1. COVID-19 pandemic
The new coronavirus whose clinical entity has been named COVID-19 (Coronavirus disease 2019) began in the province of Wuhan, China in late 2019 and has inexorably expanded globally in the form of a pandemic, also affecting our country.
The causative agent of this new respiratory condition was identified as a new coronavirus (nCoV) by deep sequencing and etiological investigations by different independent laboratories in China and on January 12, 2020, the World Health Organization temporarily named the new virus as new coronavirus 2019 (2019 – nCoV) and its clinical picture COVID-19. The International Committee on Virus Taxonomy has announced that the official classification of the new coronavirus is known as Coronavirus 2 for severe acute respiratory syndrome, SARS-CoV-2 [1].
The lines of defense against this new virus for critically ill patients begin with medical intensive care units, followed by surgical intensive care units. And the burn intensive care units have turned into an important back up for the admission of non burned critical ill patients.
As we can see through the last report published in the journal, the strategy of most of the hospital in Asia, Europe and North America has been to delimitate clean and COVID-19 positive units. In this planning, most of the burn units has been kept clean of COVID-19 positive patients, admitting negative ones from different pathologies other than burns. When possible, burned patients are treated on an outpatients basis, with wound dressing that could be change every 3–4 days, until the wound is healed. In COVID-19 positive burned patients, if they are severely burned and is an emergency to admit and treat, they have been admitted in COVID-19 positive ICU, and if they are not that severe, ambulatory regimen with wound dressing is performed until RT- PCR negativization and admission into a COVID-19 negative area to perform the required surgery [2].
2. Chile, burns and COVID-19
According to the last population census of 2017, Chile has a population of 17,574,003 inhabitants, with a higher density in the central area of the country [3].
Chile has a mixed health care system; public, private, mutual insurance companies for work related accidents and armed forces hospitals.
The public health system provides services to more than 75% of the beneficiaries in the country, coincidentally the population with the least economic resources and the most vulnerable.
To reduce health inequities, in 2005 the Explicit Health Guarantees (from the spanish Garantías Explícitas en Salud) law was implemented to provide opportunities in access, treatment and financial protection to pathologies that represent a greater risk to public health.
In 2007, problem No. 55, Management of Major Burns Adults and Pediatric patients, was incorporated into the GES benefits. The burn unit of “Dr. Alejandro del Río” Hospital de Urgencia Asistencia Pública (HUAP) in the capital city Santiago de Chile, is called the National Reference Center for Major Adults Burns for the public health system.
The first positive case for COVID-19 in Chile, was confirmed on March 3, a person who arrived from Southeast Asia. On March 18, a state of catastrophe was decreed for 90 days, and different sanitary, social and economic measures have been taken. Quarantines of infected patients and contacts, preventive confinement in different cities of Chile and sanitary cords.
From the first cases, the outbreak is ongoing, with a sustained increase in infections and an increase in deaths attributed to this cause. At April 27, the Ministry of Health reports that nearly 5000 CPR are reported daily with a cumulative of 161,235, 13,813 positive cases and 198 deaths, 67.68% over 70 years of age. 56.9% of confirmed cases are in the Metropolitan Region [4]. The Chilean Society of Intensive Medicine, at the same date, reports that of a total of 1549 beds in the Intensive Care Unit in the country, there is a current occupation of 65% and 41% occupancy of mechanical ventilators available [5]. On April 15, there were 743 infected health workers [4].
Throughout the burns units in the country, including pediatric and adults, public and private, only the HUAP Reference Center has admitted positive COVID-19 severely burned patients.
3. HUAP National Reference Center for large burned adults
“Dr. Alejandro Del Río” Hospital de Urgencia Asistencia Pública was conceived in the early 1900s as a permanent center for emergency and trauma in the capital city of Santiago de Chile. This concept has been maintained over time, being the only hospital in the country with this identity, serving an assigned population of more than 1,000,000 people in the capital, it is also a national referral center for polytrauma and burned people. The hospital complex has two buildings; an old Tower (1967) and the recently inaugurated Valech Tower (2019), with new emergency area, critical unit and operating rooms. Due to the contingency related to the coronavirus pandemic, a special area was adapted only to be respiratory COVID-19 area. Located in the HUAP old building, the national reference center for adults major burns (over 15 years old), has a potentially beneficiary population of 11,000,000 inhabitants. With an occupation of more than 90% permanently, about 200 cases are treated per year. In 2018, the global mortality was 10% and the LD50% 57% [6].
It is a closed service, it only receives patients referred from the different hospitals in Chile and who meet the criteria defined for severely burned patients in the ministerial guidelines. There is no spontaneous emergency consultation. Outpatient consultation just for post-discharge control and follow-up of rehabilitation and sequelaes. The unit has 22 beds; 10 intensive critical care isolated beds, 8 intermediate care beds, 1 middle complexity isolation bed and 4 beds in general ward an exclusive operating theater and 127 health care workers in total.
4. HUAP Burn Unit strategic approach during COVID-19
4.1. Admission of patients
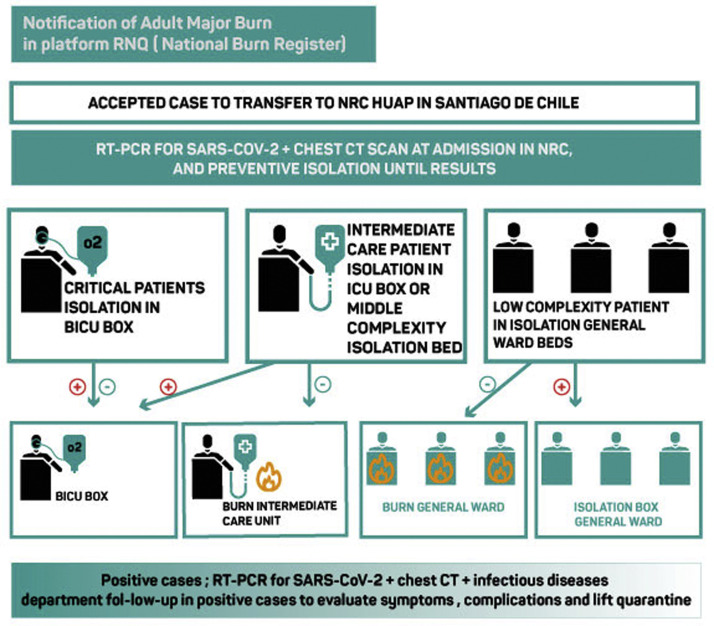
All admissions at the Burn Unit is handled as suspected COVID-19 regardless the place of origin (hospital, home or transferred from another floor within the institution). A RT- PCR for SARS-CoV-2 plus a chest CT scan is requested. The patient is remained as suspect case in the corresponding isolation bed awaiting the result (Fig. 1 ).
Fig. 1.
Screening algorithm and infectious diseases department evaluation.
The discharge post control, follow-up outpatient clinic and burn scar laser clinic were canceled and replaced with telemedicine as much as possible.
4.2. ICU area air and air conditioning replacement
Due to safety regulations and to avoid the potential spread of aerosols with the SARS-CoV-2 virus from the units with COVID-19 positive patients, the intensive care unit area must operate at Negative Pressure inside the 10 boxes, with a replacement of air 10 times per hour.
4.3. Workforce management, safety and surveillance
The most of the workforce has a call schedule that has no need to be modified. For the 13 staff surgeons, we divided them in two groups, to maintain surgeons in reserve in case of illness or preventive quarantines. After the first COVID-19 positive patient transferred to the unit (index case), without diagnosis at that moment, we had to do RT-PCR screening to every patient and health care worker inside the unit. We found 5 positive asymptomatic cases; 3 chronic burned patients, one subacute patient and 2 health workers. The patients were already in isolated ICU beds, and the workers were sending home to strict isolation quarantine, with the proper follow up of respiratory symptoms.
After this index case we established strict guidelines in the correct use of Personal Protective Equipment (PPE). Daily training in the use, removal and re-use of PPE is carried out by continuity nurse and is suggested to work in pairs to carry out a cross supervision to detect inadvertent contamination.
4.4. Surgical activity
All burned patients, whether COVID-19 positive, negative or suspected, will undergo surgery in the operating room of the unit. Two or three surgeries will be scheduled per day. Each surgery must last a maximum of 2 h. Prolonged surgeries such as MEEK or Microsurgery should be analyzed on a case-by-case basis according to the patient's conditions and the epidemiological situation of the unit.
5. Outcomes in COVID-19 severely burned patients
At April 27, we have had 6 COVID-19 positive patients in the unit (Table 1 ).
Table 1.
Socio demographic features.
| Sex | |
| Male | 3 (50%) |
| Female | 3 (50%) |
| age (years) | 32.16 (26–42) |
| %TBSA | 42.25% (27–59 |
| % partial thickness | 33% |
| % full thickness | 6.5% |
| ABSI | 7.66 (4–11) |
| Garcés Index (Chilean pronostic index) | 135.67 (85–221). Critical |
| Smoke inhalation injury | 50% (3) |
| Cause of burn wound | |
| fire | 5 (83.3%) |
| scald | 1 |
| Time from burn accident and transfer to NRC (days) | 4.6 (1–9) |
The first case (index case) was detected on April 1. This patient was transferred from the north of the country without previous RT- PCR for SARS-CoV-2. After confirmation of the diagnosis we had to forced extreme measures such as preventive quarantine for the contacts and RT-PCR test for all patients and service health workers, as we describe before.
In this general screening inside the unit, we found 4 more positive cases, among chronic and subacute burned patients, with prolonged mechanical ventilation (3 tracheostomies) but without any conflict in definitive burn wound coverage. After this event and under the new strict protocols of RT- PCR and chest TC scan at the admission time, we have found just one extra positive patient transferred from another hospital in Santiago and no cross contamination between COVID-19 positive and negative burn patients.
We can divide this cohort in two main groups. The chronic and subacute one (4 patients), who had positive RT-PCR for SARS-CoV-2, but during more than 3 weeks of follow-up, did not present any symptom or complication related with the coronavirus. They evolved as asymptomatic patients. In the second group (acute burns), with a time relapse in between the burn accident and the positive RT-PCR for SARS-CoV-2 of 9 days the manifestation of the disease was different. They were connected to invasive mechanical ventilation because of smoke inhalation injury and the burn SIRS and after that they evolved with COVID-19 pneumonia (Chest CT findings), but there were no signs of acute distress respiratory syndrome. Actually, during 3 weeks of follow-up the ventilation parameters never got worse and non prone position was needed for this reason. Also we have been able to perform our surgical protocol of early debridement and transient or definitive coverage as usual. When we did skin grafting we did not have any surgical complication during the surgery or in the postoperative time, with no complications in graft taking or donor sites (Table 2 ).
Table 2.
COVID-19 patients outcomes until April 24.
| Time from burn accident and RT-PCR SARS-CoV 2 positive | |
| Chronic burn group (4 patients) | 53.75 days |
| Acute burn group (2 patients) | 9 days |
| First RT-PCR SARS-CoV 2 | |
| Positive | 5 (83.3%) |
| Negative | 1 |
| First chest CT scan | |
| Positive | 2 |
| Negative | 4 |
| Invasive mechanical ventilation | 4 |
| Traqueostomy (chronic group) | 3 |
| Medical complication | – |
| COVID-19 pneumonia | 2 |
| Prone position ventilation | 0 |
| Total surgeries after COVID-19 diagnosis | 10 |
| Surgical debridement | 5 |
| Skin grafts | 5 |
| MEEK | 0 |
| Flaps | 0 |
| Microsurgery | 0 |
| Surgical complication | |
| Graft take | >95% |
| Donor site complication | 0 |
| Mortality | 0 |
| Discharge | 1 |
From this small cohort of severely burned COVID-19 patients, today we had one discharge and 5 remains in ICU; 3 patients with tracheostomy and mechanical ventilation and 2 patients with successful weaning.
We can not make any conclusion with this data, but in our early experience, we could suggest that the surgical treatment in severely burned patients does not need to wait until negative RT-PCR. We think that the delay in the debridement and definite skin graft could be worse for the prognosis of the patient, taking into account the behavior of COVID-19 in this cohort, because of the extremely intense systemic inflammatory syndrome associated to the severely burned and the high risk of cutaneous secondary sepsis, that could jeopardize any opportunity of a successful outcome in super-infections, a common situation in this setting, and now, COVID-19, is another one in the list.
Conflict of interest
There are no declarations or conflicts of interest.
References
- 1.Chen Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barret J. Burn center function during the COVID-19 pandemic: an international multi-center report of strategy and experience. Burns. 2020 doi: 10.1016/j.burns.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.www.deis.cl
- 4.https://www.gob.cl/coronavirus/cifrasoficiales/
- 5.https://www.medicina-intensiva.cl/site/post_covid.php?id=25
- 6.Merino C.B., Urzua C.S., Diez C.S., Irarrazabal C.A., Macho R.M. Congreso de Cirujanos de Chile; 2018. Aplicación del registro nacional de quemados (RNQ); perfil clínico y demográfico de los pacientes derivados al Hospital de Urgencia asistencia Publica (HUAP) [Google Scholar]