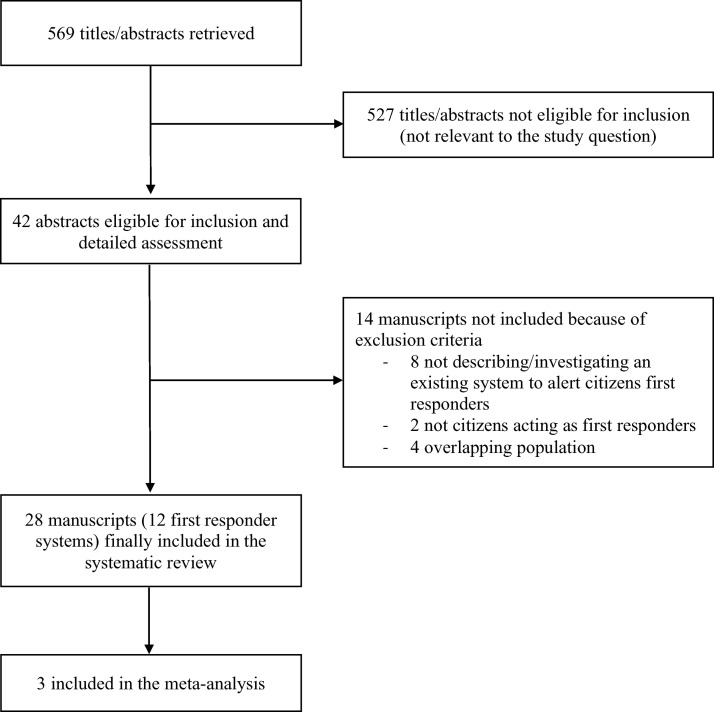
A total of 569 references were examined at the title/abstract level. After initial screening, a total of 42 studies were eligible for inclusion and detailed assessment. After exclusion of further 14 manuscripts that did not meet inclusion criteria (details in Supplemental Table 1), we included a total of 28 studies (comprising 11 conference proceedings) in the final analysis (Fig. 1 ).18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43 These 28 manuscripts were published between 2011 and 2019 and described 12 unique systems deployed in 16 different countries in the world. Four out of 28 manuscripts reported data on ROSC, four on survival to hospital discharge or at 30 days, and only one of them on survival with good neurological outcome. No study reported long-term outcomes (Table 3). Data extracted from one RCT and two observational studies comparing alerting first responders to OHCAs versus standard emergency response were meta-analyzed (Table 1 ).
Fig. 1.
Selection of included studies.
Table 3.
Performance of first responders systems.
| Name of system | Acceptance rates | First responders arrived prior to EMS | Time to arrival of first responders | CPR performed by first responders | AED attached by first responders | Shockable rhythm | ROSC | Survival to hospital discharge/30 days | Good neurological outcome (CPC 1–2) |
|---|---|---|---|---|---|---|---|---|---|
| GoodSAM18 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Momentum19, 29, 34 | n/a | 53.9% | 5.6 minb (Text message) 3.5 minb (App) |
n/a | n/a | 42% (Text message) 23%, 37% (App) |
n/a | 17% (Text Message) 28% (App) |
n/a |
| Mobile Lifesaver Service (SMSlivräddare)21, 22, 43 | 29% | 45%, 23%, 26% | 6.3 minb 9.3 minc (App) |
30%, 13%, 27% | 9% | 19.3% | 29.4% | 11.2% | n/a |
| Lee et al.a 23 | n/a | n/a | n/a | n/a | n/a | 19.8% | 13.1% | 12.7% | 8.3% |
| AED-Alert24 | 28.3% | 40.4% | n/a | 34.6% | 3.5% | n/a | n/a | n/a | |
| HartslagNu (HeartbeatNow)20, 25, 26, 31, 37, 39, 41 | n/a | n/a | n/a | 24.7%, 18% | 12%, 26.8%, 18% | 43%, 59.9%, 50% | 41.4% | 27.1% | n/a |
| FirstAED27, 28, 38 | n/a | 94.3%, 89%, 95% | 4.1, 4.3 minb 5.8 minc |
n/a | n/a | n/a | n/a | n/a | |
| Good Samaritan30 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| PulsePoint Respond32, 40 | 23% | n/a | n/a | 25% | n/a | n/a | n/a | n/a | |
| Mobile Rescuers33 | n/a | 59% | 4 minb | n/a | n/a | 63% | n/a | n/a | |
| myResponder35 | 29.3% | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| DAE RespondER42 | n/a | 19% | ∼2 minb in 25% of cases | n/a | n/a | n/a | n/a | n/a |
Name of the app/system not found.
Direct to OHCA location for performing CPR.
After collecting an AED.
ROSC = return of spontaneous circulation, CPC = cerebral performance category, OHCA = out-of-hospital cardiac arrest, CPR = cardiopulmonary resuscitation.
Table 1.
Summary of included studies ordered by year of publication.
| First author | Country | Journal | Year | Type | Overall risk of biasa |
|---|---|---|---|---|---|
| Ringh, M.21 | Sweden | Resuscitation | 2011 | Prospective observational | n/a |
| Scholten, A.C.24 | Netherlands | Resuscitation | 2011 | Survey | n/a |
| Henriksen, F.L.38 | Denmark | Abstract | 2012 | n/a | n/a |
| Henriksen, F.L.28 | Denmark | Abstract | 2013 | Prospective observational | n/a |
| Roman, B.29 | Switzerland | Abstract | 2013 | Survey | n/a |
| Zijlstra, J.A.20 | Netherlands | Resuscitation | 2014 | Prospective observational | n/a |
| Henriksen, F.L.28 | Denmark | Abstract | 2014 | Prospective observational | n/a |
| van der Worp, W.31 | Netherlands | Abstract | 2014 | Retrospective observational | n/a |
| Ringh, M.22 | Sweden | N Engl J Med | 2015 | Randomized controlled trial | Low |
| Henriksen, F.L.27 | Denmark | Abstract | 2015 | Prospective observational | n/a |
| Pijls, R.W.25 | Netherlands | Resuscitation | 2016 | Prospective observational | Serious |
| Brooks, S.C.32 | USA | Resuscitation | 2016 | Survey | n/a |
| Smith, C.M.18 | UK | Resuscitation | 2017 | Commentary | n/a |
| Caputo, M.L.19 | Switzerland | Resuscitation | 2017 | Prospective observational | n/a |
| Pijls, R.W.26 | Netherlands | Eur Heart J Acute Cardiovasc Care | 2017 | Prospective observational | n/a |
| Stroop, R.33 | Germany | Abstract | 2017 | Prospective observational | n/a |
| Dainty, K.N.40 | USA | JMIR Mhealth and Uhealth | 2017 | Survey | n/a |
| Berglund, E.43 | Sweden | Resuscitation | 2018 | Prospective observational | n/a |
| Derkenne, C.30 | France | Resuscitation | 2018 | Letter to the Editor | n/a |
| Pijls, R.W.41 | Netherlands | Neth Heart J | 2018 | Observational retrospective | n/a |
| Lee, S.Y.23 | South Korea | Resuscitation | 2019 | Prospective observational | Serious |
| Auricchio, A.34 | Switzerland | Resuscitation | 2019 | Prospective observational | n/a |
| Ng, Y.Y.35 | Singapore | Abstract | 2019 | Observational retrospective | n/a |
| Stroop, R.33 | Germany | Abstract | 2019 | Survey | n/a |
| Stroop, R.36 | Germany | Abstract | 2019 | Prospective observational | n/a |
| Stieglis, R.37 | Netherlands | Abstract | 2019 | Observational retrospective | n/a |
| Pijls, R.W.39 | Netherlands | Neth Heart J | 2019 | Observational retrospective | n/a |
| Del Giudice, D.42 | Italy | Resuscitation | 2019 | Letter to the Editor | n/a |
Only for studies included in the meta-analysis.
Characteristics of existing systems to locate and alert first responders
The first systems to alert and dispatch first responders to the site of an OHCA with text messages and app were implemented in 2006 in Canton Ticino (Switzerland)19, 29, 34 and 2010 in the USA respectively.32, 40
All systems alerted first responders in case of OHCA, with four alerting also in case of other medical emergencies.18, 27, 28, 32, 33, 36, 38, 40 In many cases, activation criteria expressly excluded children, OHCA with a non-cardiac cause and unsafe environments. Due to safety and privacy concerns, one system reported to avoid alerting first responders to private location32, 40 while the others did not provide details. Three systems specified to notify first responders only in defined time intervals during day hours, from 06–07 am to 11 pm21, 22, 43 and from 06 am to 10 pm,23 and two systems19, 20 were active 24/7. The vast majority of systems accepted CPR trained laypeople only (Table 2 ) and none of the systems declared to pay first responders for their service.
Table 2.
Summary of the 12 available systems to locate and alert first responders to nearby out-of-hospital cardiac arrests ordered by year of activation.
| Name of system | Country | Technology (platform) | Location tracking | Year of activation | Maximum activation radius | Active time | Activation criteria | First-responders training | Number of registered First Responders |
|---|---|---|---|---|---|---|---|---|---|
| Momentum19, 29, 34 | Switzerland | Text message (all) App (iOS, Android)b |
City or community (Text message) GPS (App) |
2006 (Text message), 2014 (App) | Same city or community (Text message) Dynamic (based on ambulance ETA) |
24/7 | OHCA Excluded: unsafe environment, trained bystander-CPR already initiated, ambulance ETA < first responders |
BLS/AED | 3400 |
| AED-Alert24 | Netherlands | Text message (all) App (iOS, Android) b |
Registered address (home or work) | 2008 | 1000 m | n/a | OHCA | BLS/AED | 6000 |
| HartslagNu (HeartbeatNow)20, 25, 26, 31, 37, 39, 41 | Netherlands | Text message (all) App (iOS, Android)b |
ZIP code derived location | 2008 | 1000 m | 24/7 | OHCA Excluded: address not known, non-cardiac cause, age < 8 years; ambulance ETA < first responders, AED already present, AED on-site, unsafe environment |
BLS/AED | >91,000 |
| Mobile Lifesaver Service (SMSlivräddare)21, 22, 43 | Sweden | Text message followed by a phone call (all) App (iOS, Android)b |
GPS | 2010 (Text message), 2015 (App) | 500 m (Text message) Dynamic (240–1,200 m) for CPR, 1,400 m for AED (App) |
6 am–11 pm, 7 am–11 pm | OHCA Excluded: age < 8 years, unsafe environment, non-cardiac cause, EMS-witnessed |
CPR | 23 ,097 |
| PulsePoint Respond32, 40 | USA | App (iOS, Android) | GPS | 2010 | 400 m | n/a | OHCA, medical emergencies Excluded: private location, unsafe environment |
Optional: BLS/AED | 1 ,569,084 |
| FirstAED27, 28, 38 | Denmark | App (iOS) | GPS | 2012 | n/a | n/a | OHCA, medical emergencies | CPR/AED and 3 h/year refresh course | 215 |
| Good Samaritan30 | France | App (iOS, Android) | n/a | 2015 | 150 m | n/a | OHCA | First aid | 10,000 |
| Lee et al.23a | Seul, Korea | Text message (all) | Registered address | 2015 | Same neighbourhood | 6 am–10 pm | OHCA | CPR | 63,924 |
| myResponder35 | Singapore | App (iOS, Android) | n/a | 2015 | 400 m | n/a | OHCA, minor fire, major incident | Suggested: CPR | 39,070 |
| GoodSAM18 | UK, Australia, New Zealand, India, USA, Brazil, South Africa | App (iOS, Android, Windows Phone) | GPS | 2015 | 300 m (London City) | n/a | OHCA, medical emergencies | Valid professional identification or CPR/AED training certificate | >8000 |
| DAE RespondER42 | Italy | App (iOS, Android) | GPS and registered addresses | 2017 | 5000 m | n/a | OHCA | No | 7130 |
| Mobile Rescuers33, 36 | Germany | App (iOS, Android) | n/a | n/a | n/a | n/a | OHCA | Yes | 740 |
a Name of the app/system not found.
Initially based on Text Message and then moved to app.
CPR = cardiopulmonary resuscitation, AED = automated external defibrillator, BLS = basic life support, OHCA = out-of-hospital cardiac arrest.
First responders located either within a prespecified activation radius from the OHCA location or on the same city, community or neighbourhood of the OHCA were notified through a text message or with the app. The systems calculated the distance between the current (or most recent) position of first responders obtained through Global Positioning System (GPS) tracking or from a set of registered addresses (e.g. work or home address) and the OHCA address provided by the caller. The activation radius varied among systems from 150 m30 up to 5 km,42 mainly due to the different characteristics of the area and the density of first responders. A complete overview of the strategies adopted by the different systems is available in Table 2. Remarkably, one system was developed to progressively expand the radius during each alert until a prespecified number of first responders was located and accepted to intervene.43 In Switzerland, the activation radius was dynamically adjusted based on the estimated time of arrival of the ambulance (the shorter the estimated time of arrival, the smaller the activation radius).19 For an optimal alert system, the minimum density of first responders was found to be at least ten first responders per square kilometre.38
Alerting first responders: text messages versus smartphone apps
Seven of the 12 identified systems were based on mobile applications installed on smartphones18, 27, 30, 32, 33, 35, 42 and 5 on text messages.19, 20, 21, 23, 24 Four text message systems were successively moved to a mobile app19, 20, 21, 24 for a total of 11 apps. Only one of the existing apps is available for the three main platforms (iOS, Android, and Windows Phone)18 while the remaining are available for both iOS and Android (n = 9)19, 20, 21, 24, 30, 32, 33, 35, 42 or only for iOS (n = 1).27 The characteristics of identified systems are summarized in Table 2.
Compared to text messages, the use of a mobile app increased up to 70% the proportion of first responders to be first on the scene with a reduction of the arrival time (3.5 min [2.8–5.2] vs. 5.6 min [4.2–8.5], p < 0.001) and an earlier initiation of CPR in an observational study. Survival to hospital discharge increased from 17% to 28% (OR 0.53, 95% CI 0.34–0.82, p = 0.004) in patients with both shockable and non-shockable rhythms.19
Dispatching first responders directly to the OHCA site versus retrieving an AED first
Among the identified alerting systems, we observed three different approaches to dispatch and engage first responders. The first strategy prioritized first responders to reach the OHCA site directly to deliver early CPR and discretionally retrieve an AED19, 21, 22, 24, 34, 42 significantly shortening the total intervention time and the time of CPR initiation (197 s [120–306 s] vs. 275 [184–414 s]; p < 0.001) in one observational study.34 In the second strategy, the closest first responders were instructed to collect an AED and the remaining went directly to the patient.20, 25, 31, 39, 41, 43 A third strategy organized a team of three responders with two of them reaching the event site (one for performing CPR and one for coordinating) and the third one collecting the AED.27, 28, 38 although no study directly compared the different approaches, arrival before ambulance in these three strategies was respectively 58–69%, 59–100%, and 90–99%.
Rates of alert acceptance and first responders-initiated CPR and defibrillation
The median rate of first responders who accept to intervene to an OHCA among those alerted was 28.7% (27–29%) across the different identified systems.
On median, a first responder reached the scene for performing CPR after 4.3 (4.1–4.9) minutes and delivered an AED after 7.5 (6.7–8.4) minutes. First responders arrived before EMS in median 47% (34–58%) of occasions, performed CPR in median 24% (23–27%) of cases and attached an AED in 9% (6–14%) of patients. Among those victims who had an AED positioned by the first responder, the first rhythm registered was shockable in 35% (25–47%) of cases (Table 3 ).
Effect of first responders on bystander-CPR, ROSC and survival rates
Three studies recruiting 4282 OHCA patients compared alerting first responders versus standard EMS response and reported data on bystander-CPR rates, ROSC and survival to hospital discharge or at 30 days: one RCT,22 one before-and-after study23 and one low-quality retrospective cohort study.25
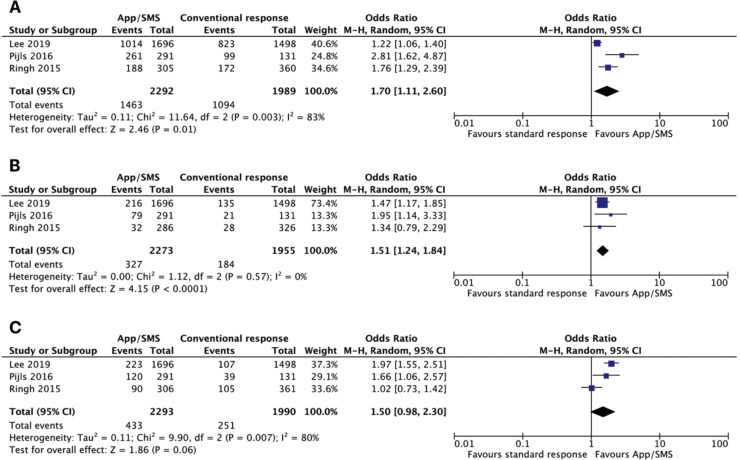
Pooled analysis showed that the use of a first responders system compared to the standard EMS response was associated with increased likelihood to receive CPR before ambulance arrival (1463/2292 [63.8%] in the app/text message group vs. 1094/1989 [55.0%] in the control group; OR = 1.70; 95% CI, 1.11–2.60; p for effect = 0.01; I 2 = 83%) (Fig. 2A) and survival to hospital discharge or at 30 days (327/2273 [14.4%] in the app/text message group vs. 184/1955 [9.4%] in the control group; OR = 1.51; 95% CI, 1.24–1.84; p for effect < 0.001; I 2 = 0%) (Fig. 2B). The activation of first responders was not associated with increased likelihood of ROSC (433/2293 [18.9%] in the app/text message group vs. 251/1990 [12.6%] in the control group; OR = 1.50; 95% CI, 0.98–2.30; p for effect = 0.06; I 2 = 80%) (Fig. 2C). Overall, risk of bias analysis (Supplemental Tables 2 and 3) showed that among the three studies included in the meta-analysis, two were at serious risk of bias23, 25 and the remaining one (the only RCT) was considered at low risk of bias.22
Fig. 2.
Forest plots for rate of bystander-CPR (A), survival to discharge or 30 days (B), and return of spontaneous circulation (C). df = degrees of freedom, M-H = Mantel–Haenszel.
Only one before-and-after study23 presented data on survival with good neurologic outcome: patients treated in the period after implementation of a text message alert system were more likely to survive to hospital discharge with good neurological outcome (8.3% vs. 4.5%, p < 0.001) when compared to the period before implementation.
Psychological burden on citizens first responders
In Germany, the psychosocial burden among first responders was evaluated and revealed a predominantly high level of coping skills and psychosocial resilience. However, a small percentage of first responders needed psychological aftercare.33 Preliminary findings suggested that the implementation of an after-care programme that comprises a follow-up, a telephone contact after 48 h and a hotline were useful.33 Only one system in the Netherlands24 had formal psychosocial support to first responders.
Discussion
In this comprehensive systematic review and meta-analysis, we investigated the impact of alerting citizens acting as first responders in the immediate vicinity of an OHCA with a text message or a smartphone app alert system. We found that implementing a system to alert first responders may reduce the period of time without intervention before EMS arrival. In many cases, first responders alerted through either text messages or mobile apps were able to timely reach the patient before ambulance arrival, start CPR and attach an AED. Furthermore, our meta-analysis suggested that patients who suffer an OHCA and are treated by first responders are more likely to receive CPR before ambulance arrival and survive to hospital discharge or at 30 days. However, the involvement of first responders did not improve rates of ROSC. Only one before-and-after study23 reported survival to hospital discharge with good neurological outcome and found an improvement after the implementation of the alert system.
It is well known that in case of OHCA, early CPR44 and early defibrillation45 improve survival. Unfortunately, nowadays surviving OHCA is often left to chance (i.e. to the casual presence of a bystander trained in CPR and willing to intervene) instead to a robust system with a strong emphasis on immediate recognition of cardiac arrest, activation of the emergency response system, early CPR and early defibrillation. Our review focused on a relatively novel technology that is cheap, simple, and universally present: smartphones and dedicated apps to improve the response to OHCA.
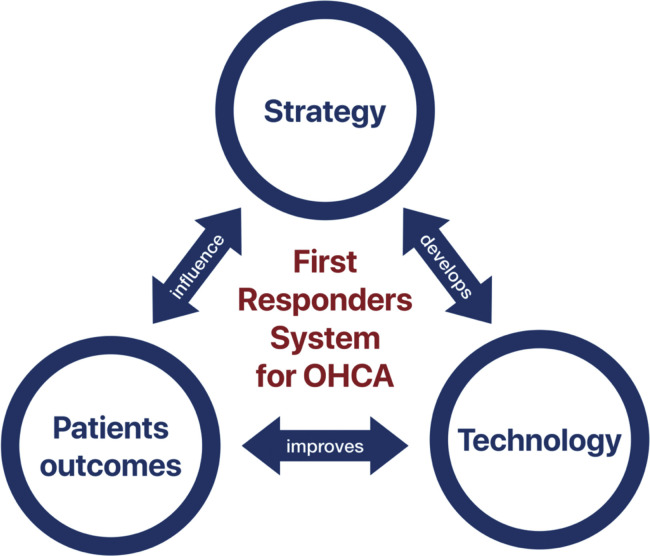
We found several differences in locating, alerting and managing first responders systems. (Table 2) Choosing the right approach to implement a network of first responders may have a considerable impact on the effectiveness of the system (Fig. 3 ). First, the number of notified citizens and the radius used to localize the nearest one are variable. This may reduce the proportion of OHCA in which a first responder is able to timely reach the location, in particular in cases of a low density of first responders or when they reach the scene by foot or by car. Second, not every system is active and functioning 24/7: some of these are deactivated during the night and others alert first responders only for OHCA occurring in public places. Third, directing first responders directly to the OHCA site or only after collecting an AED may have implications for patients’ outcomes and system management. One study in Switzerland reported a significant reduction in time of CPR initiation when dispatching first responders directly to the OHCA site without collecting an AED.34 However, collecting an AED before reaching the patient can still be useful if others first responders timely reach the location and start CPR or if a high-quality bystander-CPR is already in progress. Fourth, the majority of OHCAs occurs at home and privacy concerns may prevent alerting first responders in these cases. Notably, the results of a survey conducted in North American showed instead that citizens are comfortable to receive assistance in case of OHCA from first responders also in a private location.40
Fig. 3.
Strategy, technology and patients’ outcomes: the three dimensions of systems to locate and alert citizens first responders to nearby out-of-hospital cardiac arrests.
In recent years, with the rapid growth in technology, smartphones and mobile apps have become an essential part of our lives. Nowadays, first responder systems should be implemented on app-based systems. Compared to text message systems, apps offer the advantage of continuously geolocate the first responders with accuracy, real-time update of the details of the event, on-scene audio and video streaming, displaying the position of nearby AEDs and directing the first responders either to the OHCA location or to the nearest AED based on the estimated distance and time required. However, an active internet connection is mandatory to offer these functionalities, and this should be considered when implementing such systems in remote areas with inadequate network coverage. Given the accuracy of app geolocation, such technology may also allow to dynamically adjust the activation radius29 to alert only the nearest and most competitive first responder compared to the estimated time of arrival of ambulances. In a study carried out in Switzerland, the app-based system was found to significantly reduce the time to initiation of CPR and to increase rates of survival when compared to a text message system.19 Interestingly, the fifth-generation (5G) wireless network, thanks to its capability to process data at faster speeds, has the potential to further improve these systems. Examples of 5G applications will include the transmission of high-quality and latency-free video with augmented reality to help first responders who are on the scene of an OHCA, drone-delivered AEDs and highly accurate and continuous geolocation without ruining devices battery.
As reported by Brooks et al.,32 the efficiency of these systems may be negatively affected by some technical factors: volume of notifications, accuracy of information about OHCA location, inadequate activation radius, insufficient density of first responders in the area, and low specificity to trigger a cardiac arrest notification are all aspects that. Failure to obtain real-time GPS location from apps, and seasonal variability can further worsen these first responder systems. Moreover, considering that these apps rely on third-party devices with operating systems that could be subjected to changes and updates, a close technological monitoring should be implemented to avoid issues with the functioning of geolocation and alert system.47 Furthermore, during the outbreak of pandemics, efficiency of first responder systems may be affected due to concerns of disease transmission48 and healthcare institutions may consider providing updated guidelines and personal protective equipment to citizens first responders. To increase the number of first responders and overcome the risk of an insufficient density, many authors organized advertising campaigns in newspapers, websites, and social media and invited citizens after CPR training courses.20, 21, 22, 23, 24, 35, 39, 43 Moreover, laypeople working in the streets (e.g. taxi drivers, food-riders,46 mail carriers, and couriers) and in public places with an AED on-site should be involved in these projects for their ability to quickly reach the OHCA or to collect and deliver an AED.
The present study is the first systematic review to comprehensively identify the state-of-the-art on the topic, provide information for further development of first responder systems and inform future research. So far, our work represents the best evidence but has some limitations. First, we identified only one RCT. Second, we limited our search to systems published and described in the literature and thus this review may not provide a complete picture of all existing systems. Third, two out of the three studies included in the quantitative analyses carried a serious risk of bias. Abstracts, editorials and conference proceedings were included only in qualitative descriptions to provide a comprehensive overview of the available systems but did not have data that could be included in the meta-analysis. This finding underlines the paucity of available evidence in this field and the need for high-quality RCTs. Fourth, we identified a lack of data and no uniform reporting in many areas, hopefully informing future research. In particular, bystander-CPR rates before the implementation of first responder systems were not reported in the identified manuscripts except in one before-and-after study23 thus limiting the understanding of benefits of such technologies. Also, the important aspect of liability and safety of first responders was not covered in the identified articles: to protect lay people who offer assistance during an emergency situation, a Good Samaritan law should be implemented in every country. Furthermore, when interpreting our findings, the differences between countries in the healthcare organization, EMS system organization and clinical practice must be considered. The culture of action and education in resuscitation manoeuvres among the population of each country also has a huge impact on the effectiveness of these systems.
Two ongoing RCTs will hopefully provide more insights on the role of first responders alerted in response to OHCA. The Scandinavian AED and Mobile Bystander Activation Trial (SAMBA, ClinicalTrials.gov NCT02992873) is randomizing first responders to reach the OHCA location directly or only after collecting an AED. In both groups, at least one first responder will be alerted to provide only CPR along with standard EMS care. In Denmark, the HeartRunner Trial (ClinicalTrials.gov NCT03835403) is randomizing OHCAs to either activation of first responders or not (standard EMS care) to assess 30-day survival. Given the complex situations in which first responders are involved, this study will also evaluate the physical or psychological risks of activated first responders. Moreover, investigating the impact on long term outcomes and working towards the standardization of reporting data about first responders systems is highly emphasized.
Conclusions
Implementing mobile-phone systems to locate and alert citizens as first responders in case of OHCA may increase early CPR and defibrillation and improve patients’ outcomes. Our data suggest that first responders may be able to timely reach the OHCA before ambulance arrival and reduce the intervention-free time by starting CPR and attaching an AED. These advantages could lead to an improvement in rates of CPR performed before ambulance arrival and survival to hospital discharge or at 30 days. We identified several differences among first responder systems and found that the right choice of strategy and technological implementation play a critical role in their effectiveness. However, RCTs are needed to provide conclusive data.
Conflicts of interest
All authors do not have conflict of interest to declare.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.resuscitation.2020.05.006.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Berdowski J., Berg R.A., Tijssen J.G.P., Koster R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Atwood C., Eisenberg M.S., Herlitz J., Rea T.D. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005;67:75–80. doi: 10.1016/j.resuscitation.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Stiell I.G., Wells G.A., DeMaio V.J. Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS study phase I results. Ann Emerg Med. 1999;33:44–50. doi: 10.1016/S0196-0644(99)70415-4. [DOI] [PubMed] [Google Scholar]
- 4.Sasson C., Rogers M.A.M., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 5.Landoni G., Biselli C., Maj G., Zangrillo A. Faster rings in the survival chain: mobile phones could improve the response to the dedicated emergency call system. Resuscitation. 2007;75:547. doi: 10.1016/j.resuscitation.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 6.Gräsner J.-T., Lefering R., Koster R.W. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Ong M.E.H., Shin S.D., De Souza N.N.A. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS) Resuscitation. 2015;96:100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 8.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D., Liberati A., Tetzlaff J., Altman D.G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins J.P.T., Altman D.G., Gotzsche P.C. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sterne J.A., Hernán M.A., Reeves B.C. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perkins G.D., Ji C., Deakin C.D. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl J Med. 2018;379:711–721. doi: 10.1056/NEJMoa1806842. [DOI] [PubMed] [Google Scholar]
- 13.Kudenchuk P.J., Brown S.P., Daya M. Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N Engl J Med. 2016;374:1711–1722. doi: 10.1056/NEJMoa1514204. [DOI] [PubMed] [Google Scholar]
- 14.Gates S., Quinn T., Deakin C.D., Blair L., Couper K., Perkins G.D. Mechanical chest compression for out of hospital cardiac arrest: systematic review and meta-analysis. Resuscitation. 2015;94:91–97. doi: 10.1016/j.resuscitation.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Wang H.E., Schmicker R.H., Daya M.R. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2018;320:769. doi: 10.1001/jama.2018.7044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benger J.R., Kirby K., Black S. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac arrest on functional outcome: the AIRWAYS-2 randomized clinical trial. JAMA. 2018;320:779–791. doi: 10.1001/jama.2018.11597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jabre P., Penaloza A., Pinero D. Effect of bag-mask ventilation vs endotracheal intubation during cardiopulmonary resuscitation on neurological outcome after out-of-hospital cardiorespiratory arrest: a randomized clinical trial. JAMA. 2018;319:779–787. doi: 10.1001/jama.2018.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith C.M., Wilson M.H., Ghorbangholi A. The use of trained volunteers in the response to out-of-hospital cardiac arrest – the GoodSAM experience. Resuscitation. 2017;121:123–126. doi: 10.1016/j.resuscitation.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 19.Caputo M.L., Muschietti S., Burkart R. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: a comparison with SMS-based system notification. Resuscitation. 2017;114:73–78. doi: 10.1016/j.resuscitation.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Zijlstra J.A., Stieglis R., Riedijk F., Smeekes M., van der Worp W.E., Koster R.W. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out-of-hospital cardiac arrest dispatch system. Resuscitation. 2014;85:1444–1449. doi: 10.1016/j.resuscitation.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Ringh M., Fredman D., Nordberg P., Stark T., Hollenberg J. Mobile phone technology identifies and recruits trained citizens to perform CPR on out-of-hospital cardiac arrest victims prior to ambulance arrival. Resuscitation. 2011;82:1514–1518. doi: 10.1016/j.resuscitation.2011.07.033. [DOI] [PubMed] [Google Scholar]
- 22.Ringh M., Rosenqvist M., Hollenberg J. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2316–2325. doi: 10.1056/NEJMoa1406038. [DOI] [PubMed] [Google Scholar]
- 23.Lee S.Y., Shin S.D., Lee Y.J. Text message alert system and resuscitation outcomes after out-of-hospital cardiac arrest: a before-and-after population-based study. Resuscitation. 2019;138:198–207. doi: 10.1016/j.resuscitation.2019.01.045. [DOI] [PubMed] [Google Scholar]
- 24.Scholten A.C., van Manen J.G., van der Worp W.E., Ijzerman M.J., Doggen C.J.M. Early cardiopulmonary resuscitation and use of automated external defibrillators by laypersons in out-of-hospital cardiac arrest using an SMS alert service. Resuscitation. 2011;82:1273–1278. doi: 10.1016/j.resuscitation.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Pijls R.W.M., Nelemans P.J., Rahel B.M., Gorgels A.P.M. A text message alert system for trained volunteers improves out-of-hospital cardiac arrest survival. Resuscitation. 2016;105:182–187. doi: 10.1016/j.resuscitation.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 26.Pijls R.W., Nelemans P.J., Rahel B.M., Gorgels A.P. Factors modifying performance of a novel citizen text message alert system in improving survival of out-of-hospital cardiac arrest. Eur Heart J Acute Cardiovasc Care. 2018;7:397–404. doi: 10.1177/2048872617694675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henriksen F.L., Schakow H., Larsen M.L. The FirstAED global positioning system organizes a first responder team with distinct roles and ensures the possibility for early cardiopulmonary resuscitation and defibrillation. Resuscitation. 2015;96:11. doi: 10.1016/j.resuscitation.2015.09.025. [DOI] [Google Scholar]
- 28.Henriksen F.L., Schakow H., Larsen M.L. The langeland AED project—FirstAED—incorporates emergency dispatch, GPS technology, first responders with distinct roles, smartphones and an AED network. Resuscitation. 2013;84:S21. doi: 10.1016/j.resuscitation.2013.08.066. [DOI] [Google Scholar]
- 29.Roman B., Claudio B., Romano M. Non-professional first responders: organizational efficiency criteria in Ticino (Southern Switzerland) Resuscitation. 2013;84:S70. doi: 10.1016/j.resuscitation.2013.08.178. [DOI] [Google Scholar]
- 30.Derkenne C., Jost D., Briche F., Travers S., Tourtier J.-P. Letter by Derkenne et al. regarding the article, “The use of trained volunteers in the response to out-of-hospital cardiac arrest — the GoodSAM experience.”. Resuscitation. 2018;125:e3. doi: 10.1016/j.resuscitation.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 31.van der Worp W. Resuscitation by text-message responders in The Netherlands. Resuscitation. 2014;85:S55. doi: 10.1016/j.resuscitation.2014.03.139. [DOI] [Google Scholar]
- 32.Brooks S.C., Simmons G., Worthington H., Bobrow B.J., Morrison L.J. The PulsePoint Respond mobile device application to crowdsource basic life support for patients with out-of-hospital cardiac arrest: challenges for optimal implementation. Resuscitation. 2016;98:20–26. doi: 10.1016/j.resuscitation.2015.09.392. [DOI] [PubMed] [Google Scholar]
- 33.Stroop R., Hensel M., Strickmann B., Kerner T. Mobile-phone based alerting of CPR-trained volunteers simultaneously with ambulance can reduce resuscitation-free interval and improve outcome after out-of-hospital cardiac arrest – a prospective observational study. Resuscitation. 2019;142:e3. doi: 10.1016/j.resuscitation.2019.06.018. [DOI] [PubMed] [Google Scholar]
- 34.Auricchio A., Gianquintieri L., Burkart R. Real-life time and distance covered by lay first responders alerted by means of smartphone-application: implications for early initiation of cardiopulmonary resuscitation and access to automatic external defibrillators. Resuscitation. 2019;141:182–187. doi: 10.1016/j.resuscitation.2019.05.023. [DOI] [PubMed] [Google Scholar]
- 35.Ng Y.Y., Ng W.M., De Souza C.R., Ong M. Crowdsourcing first responders and public access defibrillation in Singapore. Resuscitation. 2019;142:e12. doi: 10.1016/j.resuscitation.2019.06.039. [DOI] [Google Scholar]
- 36.Stroop R., Eckert M., Poschkamp T., Kerner T., Goersch H. Smartphone based alerting: aftercare for first aiders – necessary or superfluous? Resuscitation. 2019;142:e10. doi: 10.1016/j.resuscitation.2019.06.034. [DOI] [Google Scholar]
- 37.Stieglis R., Koster R. Minimal AED and volunteer rescuers density needed for an effective lay rescuer network for out-of-hospital cardiac arrest. Resuscitation. 2019;142:e2. doi: 10.1016/j.resuscitation.2019.06.016. [DOI] [Google Scholar]
- 38.Henriksen F.L., Schakow H., Brandes A., Kaewkongnok B., Larsen M.L. The Langeland AED project – call for shorter response times (FirstAED) Scand J Trauma Resusc Emerg Med. 2012;19 doi: 10.1186/1757-7241-19-S2-P47. P47, 1757-7241-19-S2-P47. [DOI] [Google Scholar]
- 39.Pijls R.W.M., Nelemans P.J., Rahel B.M., Gorgels A.P.M. Characteristics of a novel citizen rescue system for out-of-hospital cardiac arrest in the Dutch province of Limburg: relation to incidence and survival. Neth Heart J. 2019;27:100–107. doi: 10.1007/s12471-018-1215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dainty K.N., Vaid H., Brooks S.C. North American public opinion survey on the acceptability of crowdsourcing basic life support for out-of-hospital cardiac arrest with the PulsePoint mobile phone App. JMIR Mhealth Uhealth. 2017;5:e63. doi: 10.2196/mhealth.6926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pijls R.W.M., Nelemans P.J., Rahel B.M., Gorgels A.P.M. Circumstances and causes of sudden circulatory arrests in the Dutch province of Limburg and the involvement of citizen rescuers. Neth Heart J. 2018;26:41–48. doi: 10.1007/s12471-017-1057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Del Giudice D., Semeraro F., Ristagno G. DAE RespondER: the Emilia Romagna app for a regional “community saving lives” system. Resuscitation. 2019;145:34–36. doi: 10.1016/j.resuscitation.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 43.Berglund E., Claesson A., Nordberg P. A smartphone application for dispatch of lay responders to out-of-hospital cardiac arrests. Resuscitation. 2018;126:160–165. doi: 10.1016/j.resuscitation.2018.01.039. [DOI] [PubMed] [Google Scholar]
- 44.Hasselqvist-Ax I., Riva G., Herlitz J. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 45.Kitamura T., Kiyohara K., Sakai T. Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med. 2016;375:1649–1659. doi: 10.1056/NEJMsa1600011. [DOI] [PubMed] [Google Scholar]
- 46.Scquizzato T., Landoni G., Forti A. Food-riders may improve the chain of survival in out-of-hospital cardiac arrests by delivering CPR and AEDs. Resuscitation. 2019;134:163–164. doi: 10.1016/j.resuscitation.2018.11.017. [DOI] [PubMed] [Google Scholar]
- 47.Scquizzato T., Landoni G., Semeraro F., Zangrillo A. Smartphone software update could potentially affect the efficiency of lay first-responders networks in out-of-hospital cardiac arrests. Resuscitation. 2019;144:15–16. doi: 10.1016/j.resuscitation.2019.08.030. [DOI] [PubMed] [Google Scholar]
- 48.Scquizzato T., Olasveengen T.M., Ristagno G., Semeraro F. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi: 10.1016/j.resuscitation.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.