Abstract
Background
Charcot neuroarthropathy is a complex condition characterised by progressive deformity, limited treatment options and a high amputation rate. Surgical reconstruction of Charcot foot has been proposed as a method to preserve the foot. However, limited information exists on the different methods of reconstruction available, their outcomes and complications.
Methods
We systematically analysed published data from Jan 1993 to Dec 2018 to assess methods of fixation and associated outcomes for the surgical reconstruction in Charcot neuroarthropathy. Statistical analyses were undertaken to determine the amputation rates, return to ambulation and complications associated with these techniques.
Results
A total of 1116 feet (1089 patients) were reported to have undergone reconstruction with significant heterogeneity in patient selection. Of these, 726 (65%) were reported to undergo internal fixation, 346 feet (31%) external fixation and 44 (4%) undergoing simultaneous internal and external fixation. No single technique demonstrated a significant benefit over the other. Overall, the bone fusion rate was 86.1%. Complications directly attributable to the technique employed were noted in 36% of individuals. The reported post-reconstruction amputation rate was only 5.5% with 91% apparently returning to ambulation.
Conclusions
Although no preferential method of fixation was identified, we find that the current options for surgical reconstruction could offer limb salvage with a low amputation risk in a highly selected population. However, the lack of controlled studies, inconsistent reporting of outcomes and heterogeneity of patient selection mean that the quality of evidence is low.
Keywords: Charcot, Neuroarthropathy, Neuropathy, Diabetes, Surgical reconstruction
Highlights
-
•
A number of methods are used (internal fixation, external fixation and combined) for surgical reconstruction in Charcot Foot.
-
•
Most studies are case series from specialist centres with wide variation in patient selection and lacking controlled studies.
-
•
Studies report improved patient recorded outcome measures with surgical intervention.
-
•
Amputation rates following surgical reconstruction are reportedly low.
-
•
Post-operative complication rates are conspicuously high reflecting the complex surgical nature in these patients.
1. Introduction
Charcot neuroarthropathy often leads to progressive deformity and ulceration. This ultimately results in loss of normal foot architecture causing significant patient morbidity and decline in the patient’s American Orthopaedic Foot and Ankle Score (AOFAS).1 Although the exact pathophysiology is unknown, it is thought that sensory and motor neuropathy causing loss of protective sensation and muscular atrophy leads to repetitive microtrauma in the weight bearing joints, predominantly in the foot and ankle. Autonomic neuropathy can increase the bone perfusion leading to osteopenia thereby increasing the risk of fracture.2,3
Different strategies have been implemented to manage this complex condition. During the acute phase, the mainstay of therapy continues to be offloading in a total contact cast to prevent deformity followed by a brace or custom orthoses once the condition has become quiescent. The ultimate aim is to preserve the soft tissue envelope by preventing or limiting any bony deformity that may occur.4,5 However, due to the progressive nature of the disease, ulcer development is common, with reported rates of as high as 50%.6
Common surgical interventions in diabetic foot surgery typically include ulcer debridement, exostectomy of bone prominences, deformity correction and minor and major amputations. The latter is often considered when conservative strategies fail and has its own limitations, including unpredictable rehabilitation. As such the overall rate of minor and major amputation in this group is 3.3–11 per 1000 patients and ulceration precedes in 70%–84% of these lower extremity amputations.7 Major amputation among patient with diabetes is also known to carry a high mortality rate, of up to of 70% at 5 years.7,8 Within these statistics we recognise that there will be a group of patients with severe deformity that will come to amputation, if reconstruction is not considered.
Recently, there has been renewed interest in the surgical reconstruction of the deformed diabetic foot. A variety of techniques have been described to obtain a plantigrade foot that can weight bear in a shoe or other orthotic device, prevent ulceration and major amputation and improve the function and quality of life. Reported surgical outcomes are sparse, and often intermingled with severe traumatic arthritis or other conditions resulting in severe foot deformity, which makes interpretation difficult.9
The purpose of this study was to systematically review the published literature on surgical reconstruction of the mid and hind-foot in Charcot neuropathy and determine the impact on key outcomes.
2. Methods
A systematic review of publicly available evidence from Jan 1993 to Dec 2018 using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines with a PRISMA checklist was conducted.
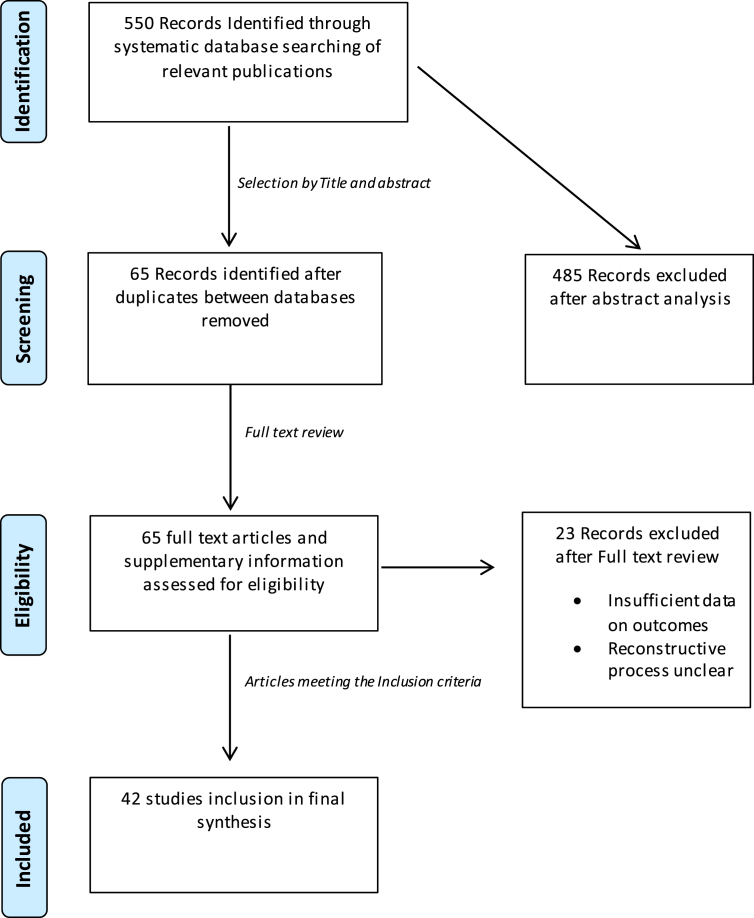
The literature search was completed by JH, TH and RA and incorporated Medline, Pubmed, Embase, Cochrane library and Proquest search engine, CINAHL (Cumulative Index to Nursing and Allied Health Literature), and Cochrane Central Register of Controlled Trials. The references in the retrieved articles were checked to identify further relevant publications. In the final analysis published proceedings of scientific meetings and conferences were reviewed, along with a manual search of various current orthopaedic and trauma textbooks (Fig. 1)
Fig. 1.
Study selection flow diagram. This outlines the filtering process from literature search to study inclusion.
The key terms identified were defined using the PICOT framework (population, intervention, comparison, outcome, time frame). A range of keywords were included: Charcot, neuroarthropathy/arthropathy, Neurogenic, Reconstruction, Surgery. The search was restricted to the articles published in English. A further set of key words within the concept were then identified, such as ankle, hind foot, foot, fore-foot, and mid-foot. Wildcards and truncation symbols were used as appropriate (i.e. Surg∗ to include surgery, surgical etc.) across different databases.
Inclusion criteria included operative (surgical) fixation with application of external fixation (external fixator, circular frame, Ilizarov frame, Taylor Spatial Frame), and internal fixation (hind foot nail, hind foot or mid foot plate, mid foot beams, screws). Exclusion criteria included all non-English language studies, pure biomechanical studies, single patient case reports, mixed studies that included non-Charcot cases, simple surgical interventions such as debridement or exostectomy, novel technique studies, perception-based studies, cadaveric studies, scientific meeting abstracts/proceedings, systematic reviews and meta-analyses with mixed pathology studies.
Evidence Levels I, II, III, and IV were deemed inclusive (per the Oxford Centre for Evidence-Based Medicine) if published in the English language. The authors extracted data from the individual studies (if stated) and included: number of patients, number of feet, number of patients with diabetes and type, age, duration of follow-up, body mass index (BMI), fixation type and site of fusion. In the event of disagreement on study inclusion the senior author (RA) made the final decision.
Outcomes of interest included quality of life, foot function score, complications, radiographic measurements, patient reported outcomes, number of amputations, ability to weight bear, time to weight bear and number of persistent ulcers and associated surgical complications. Other factors including study country of origin, author conflict of interest (COI), and single-centre versus multi-centre study design were assessed. All extracted data was assessed by IR, & RA and manuscript preparation was conducted by TH, JH, IR, PV, VK and RA.
2.1. Statistical analysis
Statistical-analysis was undertaken (RF, RA) to determine the significance of proportions or percentage results of the interventions. The primary outcomes chosen for this systematic review were amputation rates and return to ambulation. Secondary outcomes included superficial and deep infection, re-ulceration, fusion rates, revision surgery and requirement for metalwork removal.
Proportions were calculated as the number of patients with each outcome divided by the total number of patients in each study. Where possible, a meta-analysis was performed using a random effects model to derive estimated proportions for the overall outcomes of interest as per DerSimonian & Laird’s method.75
A Funnel plot was produced to assess for inherent bias and a random effects analysis was chosen due to the heterogeneity of studies, following a comparison with a fixed effects model to exclude bias of smaller studies. As the majority of studies did not have a control this analysis is centred around 1 rather than 0–1 (or 0%–100%). Heterogeneity was assessed using the chi-square (Q) test and the total percentage of this heterogeneity quantified with the I2 value set at 2. Subgroup analysis was performed for each outcome based on the operative technique selected for joint reconstruction. We defined statistical significance at the 5% (p ≤ 0.05) level. Statistical analysis was carried out using MedCalc version 17.4 (MedCalc Software, Ostend, Belgium).
3. Results
3.1. Studies
Five hundred and fifty studies (n = 550) were identified with the initial search criteria. Reviewing titles and abstracts only identified 65 for full article review and of these 42 studies met the full inclusion criteria and underwent further analysis.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47
All studies were retrospective, with no level 1 randomised controlled trials. All were classified as levels of clinical evidence 3 or 4 except for Grant et al., which is reported as level 2.18 Publication numbers increased from 1993; the mean number of feet reported every year rose from 20.3 to 65 during the 5-year period 2010–15.
3.2. Patient numbers, demographics and pathology
A total of 1089 patients were reported to have undergone reconstruction in 1116 feet (see Table 1). The majority were diabetic; only 86 patients had Charcot neuroarthropathy from another cause. The mean age of patients undergoing reconstruction was 57.5 (26–82) years (n = 38) and the mean BMI was 3521, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52 (n = 13).11,12,18,19,23,48,49
Table 1.
A statistical description of the reports (N = 42) including number of patients, paper origin demographic features of the patients including age, BMI, the duration of follow-up, and operative fixation used.
| Author, Year, Country | No. of Participants | No. of Feet | No. Diabetic | Age | Age Range | BMI | Mean F/U (Months) | Fixation Type |
|---|---|---|---|---|---|---|---|---|
| Papa et al., 1993, USA | 29 | 29 | 29 | 56 | 28–72 | Nr | 42 (14–68) | IMN 25 Ex Fix 4 |
| Early et al., 1996, USA | 18 | 21 | 18 | 58 | (38–72) | Nr | 28 (6–84) | Screw Fusion |
| Pinzur et al., 1997, USA | 20 | 21 | 19 | 56.3 | (28–68) | Nr | 20 (3–31) | IMN |
| Sammarco et al., 1998, USA | 26 | 27 | 21 | 56.9 | (32–72) | Nr | 27.9 (18–51) | Midfoot Fusion Bolt |
| Stone et al., 2000, Canada | 10 | 10 | 10 | 63 | (51−9) | Nr | 24 (12–37) | Plates and Screws, BG |
| Simon et al., 2000, USA | 14 | 14 | 14 | 48.2 | (SD ±9.5) | Nr | 41 (25.3–77.3) | Plates and Screws, BG |
| Farber et al., 2002, USA | 11 | 11 | 10 | 55 | (41–66) | Nr | 24 (12–49) | Ex Fix |
| Rooney et al., 2002, Austrailia | 36 | 43 | 26 | 58 | (33–74) | Nr | 31 (9–120) | Screw Fusion |
| Cooper et al., 2003, USA | 83 | 83 | 83 | 56.6 | Nr | 15 | Ex Fix | |
| Pinzur et al., 2005, USA | 9 | 9 | 9 | 52 | (38–72) | Nr | 32 (30–35) | IMN |
| Caravaggi et al., 2006, Italy | 14 | 14 | 14 | 58 | (SD12) | Nr | 18 (5–20) | IMN |
| Fabrin et al., 2007, Denmark | 11 | 12 | 11 | 61 | (43–71) | Nr | 48 (10–102) | Ex Fix |
| Pinzur et al., 2007, USA | 26 | 26 | 26 | 56.6 | (36-75) | 38.31 ± 12.51 | min 1 year | Ex Fix |
| Paola et al., 2007, Italy | 18 | 18 | 18 | 65 | (SD ±9) | Nr | 14 (5–35) | IMN |
| Hockenbury et al., 2007, USA | 10 | 10 | 9 | 59.3 | (50–69) | Nr | 21 (7–58) | IMN with implantable bone growth stimulator |
| Pinzur et al., 2007, USA | 51 | 51 | 51 | 58 | (SD 9.92) | Nr | 33.22 (SD 21.25) | Plates and Screws |
| Ayoub, 2008, Egypt | 17 | 17 | 17 | 61.6 | (57–69) | Nr | 26 (12–48) | Screw Fusion |
| El-Gafary et al., 2009, Egypt | 20 | 20 | 18 | 30 | (21–50) | Nr | 20 (12–30) | Ex Fix |
| Pinzur et al., 2009, USA | 44 | 46 | 44 | 54.9 | ±10.4 | 38.0 ± 9.7 | 26.2 ± 12.2 | Ex Fix |
| Paola et al., 2009, Italy | 45 | 45 | 45 | 65.3 | (SD ±8.9) | 36.58 (±9.81) | not stated | Ex Fix |
| Assal et al., 2009, Switzerland | 15 | 15 | 15 | 55 | (34–70) | Nr | 42 (24–72) | Plates and Screws |
| Mittlmeier et al., 2009, Germany | 22 | 26 | 22 | 56.2 | (29–73) | Nr | 31 (6–84) | Plates and Screws |
| Sammarco et al., 2009, USA | 22 | 22 | 19 | 59.4 | (45–81) | Nr | 52 (25–137) | Screw Fusion |
| Cinar et al., 2010, Turkey | 4 | 4 | 4 | 63 | (53–70) | Nr | 24 (12–35) | Blade Plate |
| Lamm et al., 2010, USA | 4 | 8 | 11 | 61 | (41–79) | 33.6± 13 | 22 (6/36) | Ex Fix and Screws |
| Grant et al., 2011, USA | 70 | 71 | 69 | 56.1 | (29–78) | 33.1 (21.3–51.2) | 31 (3–92) | 29 medial & Lateral beaming, 18 medial & Lateral beaming & subtalar arthrodesis, 11 medial & lateral column beaming with subtalar fusion, 12 medial column beaming, 1 medial column beaming combined with subtalar arthrodesis |
| DeVries et al., 2012, USA | 52 | 52 | 45 | 59.4 | Nail (38–85) Ex fix (35–65) | IMN 34.1 (18.5–46.6) Ex Fix 35.5 (19.9–54.9) | 24 (0–72.25) | 45 IMN, 7 Ex Fix |
| Pinzur et al., 2012, USA | 73 | 73 | 73 | 57.9 | (31–76) | 36.9 (21.8–60.9) | min 1 year | Ex Fix |
| Caravaggi et al., 2012, Italy | 45 | 45 | 45 | 56 | (SD ±11) | Nr | 63 (SD 2.85) | IMN |
| Pawar et al., 2013, USA | 5 | 5 | 3 | 59 | (46–82) | Nr | 18 (12–24) | IMN |
| Cullen et al., 2013, USA | 4 | 4 | 4 | 57.3 | (47–70) | 34 (31–35) | 18.5 (10–27) | Mid Foot Fusion Bolt |
| Eschler et al., 2013, Germany | 5 | 5 | 5 | Nr | 6 | Mid Foot Fusion Bolt and dorsal plate | ||
| Wiewiorske et al., 2013, Switzerland | 8 | 8 | 7 | 63 | (46–80) | Nr | 27 (12–44) | Mid Tarsal Bolt |
| Garcher et al., 2013, Switzerland | 24 | 25 | 22 | 58.8 | (42–74) | Nr | 38 (17–64) | Plantar plate |
| Eschler et al., 2014, Germany | 7 | 7 | 7 | 56.3 | (47–68) | Nr | 24 (9–43) | Mid Foot Fusion Bolt |
| Siebachmeyer et al., 2015, UK | 20 | 21 | 20 | 62.6 | (46–83) | 32.7 (15–47) | 26 (8–54) | IMN |
| Richter et al., 2015, Germany | 47 | 48 | 38 | 60.1 | (35–78) | 31.5 (22–42) | 12 (1–35) | Mid Foot Fusion Bolt |
| Matsumoto et al., 2015, USA | 10 | 11 | 9 | 52.2 | (35–64) | 36.32 (27.1–44.3) | 29 (12–44) | Plate and Ex Fix |
| Ettinger et al., 2016, Germany | 58 | 58 | 39 | 59.1 | (26–81) | Nr | 31.3 (12–57) | IMN 38 Ex Fix 19 |
| Hegewald et al., 2016, USA | 22 | 22 | 22 | 54 | (31–75) | 33.59 (20–48) | 58.6 (16–164) | Plate and Ex Fix |
| Vasukutty et al., 2017, UK | 42 | 40 | 40 | 59 | (38–82) | NR | 42 (12–99) | IMN (Hind foot) and mid foot Fixation (Mid foot fusion bolt, Fusion Plate) |
| Chraim et al., 2018, Austria | 18 | 17 | 10 | 63.4 (38.5–79.8) | NR | 46.36 (37–70) | IMN and mid foot |
The largest single surgeon series came from one centre in Maywood, Illinois, USA through 4 different papers (n = 159). However, it is not clear whether there was any patient crossover between publications.22, 23, 24,50 For the purpose of this review we have treated them as separate cohorts. This was also the case with the series reported by Paola et al., and Sammarco et al., which contributed 63 and 56 feet respectively.19,20,26,27,48
Two large series of patients included in our analysis were from Grant et al., (n = 70) and DeVries et al., (n = 52). Most other studies were small series with a mean of 11 patients, the overall mean was 26.7 patients.12,18 These larger studies were considered to be from specialist centres where multidisciplinary care was offered.19, 20, 21, 22, 23, 24, 25,27,43,46 The largest cohort of Charcot reconstructions in 285 patients that discussed the impact of co-morbidities on post-reconstruction amputation risk71 was excluded from our analysis as it did not specify the form/type of reconstruction used, leaving the reader unable to classify reconstruction types.
3.3. Methods of surgical fixation used
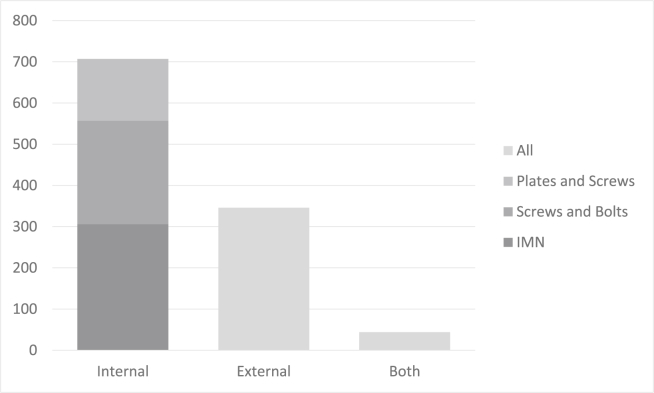
Surgical reconstruction techniques were recorded as external fixation in 346 feet, internal fixation in 726 (150 plates and screws, 251 screws or fusion bolts only, 306 feet managed primarily or in combination with an intramedullary nail with one group adding an implantable bone stimulator) and combined internal and external fixation in 44 (see Fig. 2). There was no correlation between fixation type and year of publication.
Fig. 2.
Number of feet and type of fixation reported in studies.
4. Outcomes
The outcomes reported here are collected form the data available in the referenced literature. Not all studies reported all possible outcomes leading to a discrepancy in total numbers (see Table 2).
Table 2.
A description of the reports (N = 42) and outcomes of charcot reconstruction, include number of feet, results of radiographic union, and interventions undertaken.
| Author, Year, Country | No. of Feet | Fixation Type | Complications | Mean Outcome Score | No. Able to WB (%) | No. Amputated (%) | No. of remaining ulcers (N) |
|---|---|---|---|---|---|---|---|
| Papa et al., 1993, USA | 29 | IMN 25 Ex Fix 4 | 18 (1 amputation, 9 wound complications, 3 broken screws, 2 deep infections, 3 Malunions) | Nr | 27 (93.1%) | 1 (3.4%) | 1 |
| Early et al., 1996, USA | 21 | Screw Fusion | 8 (1 Mortality MI, 3 Wound Complications, 2 Metal Work Failure, 2 Osteomylitis) | Nr | 17 (81.0%) | 2 (9.5%) | 3 |
| Pinzur et al., 1997, USA | 21 | IMN | 13 (1 amputation, 6 wound infections, 3 revisions, 3 removals of metal) | Nr | Nr | 1 (4.8%) | 0 |
| Sammarco et al., 1998, USA | 27 | Midfoot Fusion Bolt | 7 (2 removal of metal, 5 wound complications) | Nr | 26 (96.3%) | 0 (0%) | 0 |
| Stone et al., 2000, Canada | 10 | Plates and Screws, BG | 2 (1 Wound Breakdown, 1 Re-ulceration with progressive deformity) | WOMAC 33% (11%–63%) AOFAS 52 (43–66) | 10 (100%) | 0 (0%) | 1 |
| Simon et al., 2000, USA | 14 | Plates and Screws, BG | 0 | Nr | 14 (100%) | 0 (0%) | 0 |
| Farber et al., 2002, USA | 11 | Ex Fix | 1 Ulcer | Nr | 10 (90.9%) | 0 (0%) | 1 |
| Rooney et al., 2002, Austrailia | 43 | Screw Fusion | 13 (1 amputation, 8 wound complications, 4 removal of prominent screws) | Nr | 42 (97.7%) | 1 (2.3%) | 0 |
| Cooper et al., 2003, USA | 83 | Ex Fix | 13 (7 superficial pin site infections, 2 tibial fractures, 2 ulcers, 1 BKA, 1 revision) | Nr | Nr | 1 (1.2%) | 2 |
| Pinzur et al., 2005, USA | 9 | IMN | 2 (1 Wound infection, 1 Haematoma) | Nr | 9 (100%) | 0 (0%) | 0 |
| Caravaggi et al., 2006, Italy | 14 | IMN | 5 (1 amputation, 4 failures of metal work) | Nr | 13 (92.9%) | 1 (7.1%) | 0 |
| Fabrin et al., 2007, Denmark | 12 | Ex Fix | 7 (1 amputation, 6 wound infections) | Nr | 11 (91.7%) | 1 (8.3%) | 0 |
| Pinzur et al., 2007, USA | 26 | Ex Fix | 8 (1 Death CVA, 1 BKA, 2 tibial stress fractures, 4 ulcers) | Nr | 24 (92.3%) | 1 (3.8%) | 4 |
| Paola et al., 2007, Italy | 18 | IMN | 7 (2 anaemia, 2 Fever, 3 removal of screws) | Nr | 18 (100%) | 0 (0%) | 0 |
| Hockenbury et al., 2007, USA | 10 | IMN with implantable bone growth stimulator | 10 (2 Superficial wound infections, 3 removal of screw, 3 Removal of bone simulator, 2 additional midfoot osteotomy) | AOFAS Score 59 (42–77) | 10 (100%) | 0 (0%) | 0 |
| Pinzur et al., 2007, USA | 51 | Plates and Screws | 9 (3 Amputations, 1 Stress fracture, 3 Ulcers, 2 Revision for loosening) | Nr | 44 (86.3%) | 3 (5.9%) | 3 |
| Ayoub, 2008, Egypt | 17 | Screw Fusion | 9 (3 Amputations, 2 DVT, 4 Superficial wound complications) | Nr | 14 (82.4%) | 3 (17.6%) | 0 |
| El-Gafary et al., 2009, Egypt | 20 | Ex Fix | 17 (2 superficial infections, 15 Pin site infections) | Nr | 20 (100%) | 0 (0%) | 0 |
| Pinzur et al., 2009, USA | 46 | Ex Fix | 6 ulcers, 3 tibial stress fractures, 2 amputations, 2 non unions | Nr | 44 (95.7%) | 2 (4.3%) | 6 |
| Paola et al., 2009, Italy | 45 | Ex Fix | 6 (2 instability requiring IMN, 4 continued infection leading to BKA) | Nr | 39 (86.7%) | 4 (8.9%) | 0 |
| Assal et al., 2009, Switzerland | 15 | Plates and Screws | 2 (1 amputation 1 revision) | Nr | 13 (86.7%) | 1 (6.7%) | 0 |
| Mittlmeier et al., 2009, Germany | 26 | Plates and Screws | 9 | AOFAS Score 70 (hindfoot) 84 (midfoot) | 22 (84.6%) | 0 (0%) | 1 |
| Sammarco et al., 2009, USA | 22 | Screw Fusion | 11 (3 Ulcers, 8 Metal work failures) | Nr | 22 (100%) | 0 (0%) | 3 |
| Cinar et al., 2010, Turkey | 4 | Blade Plate | 4 (1 Fibrous non-union, 2 infections, 1 metal removal) | Modified Boston Children’s Hospital Ankle Scoring System 42 | 4 (100%) | 0 (0%) | 0 |
| Lamm et al., 2010, USA | 11 | Ex Fix and Screws | 14 (14 (3 operative adjustments of external or internal fixation, 11 pin tract infections) | Nr | Nr | 0 (0%) | 0 |
| Grant et al., 2011, USA | 71 | 29 medial & Lateral beaming, 18 medial & Lateral beaming & subtalar arthrodesis, 11 medial & lateral column beaming with subtalar fusion, 12 medial column beaming, 1 medial column beaming combined with subtalar arthrodesis | 38 (5 ulcers due to prominent metal, 1 transfer lesion, 6 pin tract infections, 4 broken pins, 8 osteomyelitis, 10 medial incision dehiscence, 4 medial column broken screws) | Nr | Nr | 0 (0%) | 6 |
| DeVries et al., 2012, USA | 52 | 45 IMN, 7 Ex Fix | Nail 39 (22 I&D, 6 major revision, 1 DVT, 10 Amputations) Ex fix 5 (2 Amputations, 3 I&D) | Nr | 40 (IMN 35, Ex Fix (76.9%) 5) | 12 (23.1%) | 0 |
| Pinzur et al., 2012, USA | 73 | Ex Fix | 15 (1 Death unrelated, 3 Amputations, 10 Wounds, 2 requiring local flaps) | Nr | 68 (93.2%) | 3 (4.1%) | 15 |
| Caravaggi et al., 2012, Italy | 45 | IMN | 24 (10 wound breakdowns, 4 BKA, 10 removal of metal work) | Nr | 39 (86.7%) | 4 (8.9%) | 0 |
| Pawar et al., 2013, USA | 5 | IMN | 0 | Nr | 4 (80.0%) | 0 (0%) | 0 |
| Cullen et al., 2013, USA | 4 | Mid Foot Fusion Bolt | 1 (infection requiring metal removal) | Nr | 4 (100%) | 0 (0%) | 1 |
| Eschler et al., 2013, Germany | 5 | Mid Foot Fusion Bolt and dorsal plate | 0 | Nr | Nr | 0 (0%) | 0 |
| Wiewiorske et al., 2013, Switzerland | 8 | Mid Tarsal Bolt | 3 (1 Deep Infection, 2 Bolt Migration) | AOFAS Score 67 (58–83) Inlow DFS 8 (5–11) | 8 (100%) | 0 (0%) | 0 |
| Garcher et al., 2013, Switzerland | 25 | Plantar plate | 10 (4 Infection, 2 Ulcers, Wound Dehiscence, 3 Charcot Developing into other joints, 1 Ulcer secondary to cast) | Nr | 24 (96.0%) | 0 (0%) | 2 |
| Eschler et al., 2014, Germany | 7 | Mid Foot Fusion Bolt | 6 (2 amputation, 4 wound infections) | Nr | 1 (14.2%) | 2 (28.6%) | 1 |
| Siebachmeyer et al., 2015, UK | 21 | IMN | 7 (1 failure of metal work, 3 migration of metal work, 3 recurrent ulceration) | AOFAS Score 65.2 (22–88) SF-36 29.8 (17.7–44.2) EQ-5D-5L 0.67 (0.57–0.84) | 20 (95.2%) | 0 (0%) | 3 |
| Richter et al., 2015, Germany | 48 | Mid Foot Fusion Bolt | 30 (10 wound complications, 6 deep infections, 5 amputations) | Nr | 5 (10.4%) | 6 | |
| Matsumoto et al., 2015, USA | 11 | Ex Fix and Plate | 3 (2 ulcers 1 superficial wound) | Nr | 11 (1000%) | 0 (0%) | 2 |
| Ettinger et al., 2016, Germany | 58 | IMN 38 Ex Fix 19 | 3 (Infections requiring amputation) | Nr | Nr | 2 (Ex Fix) (3.4%) | nr |
| Hegewald et al., 2016, USA | 22 | Ex Fix and Plate | 12 (10 infections, 2 BKA) | Nr | 20 (90.9%) | 2 (9.1%) | 6 |
| Vaskutty et al., 2018, UK | 42 | IMN and Plate | 5 infection, 5 screw migration, 2 re-current ulcers, 1 metal failure, 1 non- union | Nr | 35 (83.0%) | 0 (0)% | 2 |
| Chraim et al, 2018, Austria | 19 | IMN and mid foot | 3 Amputations for deep infection, 2 removal of metal work, 1 revision, 2 dynamisation of nail | AOFAS Score 71.5 (SD 9.5), FAOS 87.2 (SD 40.9) |
16 (84.2%) | 3 (15.8%) | nr |
4.1. Improvement in PROMs
A number of patient reported outcomes (PROMs) were used in 6 studies (74 patients). Overall, 6 different measures were used and there was an overall improvement by 38 points in the AOFAS scores and all of these were in patients who underwent different forms of internal fixation.31, 32, 33, 34,48,51
4.2. Fusion rates
Bony fusion, according to radiographic and clinical examination, occurred in 532 of 618 feet (86%) (see Table 3). Of these, 203 of 217 (94%) feet were in the external fixator reconstructed group, 287 of 357 (81%) in the internal fixation and 42 out of 44 (95%) in the group that utilised both internal and external fixation.10,11,13, 14, 15, 16, 17,19,21,22,26,29, 30, 31,33, 34, 35,37,39, 40, 41, 42, 43,47,51, 52, 53
Table 3.
Summary of Outcomes of the major methods of surgical reconstruction. All methods have high fusion rates and weightbearing/ambulation is achieved within less than 20 weeks.
| Overall | Internal | External | Both | |
|---|---|---|---|---|
| Complications % | 36 | 41 | 25 | 70 |
| Fusion % | 86 | 81 | 94 | 95 |
| Time to WB (weeks) | 16.5 | 16 | 19 | 17 |
4.3. Time to weight bearing ambulation
Weight bearing was documented in 20 studies with a mean of 16.5 weeks to full weight bearing ambulation. A mean duration of 19 weeks was identified in external fixation group, 16 weeks with internal fixation and 17 weeks with a combination of both (see Table 3). Within the external fixation group weight bearing ambulation was not correlated with removal of frame.11,13,34,35,37,40,42,44,46,52,53,14,15,17,19,26,28,29,31,64
4.4. Complication rates
The overall complication rate was 397 in 1116 (36%) feet. Further analysis revealed fixation specific complications to be 85 of 346 (25%) in the external fixation, 293 of 707 (41.4%) in the internal fixation (27 plates and screws, 126 screws, and 140 intramedullary nail) and 31 out of 44 (70%) in combined fixation groups. The local complications included for analysis were revision surgery, failure of metal work, superficial and deep infections, pin site infections, removal of metal work, and wound dehiscence. We observed either failure of healing or recurrence of ulceration in 63 out of 1008 feet. Systemic complications included 3 mortalities, 1 due to myocardial infarction, 1 CVA, and 1 with no known cause detailed.13,23,50
4.5. Post-surgical reconstruction amputation rates
The overall amputation rate was 55 of 1100 feet (5.0%): 19 of 364 (5.2%) in the external fixation, 34 of 767 (4.4%) of those with internal fixation (2 plates and screws, 13 screws only and 19 intramedullary nail) and 2 of 44 (4.5%) in the combined group.
4.6. Statistical assessment of review
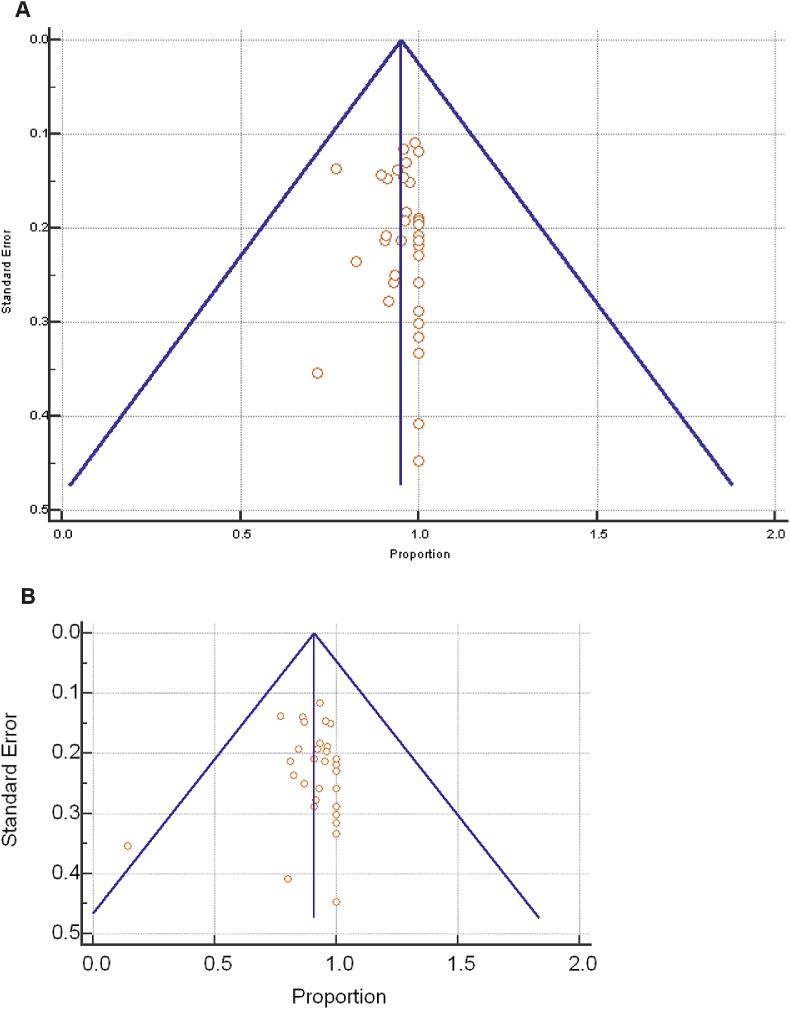
We observed significant differences in study designs, inconsistences in data collection and reporting of outcomes that were recorded. Funnel plot analysis was conducted to assess publication bias around the mean with our two principle outcomes (Fig. 3A and B):
-
•
Amputation rates following reconstructive surgery – revealed low heterogeneity, (Q = 63.06, I2 = 26.23%, p = 0.073). The overall estimated percentage of patients undergoing amputation after surgical reconstruction was 5.5% (95% CI: 3.9–7.3).
-
•
Weight bearing ambulation - The overall estimated percentage of patients returning to weight bearing ambulation in the analysis was 91% (95% CI: 87.8–93.7) but with evidence of moderate heterogeneity existing with regard to return to weight bearing ambulation (Q = 50.16, I2 = 49.26%, p = 0.0009).
Fig. 3.
A & B. Funnel plot assessing heterogeneity of studies following the Cochrane review guidelines, for the outcome of amputation (A) and mobilisation (B). Showing a symmetrical inverted funnel shape suggesting symmetry around the mean and in which 95% of studies are found within the simple triangular region as would be expected to lie in the absence of both significant bias and heterogeneity.
The results of the random effects analysis compared with a fixed effects model indicated there was no significant difference (P < 0.05) between the fixed and random effects estimates to suggest over interpretation of the results of smaller studies. Moderate evidence of study heterogeneity existed between our secondary outcomes (Deep & superficial infection, re-ulceration, revision surgery, and metalwork failure) and subgroup analysis performed for each outcome based on the operative technique selected for joint reconstruction revealed no statistical inferences can be drawn.
5. Discussion
Charcot neuroarthropathy is a debilitating condition. The development of Charcot foot and ankle deformity can have a dramatic negative affect on lifestyle, frequently leading to disability and premature retirement from work.54 Surgical reconstruction may provide the individual with an opportunity to preserve the foot and achieve improved function. In this review, we set out to explore the various techniques available, their surgical impact and reported outcomes.
5.1. Increasing volumes of surgical fixation
Surgical reconstruction of Charcot foot is being increasingly considered as an option towards achieving functional limb salvage and this is evident by the increase in the number of reported studies over the last 5 years compared to the previous 15 years.
However, the cohort sizes of the case series are still relatively small, possibly due to the complexity of these procedures and the associated high complication rates.18 Only 3 studies reported over 70 patients; although the largest series from 2018 was not included due to methodological issues which meant it did not meet the inclusion criteria. The mean number of patients in each study was less than 11, when we excluded the 3 largest series (n = 39 studies).
5.2. Methods of fixation
We found that no one particular technique had a higher frequency of outcome reporting when compared to the others. Furthermore, the reported clinical outcomes did not vary considerably between the different techniques. A number of authors who used internal fixation techniques preferred long segment or ‘Super construct techniques’ as coined by Sammarco et al., where the fixation is extended beyond the zone of damage in order to include the adjacent joints that are not effected by the Charcot process, thereby improving the fixation construct.45,47,52,53
External fixation may offer some advantages over internal fixation, allowing stable fixation, whilst ensuring access to open wounds and potentially allowing weight bearing at an earlier stage, although our findings do not clearly support this. 15,16, 24,55,56,57,58,59, 60,61,62 There are some studies that describe amputation techniques and correction with external fixation but as yet no direct comparision with reconstruction surgery exists and external fixation may be tailored to those patients where there is a suggestion of ongoing infection. 63,64,65,66,67
In studies where external fixation was the method of stabilisation, the mean time to weight bearing was 19 weeks.14,15,19 This is longer than the time observed with internal fixation (16 weeks), although clinically it is unclear how much benefit the 3 weeks would confer.11,13,17,20,27,29,31,34,48,52 Neither is it clear if frame removal is undertaken at this time or when the feet are shod in bespoke footwear or that patients are allowed to dynamise or compress at the fusion sites in the frame prior to removal.
5.3. Outcome comparison
Weight bearing and amputation were the commonly used outcomes and only 6 studies used PROMs assessment. The mean time to weight bearing was 17 weeks, one finding that was consistently and clearly reported in the studies.
Dhawan et al., found AOFAS-DFQ and SF36 to be useful tools in monitoring and assessing patients, and recommended that these would be useful when developing treatment strategies as these would allow the assessment of longer term improvements and comparison with other treatment modalities.63 Other studies have reported the use of visual analogue score (VAS) and foot and ankle outcome score (FAOS) for Charcot foot reconstructions. However, there is a significant risk that these outcome scores may not truly represent patients’ expectations following such complex functional limb salvage procedures.72,73,74 Wulkich et al., reported limb salvage as being perceived by the patients to be more important than death among those with diabetic foot disease; one could conclude that it is desirable to have specific PROMS for this group of conditions.77
5.4. Fusion rates
Fusion rates are seen as an important surgical outcome measures for such techniques.76 The overall fusion rate in the studies was 86% (see Table 3). However, we found that there was a significant heterogeneity between the methodologies used for recording fusion rates. This meant we were unable to firmly conclude if one surgical technique was superior to the other in achieving this.
Even so, it is worth noting that, despite with the aim of achieving full bone fusion, multiple studies have observed that fibrous non-unions provide adequate foot stability with good functional outcomes obviating the need for additional surgical interventions.16 The role and natural history of the fibrous non-union in the Charcot patient is yet to still be fully determined. Certainly, Chraim et al., in 2018 also concluded that fibrous union was not necessarily a poor outcome and the patient outcomes are still satisfactory if the reconstructed foot is stable and would allow functional ambulation.78
Poor diabetes control has been attributed to the risk of failure of bone fusion.71 Other known risk factors associated with delayed/non-union, such as smoking and non-steroidal anti-inflammatory drugs, were not well detailed throughout the reviewed studies. Ayoub et al.30 quoted the smoking rates among study subjects and Fragomen compared the union rates in comparative groups that demonstrated a negative impact from smoking.67 Other characteristics to be considered for failure include ethnicity and socioeconomic class. For example, in an unselected diabetes population, Lavery et al. reported in a prospective cohort of 1666 patients that Mexican Americans had a 3.8 times higher rate of major amputation than non-Hispanic whites.70
The retention of talus appears to influence the fusion rate in hindfoot arthrodesis. Papa et al., reviewed 29 diabetic patients who underwent hindfoot arthrodesis (25 retrograde IMN and 4 external fixation).21 Of the 11 tibio-calcaneal (post talectomy) fusions 6 went onto non-union (45% union rate), compared to the only one non-union out of 9 in the tibio-talo-calcaneal fusions that were performed using cannulated screws (89% union rate). Fabrin et al., reports similar results; they reviewed 11 patients with CN of hindfoot (12 feet) whom underwent reconstructions using external fixation.15 Seven of these cases were tibio-talar and 5 tibio-calcaneal fusions. The union rate in the tibio-calcaneal group was lower (20%) compared to 72% for tibio talar (similar to the overall review bony fusion rate of 71%). Analysis of such factors may allow identification of high-risk patients, to aid case selection and obtain appropriate informed consent. Fragomen et al., looked at factors affecting ankle fusion rates in complex cases using an Ilizarov method. They identified smoking and Charcot neuroarthropathy to have higher rates of non-union and in isolated ankle fusion.67
5.5. Fusion rates with bone stimulation
Hockenbury et al., combined arthrodesis with implantable bone stimulator in 10 patients in order to improve fusion rates.33 They achieved a fusion rate of 90%; however, 3 patients (33%) had complications directly attributable to the bone stimulator. Lau et al. also used implanted direct-current bone stimulators in 38 patients (40 feet) of which 14 had CN.68,69 They reported a 65% union rate (26 of 40 feet) and a complication rate (excluding non-union) of 40% (16 feet), with deep infection noted in 6 cases requiring the need for device removal and one case of amputation related to the implant. It was noted that the device carried high risks in diabetic patients but did not have any adverse effects in other patients.
5.6. Use of bio-adjuvants and orthobiologic agents
Bio-adjuvants and orthobiologic agents have been proposed to augment the healing process during bone fusion procedures. Orthobiologic agents such as platelet rich plasma, bone morphogenic proteins and demineralised bone matrix have been used in Charcot foot reconstructions. Pinzur et al. described 44 patients with CN that had undergone reconstructions with external fixation, who at the time of surgery had platelet rich concentrate and iliac crest bone marrow aspirate injected at the site of the osteotomy.43 The results were encouraging at 91.3% successful fusion rate based on clinical and radiographic evaluation. Fragomen et al., and stated that biologics such as bone morphogenic protein (BMP) may improve the fusion outcomes.67
5.7. Complications and post-surgical amputation
As expected, within this high-risk group of patients the complication rates were high at 36% overall. Surprisingly, the complication rate in those treated with external fixation was lower at 26%, compared to the internal fixation patients at 43%. However, pin site infections were largely unreported or underreported which may account for this discrepancy. When a combination of internal and external fixation methods was utilised in the same patient, the complication rates were higher at 64%, but the numbers were too small to derive any definitive conclusions.16,35 The overall rate of re-ulceration or non-healing of an ulcer was 6.25%.
The reported post-reconstruction amputation rates where are low at 5.5%. Only one study reported risk factors for a major amputation following reconstruction.17 It identified peripheral artery disease, renal disease, delayed postoperative healing, postoperative wound infection, postoperative osteomyelitis, transfer ulceration, new site of Charcot neuroarthropathy and post-reconstruction non-union as predictors of post-reconstruction amputation.17
There were no studies specifically examining the role of delayed wound closure, the usage of incisional negative pressure wound therapy, the types of dressings used or the use of biologics impregnated with antibiotics; all of which may be useful in future areas of research.
5.8. Limitation of current study
The median number of 24 patients (26.7 feet) per study in this review is small, and most larger series come from selected specialist centres and this may carry a bias. There are also inherent differences between treatment strategies from operative techniques and post-operative regimens. In addition, the impact of the pre-operative duration of deformity and/or ulceration on post-operative outcomes and complications could not be ascertained.
These and the additional factors discussed earlier make it difficult to derive meaningful conclusions and these highlight the need for either multicentre studies or a national registry of Charcot foot reconstructions to standardise the outcomes. At present we cannot provide statistically significant evidence for all our outcomes described in this systematic review due to the significant heterogeneity of study designs and the outcomes reported. Nonetheless, this review identifies potential benefit from Charcot reconstruction, irrespective of the technique used, although the quality of evidence is overall low.
Taking this into consideration the following conclusions can be drawn:
-
•
There does not appear to be any overwhelming difference in the reported rates of functional limb salvage, peri-procedural complications or post-reconstruction amputation rates between the surgical techniques.
-
•
Surgical priorities include: good surgical technique, with preservation of bone stock (e.g. talus), good bone apposition and stable rigid fixation.
-
•
Consideration may be given on the use of adjuvants such as orthobiologics, bio-adjuvants or implantable bone stimulators that can potentially improve the fusion rates, but there is currently insufficient evident on their routine usage.
-
•
Further data is required regarding the alternatives to reconstruction with specific consideration to this cohort of patient that are often neuropathic and have multiple comorbidities, to provide comparative functional outcome and fiscal utility of these techniques.
Further analysis on the outcomes following Charcot foot reconstructions will require the development of registries or common standards. A consensus should ideally be reached of what variables need to be captured and standardisation of surgical outcomes reporting should be considered to allow comparability of published results.
6. Conclusion
Surgical reconstruction is conducted by specialist centres in large volumes, in selected patients with Charcot neuroarthropathy. In the vast majority of cases it provides a predictable pathway for these patients to weight bear, and achieve functional limb salvage. Especially in a sub-group of patients where primary amputation can be considered the only other option.
However, there is still a paucity of data comparing alternatives such as non-operative treatment or primary amputation to accurately understand its clinical utility. Further studies aimed at refining selection criteria and treatment algorithms are therefore required for greater standardisation of outcomes.
Declaration of competing interest
The authors have no declaration of interest and neither any conflicts of interest to report. The authors certify that they have obtained all appropriate patient consent and the patient has given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published.
Acknowledgements
No conflicts of interest are declared
Contributor Information
Raju Ahluwalia, Email: r.ahluwalia1@nhs.net.
Venu Kavarthapu, Email: venu.kavarthapu@nhs.net.
Appendix.
Fig. 1.
Study selection flow diagram. This outlines the filtering process from literature search to study inclusion.
References
- 1.Pinzur M.S., Evans A. Health-related quality of life in patients with Charcot foot. Am J Orthoped. 2003;32:492–496. [PubMed] [Google Scholar]
- 2.Schon L.C., Easley M.E., Weinfeld S.B. Charcot neuroarthropathy of the foot and ankle. Clin Orthop Relat Res. 1998:116–131. doi: 10.1097/00003086-199804000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Robinson A.H., Pasapula C., Brodsky J.W. Surgical aspects of the diabetic foot. J Bone Jt Surg - Br. 2009;91:1–7. doi: 10.1302/0301-620X.91B1.21196. [DOI] [PubMed] [Google Scholar]
- 4.Pinzur M.S., Sage R., Stuck R., Kaminsky S., Zmuda A. A treatment algorithm for neuropathic (Charcot) midfoot deformity. Foot Ankle. 1993;14:189–197. doi: 10.1177/107110079301400403. [DOI] [PubMed] [Google Scholar]
- 5.Myerson M.S., Edwards W.H. Management of neuropathic fractures in the foot and ankle. J Am Acad Orthop Surg. 1999;7:8–18. doi: 10.5435/00124635-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Pinzur M. Surgical versus accommodative treatment for Charcot arthropathy of the midfoot. Foot Ankle Int. 2004;25:545–549. doi: 10.1177/107110070402500806. [DOI] [PubMed] [Google Scholar]
- 7.Evans K.K., Attinger C.E., Al-Attar A. The importance of limb preservation in the diabetic population. J Diabetes Its Complicat. 2011;25:227–231. doi: 10.1016/j.jdiacomp.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 8.McCabe C.J., Stevenson R.C., Dolan A.M. Evaluation of a diabetic foot screening and protection programme. Diabet Med. 1998;15:80–84. doi: 10.1002/(SICI)1096-9136(199801)15:1<80:AID-DIA517>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 9.Lowery N.J., Woods J.B., Armstrong D.G., Wukich D.K. Surgical management of Charcot neuroarthropathy of the foot and ankle: a systematic review. Foot Ankle Int. 2012;33:113–121. doi: 10.3113/FAI.2012.0113. [DOI] [PubMed] [Google Scholar]
- 10.Caravaggi C., Cimmino M., Caruso S., Dalla S. Intramedullary compressive nail fixation for the treatment of severe Charcot deformity of the ankle and rear foot. J Foot Ankle Surg. 2006;45:20–24. doi: 10.1053/j.jfas.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Cullen B.D., Weinraub G.M., Van G. Early results with use of the midfoot fusion bolt in Charcot arthropathy. J Foot Ankle Surg. 2013;52:235–238. doi: 10.1053/j.jfas.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 12.DeVries J.G., Berlet G.C., Hyer C.F. A retrospective comparative analysis of Charcot ankle stabilization using an intramedullary rod with or without application of circular external fixator-utilization of the Retrograde Arthrodesis Intramedullary Nail database. J Foot Ankle Surg. 2012;51:420–425. doi: 10.1053/j.jfas.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Early J.S., Hansen S.T. Surgical reconstruction of the diabetic foot: a salvage approach for midfoot collapse. Foot Ankle Int. 1996;17:325–330. doi: 10.1177/107110079601700605. [DOI] [PubMed] [Google Scholar]
- 14.El-Gafary K.A., Mostafa K.M., Al-Adly W.Y. The management of Charcot joint disease affecting the ankle and foot by arthrodesis controlled by an Ilizarov frame: early results. J Bone Jt Surg - Br. 2009;91:1322–1325. doi: 10.1302/0301-620X.91B10.22431. [DOI] [PubMed] [Google Scholar]
- 15.Fabrin J., Larsen K., Holstein P.E. Arthrodesis with external fixation in the unstable or misaligned Charcot ankle in patients with diabetes mellitus. Int J Low Extrem Wounds. 2007;6:102–107. doi: 10.1177/1534734607302379. [DOI] [PubMed] [Google Scholar]
- 16.Farber D.C., Juliano P.J., Cavanagh P.R., Ulbrecht J., Caputo G. Single stage correction with external fixation of the ulcerated foot in individuals with Charcot neuroarthropathy. Foot Ankle Int. 2002;23:130–134. doi: 10.1177/107110070202300209. [DOI] [PubMed] [Google Scholar]
- 17.Garchar D., DiDomenico L.A., Klaue K. Reconstruction of Lisfranc joint dislocations secondary to Charcot neuroarthropathy using a plantar plate. J Foot Ankle Surg. 2013;52:295–297. doi: 10.1053/j.jfas.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 18.Grant W.P., Garcia-Lavin S., Sabo R. Beaming the columns for Charcot diabetic foot reconstruction: a retrospective analysis. J Foot Ankle Surg. 2011;50:182–189. doi: 10.1053/j.jfas.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Dalla Paola L., Brocco E., Ceccacci T. Limb salvage in Charcot foot and ankle osteomyelitis: combined use single stage/double stage of arthrodesis and external fixation. Foot Ankle Int. 2009;30:1065–1070. doi: 10.3113/FAI.2009.1065. [DOI] [PubMed] [Google Scholar]
- 20.Dalla L., Volpe A., Varotto D. Use of a retrograde nail for ankle arthrodesis in Charcot neuroarthropathy: a limb salvage procedure. Foot Ankle Int. 2007;28:967–970. doi: 10.3113/FAI.2007.0967. [DOI] [PubMed] [Google Scholar]
- 21.Papa J., Myerson M., Girard P. Salvage, with arthrodesis, in intractable diabetic neuropathic arthropathy of the foot and ankle. J Bone Jt Surg - Am. 1993;75:1056–1066. doi: 10.2106/00004623-199307000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Pinzur M.S., Noonan T. Ankle arthrodesis with a retrograde femoral nail for Charcot ankle arthropathy. Foot Ankle Int. 2005;26:545–549. doi: 10.1177/107110070502600709. [DOI] [PubMed] [Google Scholar]
- 23.Pinzur M.S., Sostak J. Surgical stabilization of nonplantigrade Charcot arthropathy of the midfoot. Am J Orthoped. 2007;36:361–365. [PubMed] [Google Scholar]
- 24.Pinzur M.S. Neutral ring fixation for high-risk nonplantigrade Charcot midfoot deformity. Foot Ankle Int. 2007;28:961–966. doi: 10.3113/FAI.2007.0961. [DOI] [PubMed] [Google Scholar]
- 25.Pinzur M.S., Sammarco V.J., Wukich D.K. Charcot foot: a surgical algorithm. Instr Course Lect. 2012;61:423–438. [PubMed] [Google Scholar]
- 26.Sammarco G.J., Conti S.F. Surgical treatment of neuroarthropathic foot deformity. Foot Ankle Int. 1998;19:102–109. doi: 10.1177/107110079801900209. [DOI] [PubMed] [Google Scholar]
- 27.Sammarco V.J., Sammarco G.J., Walker E.W., Jr., Guiao R.P. Midtarsal arthrodesis in the treatment of Charcot midfoot arthropathy. J Bone Jt Surg - Am. 2009;91:80–91. doi: 10.2106/JBJS.G.01629. [DOI] [PubMed] [Google Scholar]
- 28.Simon S.R., Tejwani S.G., Wilson D.L., Santner T.J., Denniston N.L. Arthrodesis as an early alternative to nonoperative management of charcot arthropathy of the diabetic foot. J Bone Jt Surg - Am. 2000;82–A:939–950. doi: 10.2106/00004623-200007000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Pawar A., Dikmen G., Fragomen A., Rozbruch S.R. Antibiotic-coated nail for fusion of infected charcot ankles. Foot Ankle Int. 2013;34:80–84. doi: 10.1177/1071100712460209. [DOI] [PubMed] [Google Scholar]
- 30.Ayoub M.A. Ankle fractures in diabetic neuropathic arthropathy: can tibiotalar arthrodesis salvage the limb? J Bone Jt Surg - Br. 2008;90:906–914. doi: 10.1302/0301-620X.90B7.20090. [DOI] [PubMed] [Google Scholar]
- 31.Cinar M., Derincek A., Akpinar S. Tibiocalcaneal arthrodesis with posterior blade plate in diabetic neuroarthropthy. Foot Ankle Int. 2010;31:511–516. doi: 10.3113/FAI.2010.0511. [DOI] [PubMed] [Google Scholar]
- 32.Wiewiorski M., Yasui T., Miska M., Frigg A., Valderrabano V. Solid bolt fixation of the medial column in Charcot midfoot arthropathy. J Foot Ankle Surg. 2013;52:88–94. doi: 10.1053/j.jfas.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 33.Hockenbury R.T., Gruttadauria M., McKinney I. Use of implantable bone growth stimulation in Charcot ankle arthrodesis. Foot Ankle Int. 2007;28:971–976. doi: 10.3113/FAI.2007.0971. [DOI] [PubMed] [Google Scholar]
- 34.Mittlmeier T., Klaue K., Haar P., Beck M. Should one consider primary surgical reconstruction in charcot arthropathy of the feet? Clin Orthop Relat Res. 2010;468:1002–1011. doi: 10.1007/s11999-009-0972-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Matsumoto T., Parekh S.G. Midtarsal reconstructive arthrodesis using a multi-axial correction fixator in charcot midfoot arthropathy. Foot Ankle Spec. 2015;8:472–478. doi: 10.1177/1938640015592835. [DOI] [PubMed] [Google Scholar]
- 36.Ettinger S., Plaass C., Claassen L., Stukenborg-Colsman C., Yao D., Daniilidis K. Surgical management of charcot deformity for the foot and ankle-radiologic outcome after internal/external fixation. J Foot Ankle Surg. 2016;55:522–528. doi: 10.1053/j.jfas.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 37.Hegewald K.W., Wilder M.L., Chappell T.M., Hutchinson B.L. Combined internal and external fixation for diabetic charcot reconstruction: a retrospective case series. J Foot Ankle Surg. 2015;55:619–627. doi: 10.1053/j.jfas.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 38.Richter M., Mittlmeier T., Rammelt S., Agren P.H., Hahn S., Eschler A. Intramedullary fixation in severe Charcot osteo-neuroarthropathy with foot deformity results in adequate correction without loss of correction - results from a multi-centre study. Foot Ankle Surg. 2015;21:269–276. doi: 10.1016/j.fas.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 39.Lamm B.M., Gottlieb H.D., Paley D. A two-stage percutaneous approach to charcot diabetic foot reconstruction. J Foot Ankle Surg. 2010;49:517–522. doi: 10.1053/j.jfas.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 40.Caravaggi C.M.F., Sganzaroli A.B., Galenda P. Long-term follow-up of tibiocalcaneal arthrodesis in diabetic patients with early chronic charcot osteoarthropathy. J Foot Ankle Surg. 2012;51:408–411. doi: 10.1053/j.jfas.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 41.Cooper P.S. Application of external fixators for management of charcot deformities of the foot and ankle. Semin Vasc Surg. 2003;16:67–78. doi: 10.1053/svas.2003.50007. [DOI] [PubMed] [Google Scholar]
- 42.Pinzur M.S., Kelikian A. Charcot ankle fusion with a retrograde locked intramedullary nail. Foot Ankle Int/Am Orthop Foot Ankle Soc [and] Swiss Foot Ankle Soc. 1997;18:699–704. doi: 10.1097/BTF.0b013e31803270fb. [DOI] [PubMed] [Google Scholar]
- 43.Pinzur M.S. Use of platelet-rich concentrate and bone marrow aspirate in high-risk patients with Charcot arthropathy of the foot. Foot Ankle Int. 2009;30:124–127. doi: 10.3113/FAI-2009-0124. [DOI] [PubMed] [Google Scholar]
- 44.Rooney J., Hutabarat S.R., Grujic L., Hansen S.T. Surgical reconstruction of the neuropathic foot. Foot. 2002;12:213–223. doi: 10.1016/S0958259202000706. [DOI] [Google Scholar]
- 45.Siebachmeyer M., Boddu K., Bilal A. Outcome of one-stage correction of deformities of the ankle and hindfoot and fusion in Charcot neuroarthropathy using a retrograde intramedullary hindfoot arthrodesis nail. Bone Joint Lett J. 2015;97–B:76–82. doi: 10.1302/0301-620X.97B1.34542. [DOI] [PubMed] [Google Scholar]
- 46.Eschler A., Ulmar B., Mittlmeier T., Gradl G. Combined intra- and extramedullary fixation for Charcot arthropathy – a promising concept? Injury. 2015;44:S19. doi: 10.1016/S0020-1383(13)70083-4. [DOI] [Google Scholar]
- 47.Eschler A., Wussow A., Ulmar B., Mittlmeier T., Gradl G. Intramedullary medial column support with the Midfoot Fusion Bolt (MFB) is not sufficient for osseous healing of arthrodesis in neuroosteoarthropathic feet. Injury. 2014;45(Suppl 1):S38–S43. doi: 10.1016/j.injury.2013.10.037. [DOI] [PubMed] [Google Scholar]
- 48.Herscovici D., Sammarco G.J., Sammarco V.J., Scaduto J.M. Pantalar arthrodesis for post-traumatic arthritis and diabetic neuroarthropathy of the ankle and hindfoot. Foot Ankle Int. 2011;32:581–588. doi: 10.3113/FAI.2011.0581. [DOI] [PubMed] [Google Scholar]
- 49.Pinzur M.S. The development of a neuropathic ankle following successful correction of non-plantigrade charcot foot deformity. Foot Ankle Int. 2012;33:644–646. doi: 10.3113/FAI.2012.0644. [DOI] [PubMed] [Google Scholar]
- 50.Pinzur M.S., Gil J., Belmares J. Treatment of osteomyelitis in charcot foot with single-stage resection of infection, correction of deformity, and maintenance with ring fixation. Foot Ankle Int. 2012;33:1069–1074. doi: 10.3113/FAI.2012.1069. [DOI] [PubMed] [Google Scholar]
- 51.Stone N.C., Daniels T.R. Midfoot and hindfoot arthrodeses in diabetic Charcot arthropathy. Can J Surg. 2000;43:449–455. [PMC free article] [PubMed] [Google Scholar]
- 52.Assal M., Stern R. Realignment and extended fusion with use of a medial column screw for midfoot deformities secondary to diabetic neuropathy. J Bone Jt Surg - Am. 2009;91:812–820. doi: 10.2106/JBJS.G.01396. [DOI] [PubMed] [Google Scholar]
- 53.Sammarco V.J. Superconstructs in the treatment of charcot foot deformity: plantar plating, locked plating, and axial screw fixation. Foot Ankle Clin. 2009;14:393–407. doi: 10.1016/j.fcl.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 54.Pinzur M.S. Benchmark analysis of diabetic patients with neuropathic (Charcot) foot deformity. Foot Ankle Int. 1999;20:564–567. doi: 10.1177/107110079902000905. [DOI] [PubMed] [Google Scholar]
- 55.Conway J.D. Charcot salvage of the foot and ankle using external fixation. Foot Ankle Clin. 2008;13:157–173. doi: 10.1016/j.fcl.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 56.Cooper P.S. Application of external fixators for management of Charcot deformities of the foot and ankle. Semin Vasc Surg. 2003;16:67–78. doi: 10.1053/svas.2003.50007. [DOI] [PubMed] [Google Scholar]
- 57.Cooper P.S. Application of external fixators for management of Charcot deformities of the foot and ankle. Foot Ankle Clin. 2002;7:207–254. doi: 10.1016/s1083-7515(02)00019-0. [DOI] [PubMed] [Google Scholar]
- 58.Herbst S.A. External fixation of Charcot arthropathy. Foot Ankle Clin. 2004;9:595–609. doi: 10.1016/j.fcl.2004.05.010. x. [DOI] [PubMed] [Google Scholar]
- 59.Jolly G.P., Zgonis T., Polyzois V. External fixation in the management of Charcot neuroarthropathy. Clin Podiatr Med Surg. 2003;20:741–756. doi: 10.1016/S0891-8422(03)00071-5. [DOI] [PubMed] [Google Scholar]
- 60.Pinzur M.S. The role of ring external fixation in Charcot foot arthropathy. Foot Ankle Clin. 2006;11:837–847. doi: 10.1016/j.fcl.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 61.Roukis T.S., Zgonis T. The management of acute Charcot fracture-dislocations with the Taylor’s spatial external fixation system. Clin Podiatr Med Surg. 2006;23:467–483. doi: 10.1016/j.cpm.2006.01.008. viii. [DOI] [PubMed] [Google Scholar]
- 62.Sayner L.R., Rosenblum B.I. External fixation for Charcot foot reconstruction. Curr Surg. 2005;62:618–623. doi: 10.1016/j.cursur.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 63.Dhawan V., Spratt K.F., Pinzur M.S., Baumhauer J., Rudicel S., Saltzman C.L. Reliability of AOFAS diabetic foot questionnaire in Charcot arthropathy: stability, internal consistency, and measurable difference. Foot Ankle Int. 2005;26:717–731. doi: 10.1177/107110070502600910. [DOI] [PubMed] [Google Scholar]
- 64.Eckardt A., Schollner C., Decking J. The impact of Syme amputation in surgical treatment of patients with diabetic foot syndrome and Charcot-neuro-osteoarthropathy. Arch Orthop Trauma Surg. 2004;124:145–150. doi: 10.1007/s00402-003-0622-9. [DOI] [PubMed] [Google Scholar]
- 65.Altindas M., Kilic A., Ceber M. A new limb-salvaging technique for the treatment of late stage complicated Charcot foot deformity: two-staged Boyd’s operation. J Foot Ankle Surg. 2012;18:190–194. doi: 10.1016/j.fas.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 66.Gessmann J., Citak M., Fehmer T., Schildhauer T.A., Seybold D. Ilizarov external frame technique for pirogoff amputations with ankle disarticulation and tibiocalcaneal fusion. Foot Ankle Int. 2013;34:856–864. doi: 10.1177/1071100713475612. [DOI] [PubMed] [Google Scholar]
- 67.Fragomen A.T., Borst E., Schachter L., Lyman S., Rozbruch S.R. Complex ankle arthrodesis using the Ilizarov method yields high rate of fusion. Clin Orthop Relat Res. 2012;470:2864–2873. doi: 10.1007/s11999-012-2470-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lau J.T., Stamatis E.D., Myerson M.S., Schon L.C. Implantable direct-current bone stimulators in high-risk and revision foot and ankle surgery: a retrospective analysis with outcome assessment. Am J Orthoped. 2007;36:354–357. [PubMed] [Google Scholar]
- 69.Petrisor B., Lau J.T. Electrical bone stimulation: an overview and its use in high risk and Charcot foot and ankle reconstructions. Foot Ankle Clin. 2005;10:609–620. doi: 10.1016/j.fcl.2005.06.003. vii–viii. [DOI] [PubMed] [Google Scholar]
- 70.Lavery L.A., Armstrong D.G., Wunderlich R.P., Tredwell J., Boulton A.J.M. Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-Hispanic whites from a diabetes disease management cohort. Diabetes Care. 2003;26:1435–1438. doi: 10.2337/diacare.26.5.1435. [DOI] [PubMed] [Google Scholar]
- 71.Leeb M., Choia W.J., Hana S.H., Janga J., Lee J.W. Uncontrolled diabetes as a potential risk factor in tibiotalocalcaneal fusion using a retrograde intramedullary nail. Foot Ankle Surg. 2018;24:542–548. doi: 10.1016/j.fas.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 72.Elmarsafi T., Anghel E.A., Sinkin J. Risk factors associated with major lower extremity amputation after osseous diabetic charcot reconstruction. J Foot Ankle Surg. 2019;58:295–300. doi: 10.1053/j.jfas.2018.08.059. [DOI] [PubMed] [Google Scholar]
- 73.Kitaoka H.B., Alexander I.J., Adelaar R.S., Nunley J.A., Myerson M.S., Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 74.Ibrahim T., Beiri A., Azzabi M., Best A.J., Taylor G.J., Menon D.K. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007;46(2):65–74. doi: 10.1053/j.jfas.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 75.Higgins Julian PT., Green Sally. Cochrane handbook for systematic reviews of interventions. https://handbook-5-1.cochrane.org/
- 76.Vasukutty N., Jawalkar H., Anugraha A., Chekuri R., Ahluwalia R., Kavarthapu V. Correction of ankle and hind foot deformity in Charcot neuroarthropathy using a retrograde hind foot nail—the Kings’ Experience. Foot Ankle Surg. 2018;24:406–410. doi: 10.1016/j.fas.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 77.Wukich D.K., Raspovic K.M., Suder N.C. Patients with diabetic foot disease fear major lower-extremity amputation more than death. Foot Ankle Spec. 2018 Feb;11(1):17–21. doi: 10.1177/1938640017694722. [DOI] [PubMed] [Google Scholar]
- 78.Chraim M, Orthopaedic Hospital, Speising, Vienna, Austris Mid-term follow-up of patients withhindfoot arthrodesis with retrogradecompression intramedullary nail in Charcotneuroarthropathy of the hindfoot. BJJ. 2018;100–B:190–196. doi: 10.1302/0301-620X.100B2.BJJ-2017-0374.R2. [DOI] [PubMed] [Google Scholar]