Abstract
Coronavirus Disease-2019 (COVID-19) originated in the Wuhan, Hubei Province, China in November 2019 and has since been declared a pandemic by the WHO. COVID-19 is an acute infectious disease, primarily affecting the respiratory system. Currently, real-time reverse transcription polymerase chain reaction (RT-PCR) performed on respiratory specimens is considered the reference by which to diagnose COVID-19. However, the limitations of RT-PCR, specifically, the fact that it is time-consuming and inadequate for the assessment of disease severity, have affected the process of epidemiological disease containment and has taken a toll on the healthcare management chain. As the risk of infection for other patients and personnel must be kept to a minimum, the indications for imaging have to be carefully considered. Imaging is primarily performed in patients with a negative RT-PCR, but a high clinical suspicion of COVID-19, or, in patients with diagnosed COVID-19 who are suffering from moderate to severe symptoms. In this article, we review the typical imaging findings in COVID-19, the differential diagnoses, and common complications.
Keywords: COVID-19, Pneumonia, Infection, Ground-glass
1. Background
In late November 2019, a serious form of pulmonary illness originated in Wuhan City (Hubei Province, China) and engulfed a majority of the world [1]. This pneumonia outbreak was attributed to a novel coronavirus, a lipid-enveloped RNA virus, which was named by the International Committee on Taxonomy of Viruses severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) [2]. The disease caused by the virus was termed coronavirus disease-2019 (COVID-19). The virus outbreak presumably originated via a zoonotic transmission linked to the seafood market in Wuhan (China) and later accelerated with human to human transmission, causing the severe subsequent outbreak [1]. Since the original outbreak, SARS-CoV2 has rapidly spread across the world and, in January 2020, the World Health Organization (WHO) declared COVID-19 a global public health emergency [3]. By the 21 st of April 2020, more than 2.4 million individuals tested positive for SARS-CoV2, and it had caused more than 165,000 deaths [4].
In order to enter the human host cells, SARS-CoV2 attaches to angiotensin-converting enzyme 2 (ACE2) on the surface of the cells via its viron spike protein [5]. ACE2 is highly expressed on the surface of pulmonary epithelial cells, which explains the frequent pulmonary involvement in COVID-19 [5]. In addition to pulmonary epithelial cells, ACE2 is also expressed in the heart, ileum, kidney, bladder, and endothelial cells [5]. The involvement of endothelial cells might be the reason for the hypercoagulable state observed in some patients with severe disease [5].
COVID-19 includes a wide spectrum of symptoms, ranging from upper respiratory infection to perilous pneumonia, allied with acute respiratory distress syndrome (ARDS). The most common symptoms at presentation are fever, fatigue, dry cough, myalgia, and dyspnea [6]. Less commonly, patients present with headache, hemoptysis, diarrhea, or pleuritic chest pain [6]
Currently, real-time reverse transcriptase polymerase chain reaction (RT-PCR) on upper and lower respiratory track specimens is considered the reference standard with which to diagnose COVID-19 [7]. The sensitivity of the RT-PCR for diagnosing COVID-19 ranges between 50 % and 98 %, depending on the sampling of the specimen, the stage of the infection, and the quality of the test [8], with a pooled sensitivity estimate of 89 % [9]. Therefore, RT-PCR in symptomatic patients may initially yield negative results that may turn positive on repeat testing [10].
2. Role of imaging in the diagnosis of COVID-19 pneumonia
Imaging indications for the diagnosis and follow-up of patients with COVID-19 have been addressed by a number of scientific societies [[11], [12], [13]]. There is a general consensus that the imaging indications should be applied uniformly and carefully weighted to minimize the risk of infection to medical personnel and other patients.
Chest radiography is the most readily available modality for the detection of lung abnormalities in many centers. Compared to chest computed tomography (CT), chest radiographs are cheaper and are associated with a lower radiation dose. However, the lack of specificity, as well as sensitivity for detection of COVID-19, particularly in patients with no or only minor symptoms, must be considered [11,14]. For example, in suspected COVID-19 patients who eventually tested positive on RT-PCR, the reported sensitivity of baseline chest radiographs was reported to be 69 % [2]. Consequently, chest radiographs should be performed primarily in patients with moderate to severe symptoms to assess disease progression or diagnose complications [11]. The routine use of chest radiographs, however, is not considered to be indicated in stable, intubated patients with COVID-19 [11].
The American College of Radiology supports the view that the need for CT decontamination required after scanning a COVID-19 patient may interrupt radiological service accessibility, and proposes that portable chest radiographs should be considered to decrease the risk of cross-infection [13].
Chest ultrasound is primarily performed in some centers to triage patients, to monitor treatment effects, and for diagnosing complications of COVID-19 pneumonias, such as pleural effusions [15,16]. As with all other bed-side procedures in COVID-19 patients, ultrasound examinations should be kept to a minimum to avoid the risk of infection of the medical personnel.
Chest CT offers the advantage of providing significant information. The indication for CT depends primarily on the clinical context and resource constraints [11]. In general, imaging is not recommended for screening in asymptomatic individuals or in patients with RT-PCR confirmed COVID-19 and only mild clinical symptoms [11,12].
CT is recommended in COVID-19 patients with moderate to severe symptoms at baseline and in case of progressing clinical symptoms [11]. Furthermore, CT has a role in estimation of disease severity of COVID-19 and to steer clinical management. For example, CT can provide an estimate of the proportion of unaffected, normally aerated lung, which has been linked to improved outcome [17]. A thorough analysis should be done regarding the potential benefit of the examination against the financial costs and exposure to ionizing radiation. Using modern CT scanners, however, the radiation dose, motion artifacts, as well as beam-hardening artifacts, can be reduced significantly [18].
Considering the variable sensitivity of RT-PCR, imaging may be of value in patients with a negative RT-PCR, but a high clinical suspicion of COVID-19 with moderate to severe symptoms. In such cases, imaging, particularly CT, may aid in differentiating between COVID-19 and alternative diagnoses. If imaging findings are suggestive of COVID-19, serial RT-PCR should be performed to confirm the diagnosis [11].
It is noteworthy that a negative chest CT does not exclude COVID-19, particularly if CT is performed in the first few days after the onset of symptoms [[19], [20], [21]].
In patients with RT-PCR-confirmed COVID-19 and moderate or severe symptoms, imaging can be used for risk stratification and to establish a baseline pulmonary status [11].
In COVID-19 patients with progressing clinical symptoms, imaging is helpful to diagnose or to rule out complications, such as bacterial superinfections, pulmonary embolism, or heart failure [11].
Given the low availability of PET/CT, its costs, the high radiation dose, and limited clinical consequences, the routine use of this modality in COVID-19 is not indicated. A retrospective case series of four patients who were investigated with 18F-FDG PET/CT in COVID-19 reported a high 18F-FDG uptake in areas of ground glass and consolidation [22].
3. Chest radiograph findings in COVD-19
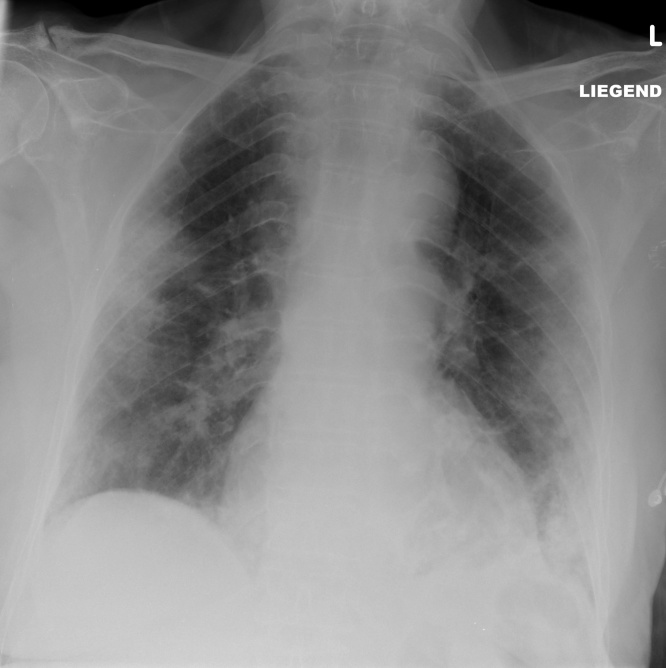
The most common findings on chest radiographs are multifocal ground-glass opacities and consolidation with a peripheral and lower lung zone predilection. Lung involvement may or may not be bilateral [23,24] (Fig. 1).
Fig. 1.
An 84-year-old female patient with dyspnea for two weeks, no fever, no cough. The chest radiograph shows ill-defined consolidations in the periphery of the mid- and lower-lung fields of both lungs. COVID-19 was confirmed by RT-PCR.
4. Chest ultrasound findings in COVD-19
As COVID-19 pneumonia has a predilection for the lung periphery, it can principally be assessed by transthoracic ultrasound. Transthoracic ultrasound may detect subpleural consolidations and variations of air and water content in lung tissue. It may show thickened irregular pleura and vertical reverberation artifacts that originate from the pleura (so-called “B-lines”) in a variety of patterns, including focal, multifocal, and confluent. In addition, it may show focal or multifocal consolidations, occasionally with mobile air bronchograms [25]. Pleural effusions are uncommon in COVID-19.
5. Chest CT findings in COVD-19
Although CT findings of COVID-19 are nonspecific, in the appropriate clinical setting with a high disease prevalence, CT findings in COVID-19 are highly suggestive of COVID-19. However, they do require RT-PCR confirmation.
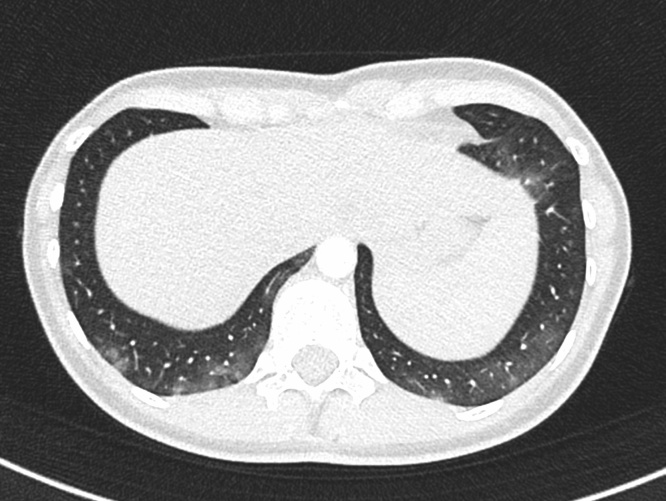
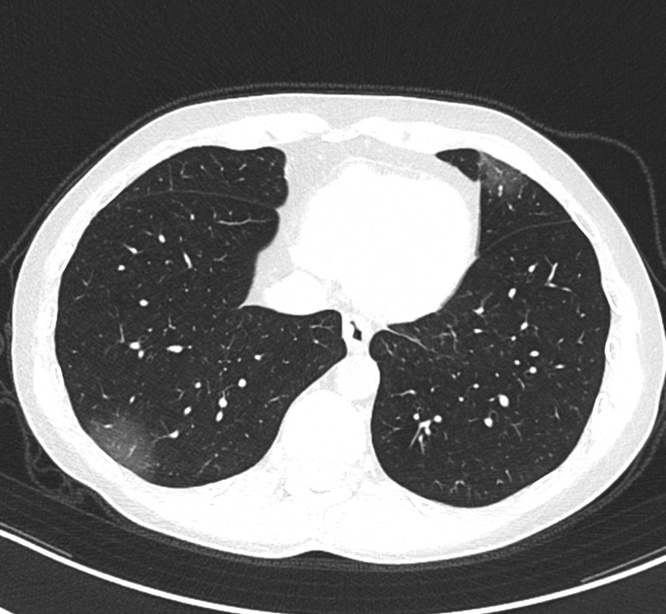
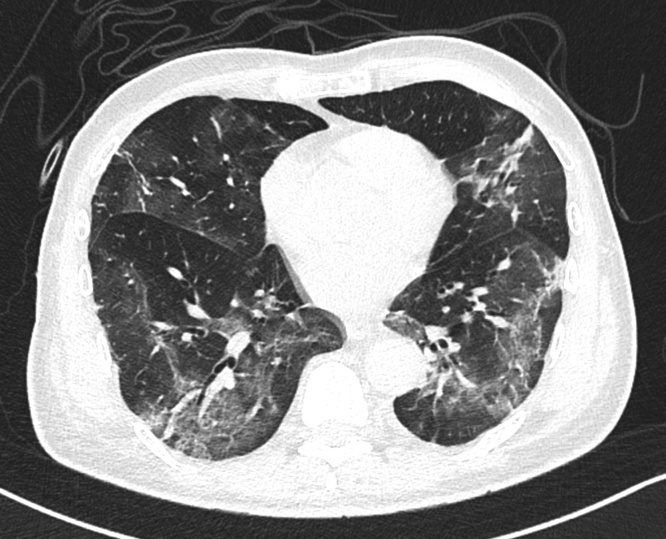
The most common initial CT findings in COVID-19 pneumonia are multifocal, patchy, or rounded ground-glass opacities that most frequently occur bilaterally and in the lung periphery with a basal predominance (Fig. 2, Fig. 3). Ground-glass opacities are observed in 88 % of the patients [26]. Those initial changes most likely correspond to pulmonary edema with hyaline membrane formation, indicating an early stage of diffuse alveolar damage [27].
Fig. 2.
A 27-year-old female patient with chest pain and chough. CT shows patchy areas of ground-glass in the periphery of both lower lobes. RT-PCR confirmed the suspicion of COVID-19.
Fig. 3.
A 47-year-old male patient with COVID-19 with fever and dry chough. CT shows rounded areas of ground-glass opacities in the periphery of both lungs.
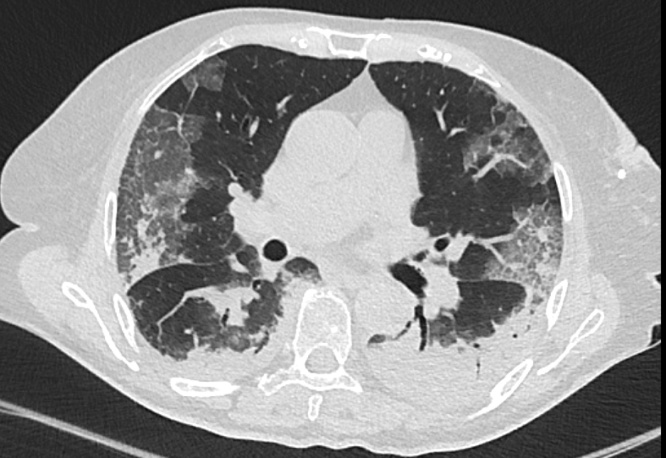
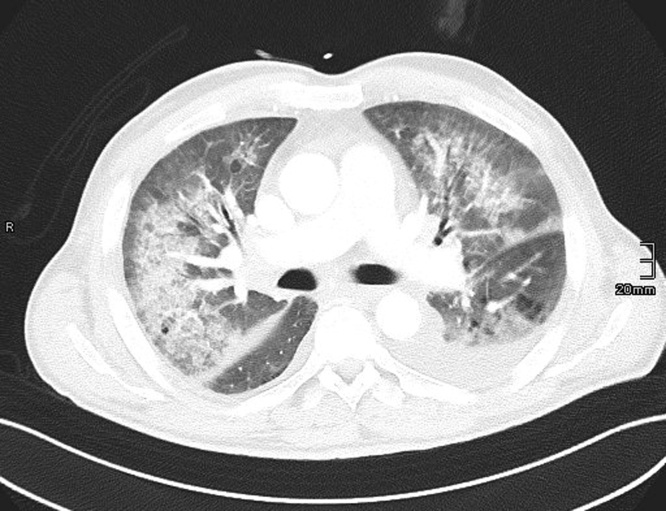
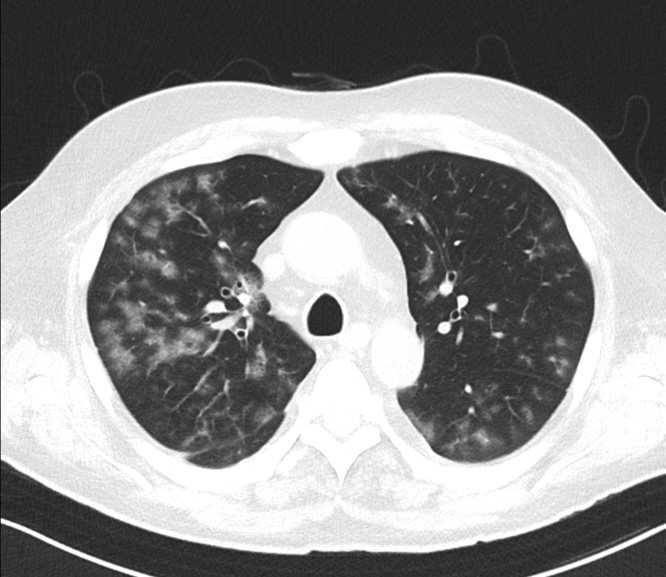
Consolidations are present in about one-third of the cases on the initial CT and occur with increasing frequency as the disease progresses (Fig. 4) [26]. In some patients, the consolidations are linear (referred to as “fibrous stripes” by some authors), most probably reflecting organizing pneumonia as a response to lung injury (Fig. 5) [28,29]. In some patients, the intra- and perilesional pulmonary vessels are engorged, indicating an increased perfusion of these areas [29,30].
Fig. 4.
A 60-year-old patient with deteriorating pulmonary function ten days after hospital admission and acute respiratory distress syndrome (ARDS). The CT scan depicts consolidations in the dorsal aspects of the lower lobes, frequently encountered in ARDS. Heterogeneous ground-glass opacifications in the nondependent lung are found in the subpleural peripheral lungs—a characteristic finding in COVID-19 cases. A combination of smooth, interlobular, septal thickening in areas of ground-glass attenuation, also described as the crazy-paving pattern, were also present and have been described in COVID-19 (encircled).
Fig. 5.
A 50-year-old male patient with a fever of up to 38 °C, cough, and dyspnea and negative RT-PCR. CT performed on the same day shows an organizing pneumonia type of appearance with peripheral arcades and linear opacities in both lungs, with a lower lobe and peripheral predominance. Repeated RT-PCR one day later confirmed SARS-CoV2 infection.
In addition to ground-glass opacities and consolidations, ground-glass superimposed with reticular abnormalities—termed crazy paving—and areas of ground-glass surrounded by a ring of consolidation—termed the reversed halo sign—have also been observed [[31], [32], [33], [34]].
In most cases, lesions are multifocal (70 %) and located in the lung periphery. Occasionally, they occur centrally in a bronchovascular distribution (12 %) or a combination of both (44 %–59 %) [20,35,36]. Typically, the lesions are found in both lungs with a slight predominance for the lower lobes [[31], [32], [33], [34],36].
In severe cases, CT shows diffuse heterogeneous consolidation with ground-glass opacities, air bronchograms, and bronchiectasis, presenting as “white lung” when most lung lobes are affected [37]. The presence of multiple bilateral lobular and subsegmental consolidation on CT were associated with an increased frequency of intensive care unit admission [38]. Patients also may occasionally present with thickening of interlobar septa and the bilateral pleura [39].
Pleural effusion, lung cavitation, lymphadenopathy, and calcification are not typically seen [30,40]. Centrilobular nodules with the tree-in-bud pattern are not distinctive and likely indicate other causes of pneumonia.
Over the course of the disease, GGOs were observed to be rapidly growing, demonstrating consolidation and a crazy-paving pattern as the disease progresses. The peak of CT morphological lung involvement occurs between day 9 and 13 after the initial onset of symptoms, followed by slow gradual clearing [41].
6. Differential diagnoses of COVID-19 pneumonia
Although the CT findings in COVID-19 pneumonia are characteristic, they lack specificity and require confirmation by RT-PCT. The most important differential diagnoses are other pulmonary infections, heart failure (Fig. 6), eosinophilic pneumonia, and organizing pneumonias of other etiologies.
Fig. 6.
A 59-year-old male patient with acute dyspnea and suspected COVID-19 pneumonia. CT shows minor, bilateral, pleural effusions, diffuse ground-glass opacities, and broncho-centric consolidations that spared the lung periphery. The CT findings were suspected to be more compatible with heart failure, which was confirmed clinically with multiple RT-PCR that was negative for SARS-CoV2.
Influenza virus pneumonias show unilateral or bilateral ground-glass opacities with multifocal areas of consolidation, which are predominantly peri-bronchovascular and subpleural in distribution [42]. RSV (Respiratory syncytial virus) infection exhibits multiple, centrilobular nodules with bronchial wall thickening (Fig. 7) [42]. Adenovirus infection shows multifocal consolidation with random ground-glass opacities and a predilection for lobar collapse that involves the right upper lobe (common in children) [42]. Severe acute respiratory syndrome coronavirus (SARS- 2003) and Middle East respiratory syndrome coronavirus (MERS-2012) manifests with peripheral, bilateral, focal or multifocal ground-glass opacities and consolidations [43]. Mycoplasma pneumonia frequently shows areas of ground-glass attenuation, patchy consolidations in a lobular distribution, and ill-defined centrilobular nodules with thickening of the bronchovascular bundles [44].
Fig. 7.
A 55-year-old male patient with progressive dyspnea after hematopoietic stem cell transplantation. CT shows multiple, centrilobular, nodular ground-glass opacities compatible with a respiratory syncytial virus (RSV) pneumonia, which was confirmed by PCR.
7. Complications in COVID-19
7.1. Bacterial superinfections
The presence of pleural effusions, multiple lung nodules, and lymphadenopathy on imaging may point toward a co-existing bacterial superinfection. Furthermore, tree-in-bud opacities or cavities are not typical and also point toward a superinfection [14].
7.2. Acute respiratory distress syndrome
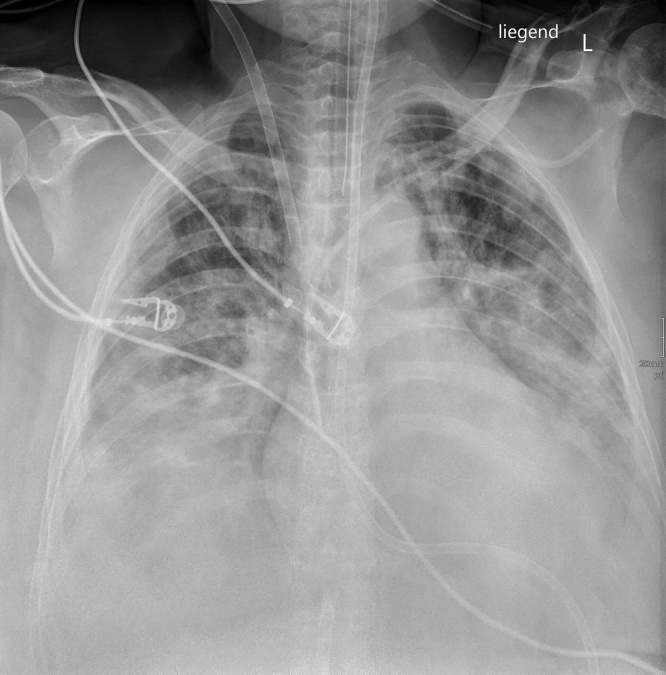
Acute respiratory distress syndrome (ARDS) describes the most severe complication of pulmonary impairment in the form of diffuse alveolar damage caused by SARS-CoV2. Clinically, patients present with significant arterial de-oxygenation and respiratory failure. Lung imaging, particularly CT, shows bilateral diffuse areas of ground-glass opacities with or without admixed consolidations (Fig. 8) [45].
Fig. 8.
A 50-year-old female patient with RT-PCR-confirmed COVID-19 pneumonia complicated by acute respiratory distress syndrome (ARDS). The chest radiograph shows confluent ill-defined consolidations in both lungs, with a predominance in the lower lung fields. The patient was intubated and on extra-corporeal membrane oxygenation (ECMO).
7.3. Cardiac involvement
Cardiac involvement as a complication of SARS-CoV-2 infection is rare [46]. Myocarditis due to viral insult ensues after focal or global myocardial inflammation and eventually leads to ventricular dysfunction [47]. The electrocardiography, laboratory tests, and wall-motion abnormalities found on echocardiographs in COVID-19 patients may resemble coronary heart disease and should prompt further evaluation using cardiac MRI, once obstructive coronary artery disease is excluded [46]. Cardiac MRI findings reveal diffuse edema and the slow gadolinium washout favors a diagnosis of acute myocarditis [47].
7.4. Pulmonary embolism
Pulmonary embolism appears to be a frequent complication in patients with COVID-19 pneumonia (Fig. 9). In a retrospective study that investigated 106 COVID-19 patients, a pulmonary embolism was detected in 30 % of the cases, which is much higher than the 1.3 % detection rate of pulmonary embolism detected in critically ill patients [48].
Fig. 9.
CT pulmonary angiography in a patient with RT-PCR-confirmed COVID-19 pneumonia shows a pulmonary embolism in the right anterior upper lobe artery (arrow).
7.5. CNS involvement
Acute necrotizing encephalopathy (ANE) has been previously reported as a rare complication of influenza and other viral infections. It is thought to be related to the intracranial cytokine storm that causes damage to the blood-brain barrier rather than a direct viral insult or para-infectious demyelination [49].
On imaging, ANE most characteristically shows symmetric, multifocal lesions with invariable thalamic involvement. On CT, these lesions are hypoattenuating, while MRI demonstrates a T2 FLAIR hyperintense signal with internal hemorrhage [49]. On postcontrast images, a ring of contrast enhancement may be visible [49].
8. Assessment schemes for COVID-19 pneumonia
To harmonize the reporting of CT findings and to give clinicians a categorical estimate of the probability of a COVID-19 pneumonia, several groups have developed assessment schemes for COVID-19 pneumonia [[50], [51], [52]]. In short, findings are categorized into typical findings of COVID-19, indeterminate findings, atypical findings (Covid-19 pneumonia unlikely, alternative diagnoses more likely) and normal [[50], [51], [52]]. In addition to categorization, imaging findings should also be roughly quantified into mild, moderate, and severe in order to allow a risk estimation [14,[50], [51], [52]].
9. Conclusion
Imaging plays an important role in the management of COVID-19 patients. To minimize the risk of infection of other patients and medical personnel, indications for imaging should be carefully weighed and tailored to the clinical situation and resources available. Typical CT features of COVID-19 pneumonia include multifocal bilateral GGOs, with or without patchy consolidations, prominent peripheral subpleural distribution, and posterior or lower lobe predilection. Thin-slice chest CT help to achieve a prompt diagnosis, guide clinical decision-making, and monitor disease progression, thus playing a critical role in the early prevention and control of COVID-19.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
All authors declare to have no conflict of interests regarding this article
References
- 1.Zu Z.Y., Jiang M.D., Xu P.P., Chen W., Ni Q.Q., Lu G.M., Zhang L.J. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology. 2020 doi: 10.1148/radiol.2020200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55(3) doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phelan A.L., Katz R., Gostin L.O. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA. 2020 doi: 10.1001/jama.2020.1097. [DOI] [PubMed] [Google Scholar]
- 4.Johns Hopkins University . 2020. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)https://coronavirus.jhu.edu/map.html (Accessed 21.4.2020 2020) [Google Scholar]
- 5.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin. Immunol. 2020 doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He F., Deng Y., Li W. Coronavirus disease 2019: what we know? J. Med. Virol. 2020 doi: 10.1002/jmv.25766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., Tao Q., Sun Z., Xia L. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim H., Hong H., Yoon S.H. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020 doi: 10.1148/radiol.2020201343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z., Yu J., Kang M., Song Y., Xia J., Guo Q., Song T., He J., Yen H.L., Peiris M., Wu J. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubin G.D., Ryerson C.J., Haramati L.B., Sverzellati N., Kanne J.P., Raoof S., Schluger N.W., Volpi A., Yim J.J., Martin I.B.K., Anderson D.J., Kong C., Altes T., Bush A., Desai S.R., Goldin J., Goo J.M., Humbert M., Inoue Y., Kauczor H.U., Luo F., Mazzone P.J., Prokop M., Remy-Jardin M., Richeldi L., Schaefer-Prokop C.M., Tomiyama N., Wells A.U., Leung A.N. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Radiology. 2020:201365. doi: 10.1148/radiol.2020201365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nair A., Rodrigues J.C.L., Hare S., Edey A., Devaraj A., Jacob J., Johnstone A., McStay R., Denton E., Robinson G. A British Society of Thoracic Imaging statement: considerations in designing local imaging diagnostic algorithms for the COVID-19 pandemic. Clin. Radiol. 2020;75(5):329–334. doi: 10.1016/j.crad.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American College of Radiology . 2020. ACR Recommendations for the Use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. (Accessed 22.3.2020 2020) [Google Scholar]
- 14.Revel M.P., Parkar A.P., Prosch H., Silva M., Sverzellati N., Gleeson F., Brady A. R. European Society of, I. the European Society of Thoracic, COVID-19 patients and the radiology department - advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI) Eur. Radiol. 2020 doi: 10.1007/s00330-020-06865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soldati G., Smargiassi A., Inchingolo R., Buonsenso D., Perrone T., Briganti D.F., Perlini S., Torri E., Mariani A., Mossolani E.E., Tursi F., Mento F., Demi L. Is There a Role for Lung Ultrasound During the COVID-19 Pandemic? J. Ultrasound Med. 2020 doi: 10.1002/jum.15284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim D.J., Jelic T., Woo M.Y., Heslop C., Olszynski P. Just the Facts: recommendations on point-of-care ultrasound use and machine infection control during the coronavirus disease 2019 pandemic. CJEM. 2020:1–5. doi: 10.1017/cem.2020.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colombi D., Bodini F.C., Petrini M., Maffi G., Morelli N., Milanese G., Silva M., Sverzellati N., Michieletti E. Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020201433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agostini A., Floridi C., Borgheresi A., Badaloni M., Esposto Pirani P., Terilli F., Ottaviani L., Giovagnoni A. Proposal of a low-dose, long-pitch, dual-source chest CT protocol on third-generation dual-source CT using a tin filter for spectral shaping at 100 kVp for CoronaVirus Disease 2019 (COVID-19) patients: a feasibility study. Radiol. Med. 2020;125(4):365–373. doi: 10.1007/s11547-020-01179-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N., Diao K., Lin B., Zhu X., Li K., Li S., Shan H., Jacobi A., Chung M. Chest CT findings in coronavirus Disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiong Y., Sun D., Liu Y., Fan Y., Zhao L., Li X., Zhu W. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest. Radiol. 2020 doi: 10.1097/RLI.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pan F., Ye T., Sun P., Gui S., Liang B., Li L., Zheng D., Wang J., Hesketh R.L., Yang L., Zheng C. Time Course of Lung Changes On Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19) Pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qin C., Liu F., Yen T.C., Lan X. (18)F-FDG PET/CT findings of COVID-19: a series of four highly suspected cases. Eur. J. Nucl. Med. Mol. Imaging. 2020;47(5):1281–1286. doi: 10.1007/s00259-020-04734-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong H.Y.F., Lam H.Y.S., Fong A.H., Leung S.T., Chin T.W., Lo C.S.Y., Lui M.M., Lee J.C.Y., Chiu K.W., Chung T., Lee E.Y.P., Wan E.Y.F., Hung F.N.I., Lam T.P.W., Kuo M., Ng M.Y. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019 doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoon S.H., Lee K.H., Kim J.Y., Lee Y.K., Ko H., Kim K.H., Park C.M., Kim Y.H. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J. Radiol. 2020;21(4):494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peng Q.Y., Wang X.T., Zhang L.N. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am. J. Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 27.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F.S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hani C., Trieu N.H., Saab I., Dangeard S., Bennani S., Chassagnon G., Revel M.P. COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn. Interv. Imaging. 2020 doi: 10.1016/j.diii.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lomoro P., Verde F., Zerboni F., Simonetti I., Borghi C., Fachinetti C., Natalizi A., Martegani A. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur. J. Radiol. Open. 2020;7 doi: 10.1016/j.ejro.2020.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye Z., Zhang Y., Wang Y., Huang Z., Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur. Radiol. 2020 doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caruso D., Zerunian M., Polici M., Pucciarelli F., Polidori T., Rucci C., Guido G., Bracci B., de Dominicis C., Laghi A. Chest CT features of COVID-19 in Rome, Italy. Radiology. 2020 doi: 10.1148/radiol.2020201237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen R., Chen J., Meng Q.T. Chest computed tomography images of early coronavirus disease (COVID-19) Can. J. Anaesth. 2020 doi: 10.1007/s12630-020-01625-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu J., Wu X., Zeng W., Guo D., Fang Z., Chen L., Huang H., Li C. Chest CT Findings in Patients With Coronavirus Disease 2019 and Its Relationship With Clinical Features. Invest. Radiol. 2020;55(5):257–261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li K., Wu J., Wu F., Guo D., Chen L., Fang Z., Li C. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest. Radiol. 2020 doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am. J. Roentgenol. 2020;214(5):1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 36.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J., Fan Y., Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu K.C., Xu P., Lv W.F., Qiu X.H., Yao J.L., Gu J.F., Wei W. CT manifestations of coronavirus disease-2019: a retrospective analysis of 73 cases by disease severity. Eur. J. Radiol. 2020;126 doi: 10.1016/j.ejrad.2020.108941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen Z., Fan H., Cai J., Li Y., Wu B., Hou Y., Xu S., Zhou F., Liu Y., Xuan W., Hu H., Sun J. High-resolution computed tomography manifestations of COVID-19 infections in patients of different ages. Eur. J. Radiol. 2020;126 doi: 10.1016/j.ejrad.2020.108972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ng M.-Y., Lee E.Y., Yang J., Yang F., Li X., Wang H., Lui M.M.-s., Lo C.S.-Y., Leung B., Khong P.-L. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol. Cardiothorac. Imaging. 2020;2(1) doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kanne J.P., Little B.P., Chung J.H., Elicker B.M., Ketai L.H. Essentials for radiologists on COVID-19: an update-radiology scientific expert panel. Radiology. 2020 doi: 10.1148/radiol.2020200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koo H.J., Lim S., Choe J., Choi S.H., Sung H., Do K.H. Radiographic and CT features of viral pneumonia. Radiographics. 2018;38(3):719–739. doi: 10.1148/rg.2018170048. [DOI] [PubMed] [Google Scholar]
- 43.Hosseiny M., Kooraki S., Gholamrezanezhad A., Reddy S., Myers L. Radiology Perspective of Coronavirus Disease 2019 (COVID-19): Lessons From Severe Acute Respiratory Syndrome and Middle East Respiratory Syndrome. AJR Am. J. Roentgenol. 2020:1–5. doi: 10.2214/AJR.20.22969. [DOI] [PubMed] [Google Scholar]
- 44.Reittner P., Muller N.L., Heyneman L., Johkoh T., Park J.S., Lee K.S., Honda O., Tomiyama N. Mycoplasma pneumoniae pneumonia: radiographic and high-resolution CT features in 28 patients. AJR Am. J. Roentgenol. 2000;174(1):37–41. doi: 10.2214/ajr.174.1.1740037. [DOI] [PubMed] [Google Scholar]
- 45.Tang X., Du R., Wang R., Cao T., Guan L., Yang C., Zhu Q., Hu M., Li X., Li Y., Liang L., Tong Z., Sun B., Peng P., Shi H. Comparison of hospitalized patients with ARDS caused by COVID-19 and H1N1. Chest. 2020 doi: 10.1016/j.chest.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system, Nature reviews. Cardiology. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasoni D., Cani D.S., Cerini M., Farina D., Gavazzi E., Maroldi R., Adamo M., Ammirati E., Sinagra G., Lombardi C.M., Metra M. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leonard-Lorant I., Delabranche X., Severac F., Helms J., Pauzet C., Collange O., Schneider F., Labani A., Bilbault P., Moliere S., Leyendecker P., Roy C., Ohana M. Acute pulmonary embolism in COVID-19 patients on CT angiography and relationship to D-Dimer levels. Radiology. 2020 doi: 10.1148/radiol.2020201561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Prokop M., van Everdingen W., van Rees Vellinga T., Quarles van Ufford J., Stoger L., Beenen L., Geurts B., Gietema H., Krdzalic J., Schaefer-Prokop C., van Ginneken B., Brink M., C.-S.R.W.G.o.t.D.R. Society CO-RADS - A categorical CT assessment scheme for patients with suspected COVID-19: definition and evaluation. Radiology. 2020 doi: 10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sverzellati N., Milanese G., Milone F., Balbi M., Ledda R.E., Silva M. Integrated radiologic algorithm for COVID-19 pandemic. J. Thorac. Imaging. 2020 doi: 10.1097/RTI.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simpson S., Kay F.U., Abbara S., Bhalla S., Chung J.H., Chung M., Henry T.S., Kanne J.P., Kligerman S., Ko J.P., Litt H. Radiological society of north america expert consensus statement on reporting chest ct findings related to covid-19. endorsed by the society of thoracic radiology, the American College of Radiology, and RSNA. J. Thorac. Imaging. 2020 doi: 10.1097/RTI.0000000000000524. [DOI] [PMC free article] [PubMed] [Google Scholar]